Coronavirus Today: Our final edition
Good evening. I’m Karen Kaplan, and it’s Tuesday, March 28. Here’s the latest on what’s happening with the coronavirus in California and beyond.
When the inaugural issue of this newsletter went out on March 5, 2020, California, Los Angeles County and the city of Los Angeles were all wrapping up their first full day of living under coronavirus-induced states of emergency. At the time, one person in California had died of COVID-19 after taking a cruise to Mexico and a second such death was suspected but not confirmed. It would take seven more weeks to learn that the state’s — and the country’s — first COVID-19 victim had actually passed away in early February.
Things went from bad to worse to disastrous in no time flat. For many of us, the true scope of the threat began to sink in on March 19, when Gov. Gavin Newsom went way out on a limb and ordered 40 million Californians to stay home to keep hospitals from becoming overwhelmed with COVID-19 patients. (There were limited exceptions for essential activities.) Overnight, the most populous county in the nation became a ghost town.
Looking back, it’s hard to believe so many people were willing to go to such great lengths for the sake of public health at a time when L.A. County’s new cases numbered in the dozens each day. But there’s no fear quite like the fear of the unknown — and there were certainly plenty of unknowns three years ago.

These days the situation is essentially the reverse. On Friday, the county reported 932 newly confirmed cases and 10 COVID-19 deaths, yet the public barely blinks an eye.
People like to think COVID-19 is just part of the landscape now, like the flu. But there’s a big difference: L.A. County has tallied 66 influenza deaths since the start of flu season in early October. During the same time period, 2,010 county residents have died of COVID-19.
It’s unclear how long it may take for COVID-19 to become no worse than the flu. Compared to the original version of the coronavirus, the Omicron variants are more transmissible but appear to be less dangerous. (It’s hard to be certain whether the reduced rates of severe illness and death in the Omicron era are due to the virus itself or the fact that we’ve got more immunity and better treatments.) That’s the evolutionary course viruses often take, but there’s no guarantee SARS-CoV-2 will follow it.
Although COVID-19 is still with us, public health officials no longer require emergency powers to manage it. That’s why California and the city of Los Angeles ended their emergency declarations last month. L.A. County’s will come to an end Friday, and President Biden intends to wind down the federal emergencies on May 11.
Likewise, COVID-19 isn’t making as much news as it used to, which is why this is the final edition of Coronavirus Today. It doesn’t mean our coverage of the pandemic will end — we’ll continue to keep you informed about the next round of booster shots, new discoveries about long COVID, additional treatments that win the Food and Drug Administration’s blessing, efforts to address health disparities, and more.
You can find our latest COVID-19 stories collected here. You can also subscribe to the Health & Science newsletter (which comes out on Saturdays), Essential California (which publishes every day except Sunday) and Today’s Headlines (which is available every weekday).
Our archive of more than 375 reader questions, along with their answers, is available here. And if you find yourself testing positive for a coronavirus infection in the future, check out our updated guide on what you should do to recover while keeping those around you safe.
Our COVID-19 tracker — possibly the single most useful thing The Times has ever produced — will be retooled in the coming months. It relies on information published by the Centers for Disease Control and Prevention, the California Department of Public Health and other government agencies, but new data is being released less often than it used to be.
My colleagues in the data and graphics department want to know what kind of COVID-19 information you’d like to have easy access to going forward. Please give them a hand by taking their survey here. Your answers will help shape the next version of the tracker, which should debut in June.
My byline has been on Coronavirus Today for nearly two years, but it takes a small village to produce it. I’d like to acknowledge the members of the newsletter team (past and present) who turned these words and pictures into email dispatches, including Sam Schulz, Scott Sandell, Amy Hubbard, Elvia Limón and Karim Doumar. The original full-time writer was Diya Chacko, and after she moved on, Deborah Netburn, Amina Khan, Soumya Karlamangla, Thuc Nhi Nguyen, Lila Seidman, Faith E. Pinho and Kiera Feldman took turns at the helm (and put up with my editing). A sincere thanks to you all.
My biggest thanks goes to the many readers who reached out over the years to tell us you appreciated the information we provided. Knowing you relied on these emails and looked forward to receiving them made the writing so much more worthwhile.
