Coronavirus Today: Are there consequences for failing to mask up?
Good evening. I’m Karen Kaplan with an assist from Corinne Purtill, and it’s Tuesday, May 10. Here’s the latest on what’s happening with the coronavirus in California and beyond.
“To Protect and to Serve.” Those words appear on every black-and-white patrol car driven by officers of the Los Angeles Police Department.
The pandemic added a new layer of risk to their already hazardous job. As first responders, they don’t have the luxury of holing up at home to stay out of the coronavirus’ way. Instead, they are out and about in the city, sometimes venturing into communities where infection rates are particularly high.
This is why law enforcement officers were high on the priority list when COVID-19 vaccines first became available. It wasn’t just a show of appreciation. It was intended to assure members of the public that if they interacted with a police officer, he or she had taken precautions to keep the virus from spreading. (The public might want that reassurance — as of late April, more than 44% of the LAPD’s employees had been infected at some point during the pandemic.)
As we’ve discussed, this wasn’t an opportunity all officers were eager to embrace. Six months into the state’s vaccination campaign, only 52% of LAPD personnel were at least partially vaccinated against COVID-19. That was well below the overall rate for California adults at that time — 72%.
Even today, 20% of the LAPD’s workforce remains unvaccinated. No matter how high the death toll has climbed (the United States is on the verge of hitting the 1-million mark) and no matter how many doses have been administered (nearly 580 million in this country alone), some people are just not down with the idea of giving their immune systems a coronavirus-fighting cheat sheet in the form of a shot.
But vaccines aren’t the only prevention tool. Since 2020, the LAPD has required officers to wear masks at work and when they are face-to-face with members of the public.
The Police Department said its mandate wasn’t just for show. Those who failed to comply would be held accountable, officials promised. But that doesn’t seem to be happening, my colleague Kevin Rector reports.
The LAPD received 268 mask complaints in 2020 and 2021. Guess how many of those complaints resulted in formal punishment?
Two. That’s an average of one per year.
The figures come courtesy of the LAPD’s Professional Standards Bureau. Its reports don’t describe the circumstances of the complaints, so we don’t know how many officers were involved, or how many times their masking habits were found wanting.
LAPD Chief Michel Moore said the two cases involved “repeat failures” to abide by the mask mandate. The punishments included reprimands and suspensions, he added.
What about the other 266 cases?

Before we get to that, let’s note that many of those complaints involved more than one officer. Let’s also note that there may be additional allegations of lax mask use by officers that are contained within more serious complaints. Plus, officials acknowledged that internal investigators might have discovered other mask scofflaws on their own.
As for the cases we do know about, dozens were handled through a “non-disciplinary” process that allowed officers to avoid punishment. They didn’t get a “reprimand” or an “admonishment.” What they got instead was a ruling that their “actions could have been different.”
Some of those officers received a “Notice to Correct Deficiency” or were told to get “counseling” about their mask use (or lack thereof). Either path would leave them without a “sustained” complaint on their records.
In a few dozen cases, there was “insufficient evidence” to determine whether a violation occurred. Investigators found “no misconduct” in at least 22 other cases.
Moore said the disciplinary responses were appropriate: The goal is to get maskless officers to change their behavior, he said, not to punish them.
That’s why first-time offenders were routed to counseling, which was documented in their personnel files, he said. When necessary, those who needed a refresher received training that reinforced the department’s expectations about the mask mandate.
Moore described the approach as “progressive discipline.”
William Gude called it a sham.
Gude is one of the LAPD’s chief critics. His Twitter handle is @FilmThePoliceLA, and he has used the account to post videos of unmasked officers, both on the street and inside police stations. Several of the 268 mask complaints originated with him.
The leniency shown toward maskless officers who are clearly guilty not only leaves their disobedience unpunished but also effectively condones it, Gude said.
“It’s really frustrating,” he told Rector. “It’s not done in the public interest.”
No matter how strongly health officials at all levels of government urge us to continue wearing masks, the number of Americans who follow that advice seems to be a shrinking by the day.
The LAPD still requires its officers to mask up in some indoor and detention settings. But in keeping with the national trend, the department no longer requires masks for all officers at all times.