By the numbers
California cases and deaths as of 3:55 p.m. on Tuesday:
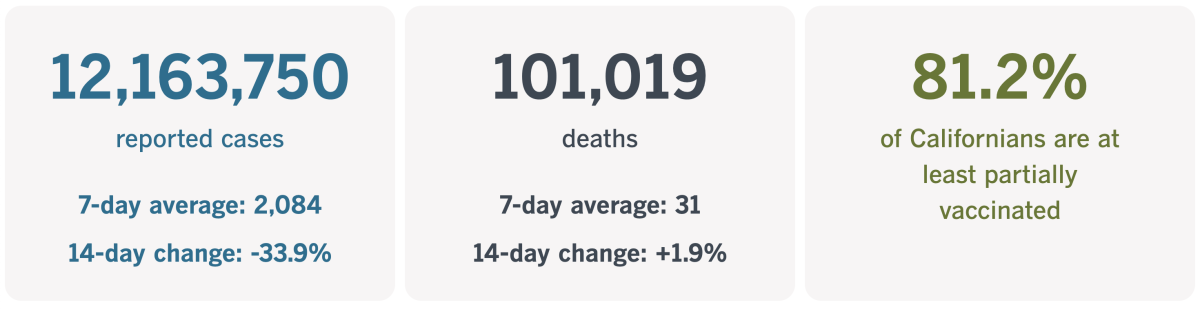
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Recognition for a pandemic heroine
While we’re feeling nostalgic, let’s think back to the days when we were learning to sew our own face masks (or making them out of old socks or T-shirts).
Homemade masks were necessary because demand for the real things had suddenly outstripped supply. Any bona fide face coverings that could be found were prioritized for doctors, nurses and other frontline workers, who were grappling with shortages as well.
Performance artist Kristina Wong looked around her Koreatown apartment. She had a Hello Kitty sewing machine, which she used to create sets and props. She had fabric and some elastic.
And she had an idea.
On March 20, 2020, Wong posted a photo of herself on Facebook wearing a rudimentary cloth mask. The caption read, in part, “If you are immunocompromised with no access to masks, I can mail you one if you don’t mind really messy stitching.”
With requests pouring in, she recruited friends — and later strangers — to help. The Auntie Sewing Squad was born.
Over 504 days, more than 800 volunteer sewers in 33 states created 350,000 masks. Those masks went to people in underserved communities, including Native Americans living on reservations, farmworkers, people in jail and migrants at the border seeking asylum in the U.S.
As word of the Auntie Sewing Squad spread, donations poured in. Some of the funds were spent on mask-making supplies and postage. Some were used to purchase essentials for mask recipients, such as diapers and detergent.
“I’m suddenly feeling the weight of saving the entire world with a sewing machine,” Wong recalled in a recent conversation with my colleague Jessica Gelt.
It was not what she expected. But then something even more far-fetched happened: She turned the story of the Auntie Sewing Squad into an acclaimed one-woman show.
It began as short bits performed on Zoom. In September 2021, a month after the Squad disbanded, she was invited by New York Theatre Workshop to turn it into their first post-shutdown production. “Kristina Wong, Sweatshop Overlord” premiered there on Oct. 25, 2021.
The play was a rare piece of art about the pandemic, and it came along as the pandemic was still going strong — its run began at the tail end of the Delta wave and ended as Omicron began to surge.
“Every single human being on this planet was impacted by it,” Wong said. “And it’s just so strange that there isn’t any work on it. I think there is this expectation that all the reflections are going to be really depressing and overwrought and sad.”
But hers is not. With wit and humor, the show tackles “life and death, class and privilege, the harm done to Black, Native and Asian Americans during the pandemic and how humanity’s mutual peril drove a wedge between us rather than binding us together with love,” as Gelt put it. (One of Wong’s costumes includes a cross-body ammo belt studded with colorful spools of thread, and she wields thread snips instead of a gun.)

“It doesn’t matter if I’m third-generation Chinese American,” Wong says during the play. She points to her face and explains, “This is a mask I can’t take off. It already tells people that maybe I’m an immigrant from the monolith that is Asia. Maybe I don’t speak English. Maybe I’m the one who brought the virus here.”
The Pulitzer Board was impressed. It named “Sweatshop Overlord” a finalist in the Drama category last year.
The Doris Duke Foundation was impressed as well. In February, it honored Wong with a Doris Duke Artist Award, which includes a $550,000 prize.
When the play came to the Kirk Douglas Theatre in Culver City this year, our theater critic Charles McNulty saw why it was so beloved.
“Sweatshop Overlord” was “the pandemic debriefing I didn’t know how badly I needed,” he wrote in his review. “This sanity-boosting recap of a horrendously difficult period is just what the doctor ordered.”
Though the production closed a couple of weeks ago, it stays with those who’ve seen it.
“The big feedback I get is, ‘Wow, I didn’t realize how much we just never stopped to process and remember,’ and ‘I can’t believe we lived through all that’,” Wong said. “But I remember. I was writing it all down. And I’m glad I did.”
California’s vaccination progress
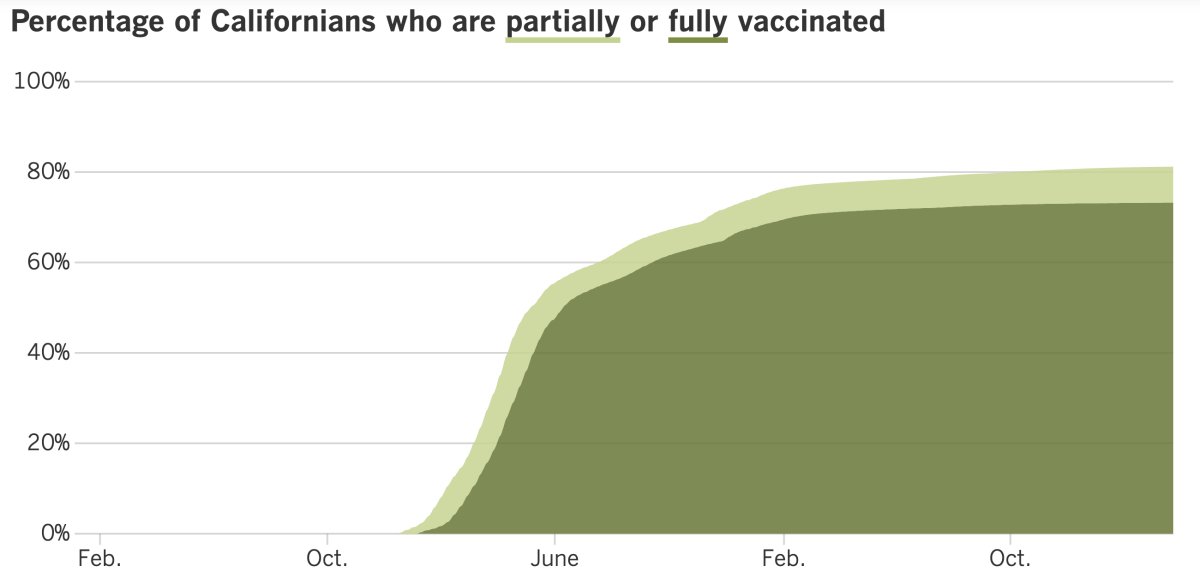
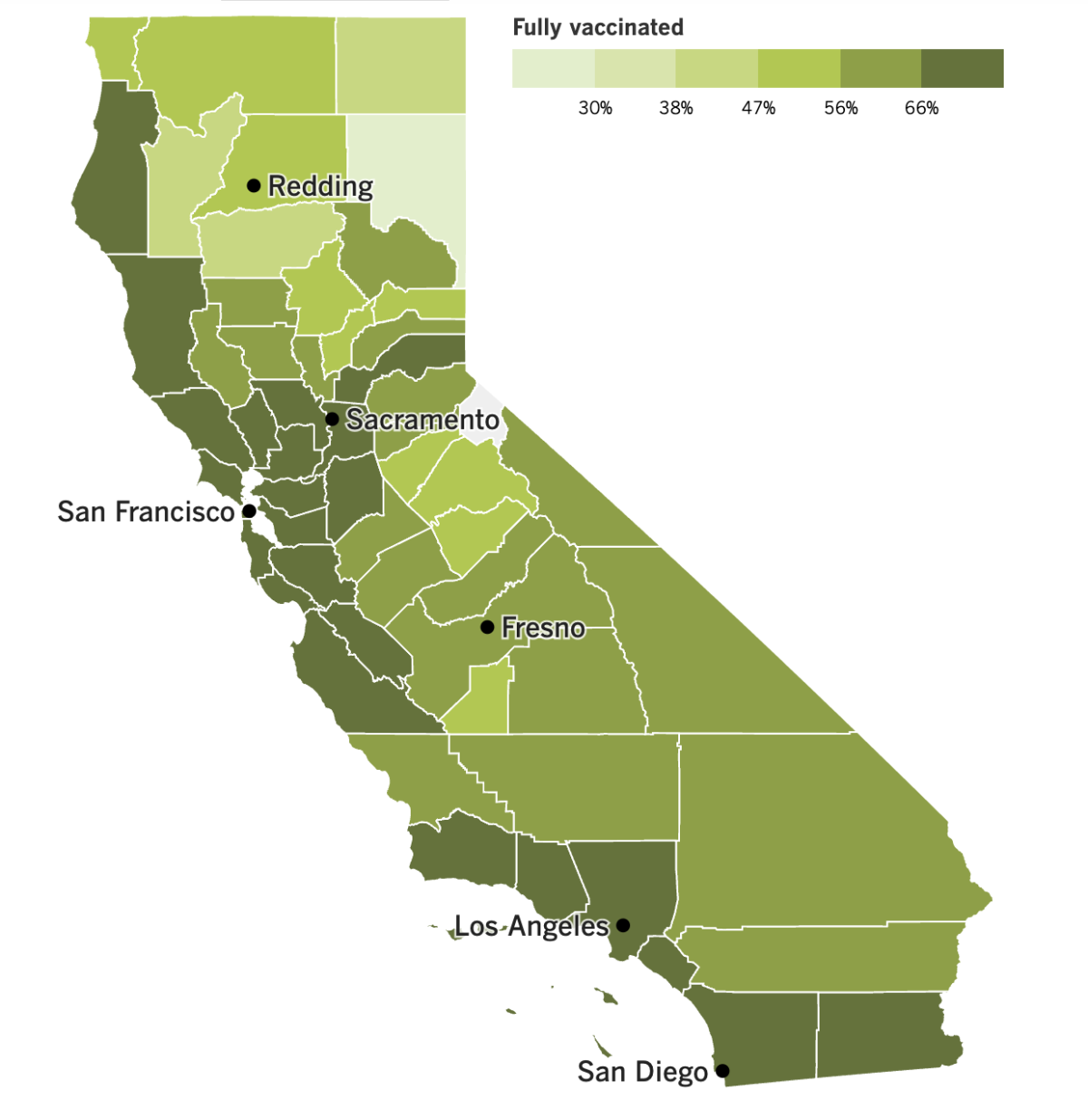
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
Way to go out on a high note, California! The entire state is currently colored green on the CDC’s map of COVID-19 Community Levels. That means every single county is in the coveted “low” category.
The official number of new infections fell week-to-week in Los Angeles, Orange, Riverside, San Bernardino, Ventura, Santa Barbara, San Diego and Imperial counties, the CDC said. L.A. County had the highest COVID-19 mortality rate in Southern California, at 0.8 deaths per 100,000 residents per week.
The coronavirus may be in retreat, but other threats are rising. One of them is a dangerous, drug-resistant yeast called Candida auris, or C. auris.
First detected in 2016, it has spread to more than half of U.S. states and likely got a boost from the pandemic since it mainly spreads in healthcare facilities that are sloppy with infection control, according to the CDC. In the last year, Nevada saw the most clinical cases (384) followed by California (359).
C. auris isn’t usually a problem for healthy people, but it can cause severe illness in hospitalized patients. The CDC estimates that infections are fatal 30% to 60% of the time, though it notes that patients often have other illnesses that make it more difficult for them to recover.
The CDC’s National Center for Health Statistics reported that maternal deaths have spiked during the pandemic. In 2019, a total of 754 pregnant women died in the United States. That figure rose 14% to 861 deaths in 2020, then increased another 40% to 1,205 in 2021.
The report released last week didn’t specify the exact causes of these maternal deaths. However, another recent report from the federal Government Accountability Office said COVID-19 played in a role in 1 in 4 maternal deaths in 2020 and 2021. A likely factor was the lower vaccination rates among pregnant women.