By the numbers
California cases and deaths as of 5:05 p.m. Tuesday:

Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Yes, teens can get long COVID too
A lot of people, especially teens, have developed a cavalier attitude toward the coronavirus. Sure, their chances of becoming severely ill are lower.
But that doesn’t mean they’re bulletproof. About 13 million children have been infected during the pandemic, including 62,467 in the most recent reporting week, according to the American Academy of Pediatrics and the Children’s Hospital Assn.
If you need another good reason to try avoid getting sick, consider the case of Ami Korn.
He came down with COVID-19 in January 2021, right in the thick of the pandemic’s deadliest surge. He was a 13-year-old eighth-grader at the time who took honors classes and played baseball.
His illness started with a nagging headache and an earache. Then it got worse. A lot worse.
Ami suffered lung inflammation, body aches, nausea and dizziness, my colleague Emily Alpert Reyes reports. He became so fatigued that he slept 12 to 16 hours a day and labored to walk a full block from his Tarzana home. At one point, just shuffling from his bedroom to the kitchen caused his heart rate to spike.
As his symptoms dragged on, he wound up missing much of eighth grade. He also missed playing baseball and hanging out with his friends.
It took more than five months for his condition to start to improve. His gains didn’t come easily. He began a cardiopulmonary rehab program that included workouts on a treadmill and a stationary bike while machines tracked his heart rate and oxygen levels. His fellow rehab patients were in their 70s and 80s.
Ami got the Pfizer-BioNTech vaccine when it was authorized for younger teens. His father, Ze’ev Korn, said his son improved after getting the shot, something that’s been seen in older people with long COVID.
When he went back to school for ninth grade, it became clear that his recovery still had a very long way to go. He’s still grappling with brain fog, one of long COVID’s signature symptoms. It’s particularly frustrating to Ami because he used to have a great memory.
As Ami explained, he can learn about independent clauses in English class on a Monday, but two days later when the class proceeds to complex clauses, he’s forgotten what an independent clause is. In math, he can master a certain kind of problem one day, then struggle to solve it a few days later.

Anxiety over situations like those may have contributed to the panic attacks that have kept him from falling asleep. Another possible factor: seeing classmates blow off COVID-19 safety precautions. Ze’ev Korn told Alpert Reyes that a few students made a point of coughing on his son.
Things got so bad that the Korns moved from Tarzana to the Atlanta area so Ami could attend a school with better safety protocols. That helped with his anxiety, but he’s still working out what to do about his schoolwork. His parents cut back his schedule to just two classes, and Ami is planning to repeat ninth grade.
Ami’s mom, Linda Korn, said it had been difficult to explain the teen’s situation to others. “It’s not something you can see, like a broken arm or a broken foot,” she said. “It’s very hard for people to understand.”
Long COVID is still a mysterious condition for adults, and it’s even less well understood in children. Dr. Lawrence C. Kleinman, a pediatrician and professor at Rutgers Robert Wood Johnson Medical School in New Jersey, has a grant from the National Institutes of Health to study long COVID in kids. For now, he said, trying to advise parents about what their children are going through is “like fixing the engine while the plane is flying in the air.”
Imaging studies have turned up measurable changes in the brains of adults who have weathered coronavirus infections, even mild ones. It’s unclear what those changes might mean for teens, whose brains are still developing.
Even with so much still uncertain, Ami said he was grateful to have survived his bout with COVID-19. More than 1,500 American children and teens under 18 haven’t been as lucky.
“And I’m grateful that my brain is as well as it is,” he said, “even though I want it to be better.”