Speaking of COVID-19 vaccines, the 5th U.S. Circuit Court of Appeals has blocked President Biden’s vaccination mandate for federal employees. The court rejected the administration’s argument that just as CEOs of private firms could require workers to get the COVID-19 shots, so too could Biden require them of the federal workforce.
The 10-6 ruling was issued last week by the full appeals court, reversing a decision made by a three-judge panel. Nothing changes on a practical level, since a preliminary injunction has blocked the implementation of the vaccination mandate since January 2022. The case now returns to the lower court, where “both sides will have to grapple with the White House’s announcement that the COVID emergency will finally end on May 11, 2023,” the ruling said.
In other news, a new poll from the Pew Research Center found that the proportion of American adults attending religious services in person has dropped slightly since the start of the pandemic, from 33% in 2019 to 30% in 2022. However, when virtual services were factored in, the proportion held “remarkably steady” at about 40%.
Thomas Groome, a professor of theology and religious education at Boston College, said in-person attendance will “probably never come back to where it was before the pandemic,” but that’s not necessarily a cause for concern.
“I think people learned how to nurture their spiritual lives and faith without necessarily going to their local church every Sunday,” he added. “I know some of them went there virtually by Zoom. ... Many read the Scriptures themselves or they got together with neighbors or they bonded into family groups.”
Churches aren’t the only thing Americans have stayed away from — college falls into that category too. Across the country, undergraduate enrollment has dropped 8% since 2019, according to data from the National Student Clearinghouse. The declines continued even after colleges welcomed students back to campus.