California’s vaccination progress
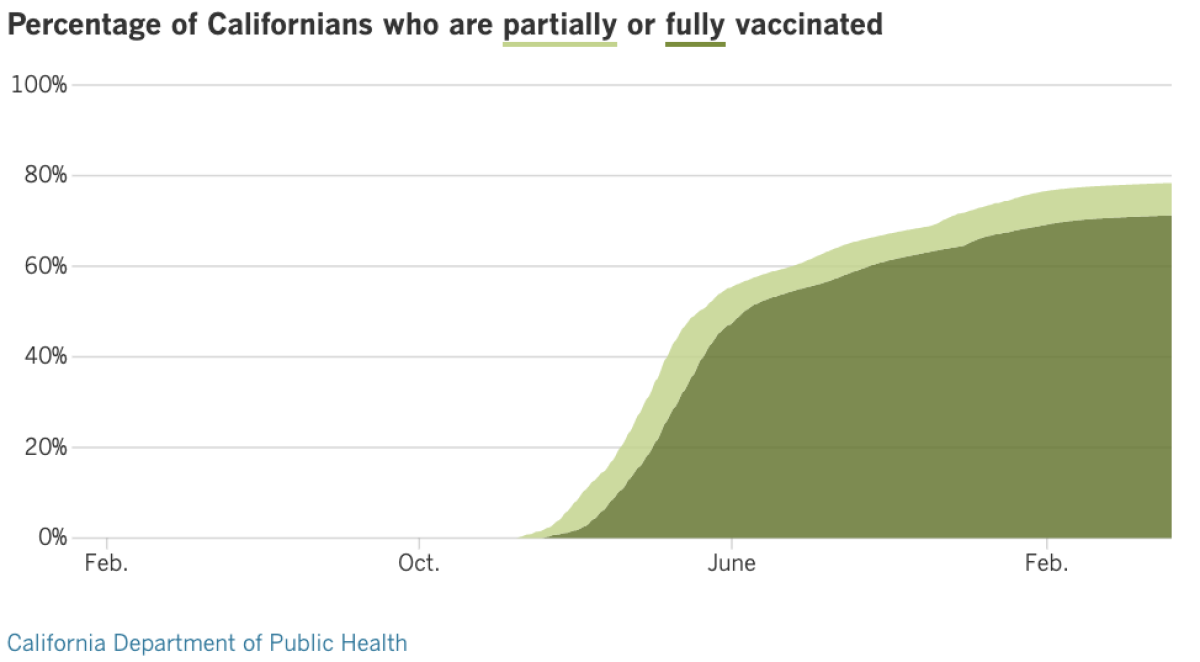
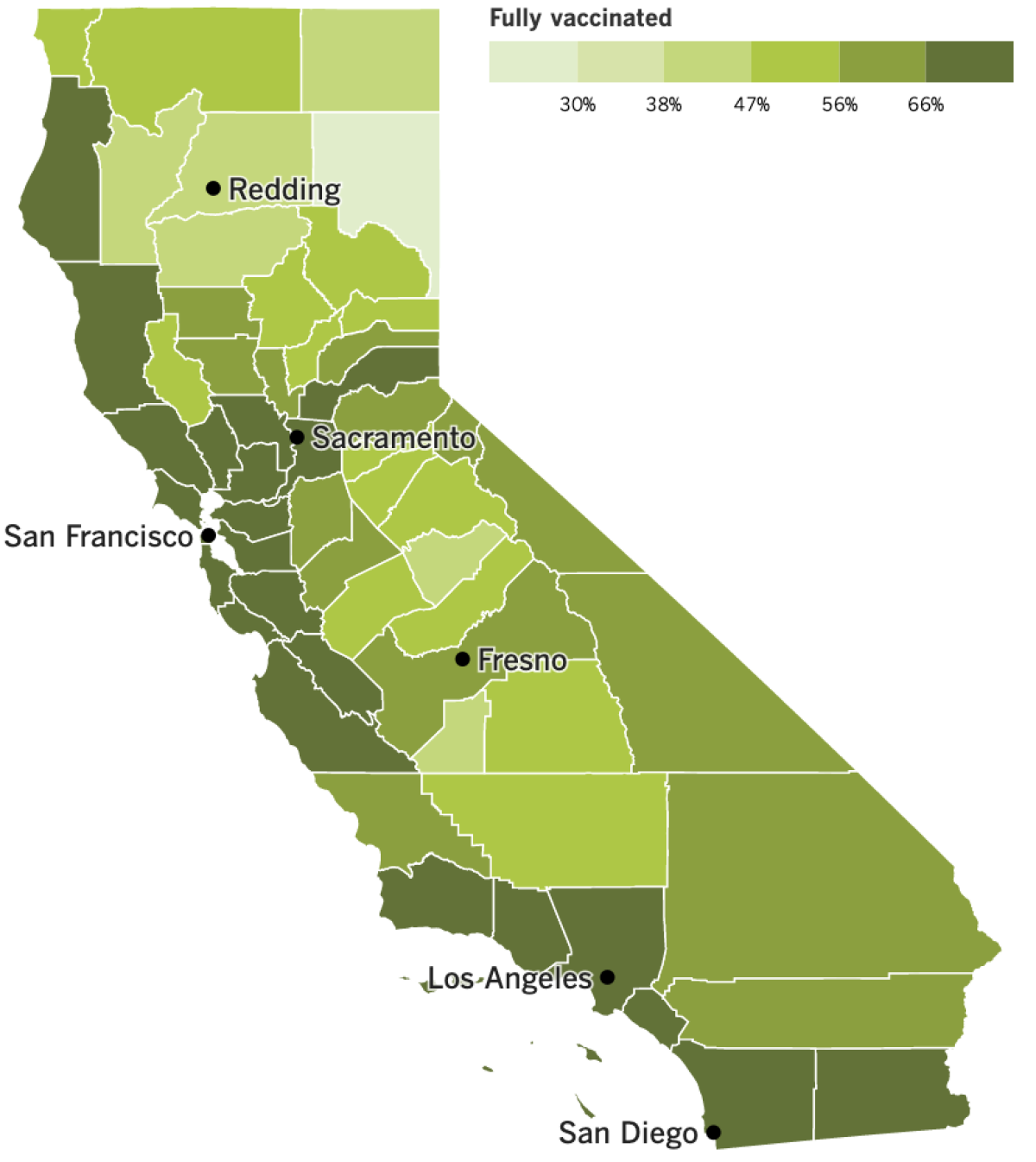
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
The past week has brought fresh evidence that the newest Omicron variants aren’t done with us yet. In Los Angeles County, officials are seeing more coronavirus outbreaks in schools and workplaces. It could mean some rules we’ve recently done away with will be back in the near future.
The number of outbreaks at schools and workplaces are now considered of “medium” concern under the county’s early alert system, our colleagues Rong-Gong Lin II and Luke Money report.
All told, 108 worksites reported new clusters of coronavirus cases in the last week, up from 82 the prior week. And if you’re a parent, you may have already noticed an unwelcome increase in alerts on confirmed infections in your child’s school.
County Public Health Director Barbara Ferrer told The Times that reported coronavirus cases among K-12 students and staff more than quadrupled in the last month. About 1,200 elementary school students and staff in L.A. County had a positive coronavirus test between April 18 and 24, up from 300 between March 21 and 27.
“There are now nearly as many cases among students and staff as there were in mid-February,” Ferrer said, an increase likely fueled in part by spring break travel.
Overall, the average number of new coronavirus infections being reported daily in L.A. County has risen 29% since last week — from 1,835 to 2,366.
California’s per capita rate of coronavirus-related deaths remains among the lowest in the U.S., according to a Times analysis. Among the 10 most populous states, California’s cumulative death rate is the lowest of all.
Yet as the most populous state in the nation, there’s no escaping the grim fact that even relatively low rates of infection have led to a stunning number of deaths. In the next few days, California is likely to record its 90,000th COVID-19 death — just as the U.S. approaches the sobering milestone of 1 million coronavirus-related deaths since the pandemic’s start.
Infections and deaths in the U.S. have been disproportionately concentrated among communities of color. A new poll shows that Black and Latino Americans remain far more concerned about COVID-19 safety than their white neighbors. Roughly 68% of Latino Americans and 63% of Black Americans say they are at least somewhat worried that they or a family member will become infected with the coronavirus, according to the poll from the Associated Press-NORC Center for Public Affairs Research. Only 45% of white Americans share that view.
Despite those concerns, and despite rising case counts, public officials seem to have little stomach for bringing back indoor mask mandates.
Many U.S. cities and regions with infection rates that in earlier pandemic times would have triggered mask mandates are no longer enforcing those rules, citing “pandemic fatigue.” (For what it’s worth, the CDC still urges people to mask up in indoor public places, regardless of vaccination status.)
The crumbling of mask mandates underscores the importance of vaccines, the safest and most effective means of preventing coronavirus transmission. State lawmakers are trying to make it easier for adolescents who want a shot to get one without their parents’ consent.
California already allows minors age 12 and older to receive vaccines against sexually transmitted diseases without parental approval. A bill that has cleared the state Senate Judiciary Committee would expand that permission to any vaccine that has been approved by the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention. If it passes, California will be the first state to allow children as young as 12 to obtain a coronavirus vaccine without parental consent.
While we’re in Sacramento, California State Controller Betty Yee is in hot water for her role in helping two political operatives secure a $600-million contract for their medical supply company in the chaotic early days of the pandemic. Yee, who had no formal role in the contract process, privately advised Blue Flame Medical LLC’s co-founder how to negotiate an advance payment and discouraged him from disclosing how much the company would pocket from the deal, Melody Gutierrez reports. The state is now embroiled in a lawsuit over the costs of undoing the misbegotten arrangement.
Blue Flame’s deal is one of three no-bid contracts for emergency supplies totaling $1.6 billion that the state handed out in the pandemic’s frantic first weeks. All later collapsed.
“No-bid contracts are subject to all kinds of problems,” political commentator and San Jose State professor emeritus Larry Gerston told Gutierrez. “They are subject to foolish things. You have to wonder how many things we don’t know about.”
Speaking of things we do know: The World Health Organization says that nearly 15 million people have died because of the COVID-19 pandemic, either from the virus itself or from being unable to seek healthcare for other conditions as a result of the crisis. That’s more than double the official 6 million global death toll. Most of those who died were in Southeast Asia, Europe and the Americas.
Since the start of the pandemic, China has officially reported only about 5,000 total deaths to the coronavirus, though the true number is believed to be far higher. The country has imposed strict lockdowns once again in recent weeks as a result of new outbreaks, and economists are questioning whether the country’s zero-tolerance coronavirus policy is worth the cost. The public is growing increasingly frustrated with strict quarantine measures, and some foreign companies are reconsidering their operations in the country.
China set a 5.5% gross domestic product growth target in March. Yet a study from the Chinese University of Hong Kong and Tsinghua University estimated that a one-month countrywide lockdown would reduce quarterly GDP by 22.3%, while a lockdown limited to China’s four largest cities — Beijing, Guangzhou, Shanghai and Shenzhen — would reduce the country’s GDP by 8.6%.
“The problem is that this thing can pop up at any time,” said Gene Ma, head of China research at the Institute of International Finance in Washington. “That’s what makes the situation so precarious.”
Your questions answered
Today’s question comes from readers who want to know: Is the Johnson & Johnson COVID-19 vaccine still an option in the U.S.?
Yes, but as of Thursday, it’s only recommended for a very limited group of Americans — those who had a severe allergic reaction to Comirnaty (the Pfizer-BioNTech vaccine) or Spikevax (the Moderna vaccine) and can’t take an mRNA vaccine again.
The Food and Drug Administration restricted use of J&J’s single-dose vaccine after reconsidering the risk of developing life-threatening blood clots within two weeks of getting a shot. Scientists identified 60 cases as of mid-March, which worked out to one case per 3.23 million shots administered. Nine of those cases were fatal.
Going forward, the J&J vaccine will come with a stronger warning about the potential “long-term and debilitating health consequences” of the blood clots.
For months now, the CDC has recommended the mRNA shots over the J&J vaccine because of the safety risks. All three vaccines are effective, but Comirnaty and Spikevax have consistently performed better.
The FDA’s new instructions still allow people who request the J&J shot to get it if they would otherwise skip vaccination altogether.
The vaccine “still has a role in the current pandemic response in the United States and across the global community,” said Dr. Peter Marks, the FDA’s vaccine chief.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The child in the photo above is Allan Fernandez. He made that funny face after getting a dose of COVID-19 vaccine at Ted Watkins Memorial Park in South L.A.
Then he turned around and high-fived the woman behind him — Dr. Rochelle Walensky, the director of the Centers for Disease Control and Prevention.
Walensky stopped by the vaccination site Thursday afternoon during her first official visit to Los Angeles as the nation’s top public health official. She acknowledged the challenge of finding new people to vaccinate, since most folks who were eager to get a shot have already done so. Persuading those who are hesitant to go ahead and roll up their sleeves will require persistence and patience.
“People have frequently asked me, ‘How do you convince somebody to get vaccinated?’” she said. “And the answer is, you stop talking and you listen.”
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.