The high cost of tuition and prospect of student debt are certainly factors, though not the only ones. For many young adults, an underwhelming experience with remote learning in high school made the prospect of further education unappealing. At the same time, it gave them the tools they needed to see their future paths differently.
“There were a lot of us with the pandemic, we kind of had a do-it-yourself kind of attitude of like, ‘Oh — I can figure this out,’” said Grayson Hart, who declined his college admissions offers in favor of directing a youth theater program in Tennessee. “Why do I want to put in all the money to get a piece of paper that really isn’t going to help with what I’m doing right now?”
Economists fret that it may be the start of a trend with dire consequences. In the short term, it certainly won’t help with the current labor shortage. And in the longer term, those who skip college usually make significantly less money over their lifetimes.
And finally, a study that compared the COVID-19 mortality rates of U.S. states found that the rate was nearly four times higher in the worst state than in the best state.
Arizona had the highest cumulative mortality rate through July 2022, with 581 COVID-19 deaths per 100,000 residents. At the other end of the spectrum was Hawaii, which saw 147 COVID-19 deaths per 100,000 residents. Both figures were adjusted to account for demographic differences between states, including the age and health status of the population.
Not surprisingly, states with higher proportions of Black and Latino residents, more people living in poverty, lower levels of education and more people without health insurance had higher COVID-19 mortality rates. On the flip side, the greater a state’s number of “vaccinated person days” (a term that measured how much of the population was immunized against COVID-19, and for how long), the lower the mortality rate.
The researchers also identified another protective factor: high levels of “interpersonal trust.”
“How we feel about one another matters,” said political scientist Thomas J. Bollyke, one of the study’s lead authors. “The solidarity between people — the feeling that others will also do the right thing, that you’re not being taking advantage of — is a big driver in your willingness to adopt protective behaviors.”
It’s another way of saying America’s growing divisiveness hasn’t served us well during the pandemic. Interpersonal trust has been declining for three decades, leading to the kind of us-versus-them mentality that fueled debates over mask and vaccine mandates. (Those, by the way, were also associated with lower COVID-19 mortality rates.)
As of this month, the United States has suffered more COVID-19 deaths per capita than any other high-income country, according to Johns Hopkins University.
Your questions answered
Today’s question comes from readers who want to know: Can a sinus rinse (like a neti pot) help flush out the coronavirus in an infected person?
It would stand to reason that the answer is yes, said Dr. Elizabeth Ko, an internal medicine physician at UCLA. The SARS-CoV-2 virus spreads primarily through the air, and its primary means of entry into the body is through the nose. Cleansing the nasal cavity seems like a plausible way to reduce the amount of coronavirus available to establish an infection.
Data from small clinical trials suggest that nasal irrigation may help COVID-19 patients after their infections have taken hold. One trial found that patients who were randomly assigned to use sinus rinses twice a day got over their congestion and headaches more quickly than patients who didn’t. They also reported feeling better about four days sooner than their non-rinsing counterparts, according to a report in the International Forum of Allergy & Rhinology.
Another study in the Ear, Nose & Throat Journal found that high-risk patients who started using some kind of nasal irrigation after they became infected were hospitalized at rates eight times lower than the national average.
However, there are no definitive clinical trial results showing that nasal irrigation can prevent a coronavirus infection or lessen its severity, Ko said.
Wondering if your question has already been answered? Check out our archive here.
The pandemic in pictures

There are a lot of images from the pandemic that will stay with me. There’s the shot of hundreds of cars snaking through the Dodger Stadium parking lot to get drive-through coronavirus tests. There’s the picture of New York City nurse Sandra Lindsay receiving the country’s first FDA-authorized dose of the COVID-19 vaccine. And who could forget the goats that took over a locked-down town in Wales?
But to my mind, no single photo captures the pandemic’s peak surrealness better than the one above. It was taken by my colleague Carolyn Cole on March 20, 2020, the day after Newsom took the extraordinary step of ordering millions of Californians to stay home.
When I think back to those initial lockdown days, I sometimes wonder if we really did sing two rounds of “Happy Birthday” while washing our hands and if the toilet paper shortage really was as dire as I remember. Seeing downtown L.A.’s four-level freeway interchange almost entirely traffic-free — on a Friday, no less — was a sure sign that something truly unprecedented was going on.
That photo also reminds me of how far we’ve come in the past three years. I’ll never be happy to sit in traffic when merging from the Pasadena to the Hollywood freeway, but now I’ll have a new appreciation for the normalcy that it represents.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




