Coronavirus Today: The problem with the lab leak theory
Good evening. I’m Karen Kaplan, and it’s Tuesday, March 14. Happy Pi Day! Here’s the latest on what’s happening with the coronavirus in California and beyond.
There’s a phrase that’s gotten a lot of use during the pandemic, repeated by people who were skeptical of the new COVID-19 vaccines, of the need for public health precautions, or of scientifically sound studies that debunked beloved remedies like hydroxychloroquine and ivermectin.
“Do your own research.”
Usually, the people who say this are not biologists who study viruses and their origins. But Michael Worobey is the exception.
Worobey heads the Department of Ecology and Evolutionary Biology at the University of Arizona, and like many others, he was curious about the origins of the SARS-CoV-2 coronavirus. Claims that the virus escaped from a research lab at China’s Wuhan Institute of Virology may have been dismissed as politically motivated, but Worobey and 17 other scientific experts urged their colleagues to keep an open mind and not jump to the conclusion that an infected animal spread the virus to humans.
After all, “knowing how COVID-19 emerged is critical for informing global strategies to mitigate the risk of future outbreaks,” they wrote in a 2021 open letter in the journal Science. “We must take hypotheses about both natural and laboratory spillovers seriously until we have sufficient data.”
Then Worobey went out and got the data.
As he recounts in The Times, he thought a lab leak was “plausible” but less likely than a “zoonotic” scenario in which the virus jumped from an animal to a person — especially after a study in the journal Scientific Reports documented that wet markets in Wuhan sold animals known to carry coronaviruses similar to the one that causes COVID-19.
“A scientist’s job is to kick the tires of a hypothesis — to try to falsify it,” Worobey writes. “I tabled all my other research to try to falsify the hypothesis that the pandemic began at one of those markets, the Huanan Seafood Wholesale Market, where many of the earliest known COVID patients worked.”
Here’s how he did it:
First, he examined the genetic sequences of viruses that were being studied at the Wuhan lab by a scientist named Shi Zhengli. He saw that they were too distantly related to SARS-CoV-2 to be responsible for the outbreak.
Next, he considered whether the reason so many of the earliest COVID-19 cases had ties to the Huanan market was that Chinese investigators were focusing their attention there. That turned out not to be the case because authorities hadn’t been surveilling the market at the time. In fact, doctors figured out that many of their patients with the mysterious new type of pneumonia had ties to the market.

That was an important clue, Worobey explains. Wuhan has a population of about 11 million people, and only about 1,500 of them work at the Huanan market. Yet 10 of the 19 earliest COVID-19 patients had links to the market. With the help of others, he mapped the patients’ homes to see if some other location would emerge as a potential epicenter. The results actually strengthened the case for the market being the epicenter, since it provided a missing geographic link for patients who said they didn’t work or shop there.
Another piece of evidence came from tests of stalls conducted after Chinese authorities had closed the market. Evidence of the SARS-CoV-2 virus was more likely to turn up in stalls where live mammals or meat were sold. (Unfortunately, the animals themselves weren’t screened before they were removed.)
Worobey and his collaborators also looked at cellphone data to assess the traffic in and out of the Huanan market and compare it with other public venues like schools, restaurants and shopping malls. Some of those places had 100 times more people passing through, Worobey noted. Given that, the only realistic way for the Huanan market to be the epicenter of the outbreak was for it to be the spot where the virus emerged in the first place.
It probably did not once, but at least twice. This part of the sleuthing gets more complicated.
It turns out there were two distinct lineages of SARS-CoV-2 — known as A and B — and both had geographic links to the Huanan market. Worobey and the others figured this out before they knew of any physical evidence that lineage A had been detected there. But such evidence turned up in February 2022.
A deep dive into the evolutionary history of more than 700 early SARS-CoV-2 sequences revealed that both lineages were descended from variants that were circulating in mid-December 2019. That’s consistent with a scenario in which infected people were contained within a limited geographic area around the market.
All this leads Worobey to the conclusion that the pandemic almost certainly started with zoonotic transmission, not a lab leak. And instead of being a fluke, it may have been reasonably likely: If a virus with the properties of SARS-CoV-2 finds itself in a city the size of Wuhan, computer simulations suggest that “about a third of animal-to-human transmissions will result in an epidemic,” he writes.
It remains unclear why the Department of Energy recently came to the conclusion — albeit with “low confidence” — that the pandemic began with a lab leak. If it’s that no one has been able to identify an animal that harbored the virus, that can be explained by the fact that the market was closed before any such testing was done. If it seems like too much of a coincidence for the first COVID-19 cases to arise in a city that’s home to a virology lab that studies coronaviruses, Worobey will have you know that “the vast majority” of China’s biggest cities have labs doing that kind of work. (Beijing has four.)
“I remain open to any and all evidence supporting a laboratory origin of the pandemic,” Worobey says like a true scientist. “So far, we have no such evidence.”
By the numbers
California cases and deaths as of 5:28 p.m. on Tuesday:
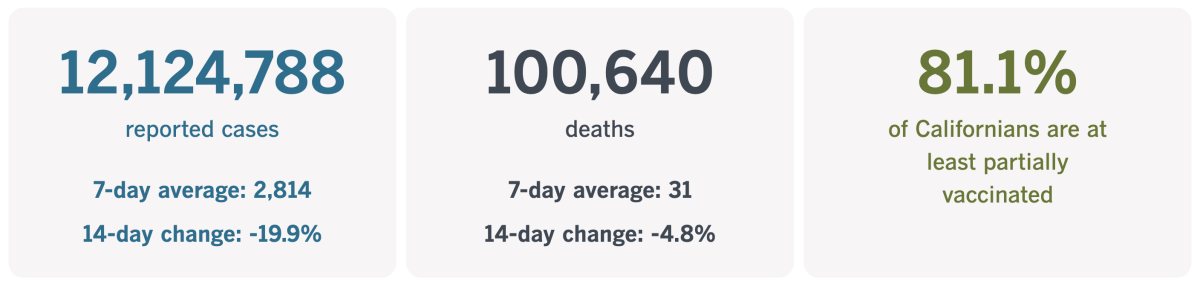
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
The power of promotoritos
Alma Gallegos’ family members didn’t want to get vaccinated against COVID-19 because they didn’t believe the disease was dangerous — until the death of a family friend prompted them to reconsider.
That’s when Gallegos, a senior at Theodore Roosevelt High School in southeast Fresno, seized her opportunity. Luckily for them, she is a promotorito.
In Latino communities, a promotora is an unlicensed but trusted health worker who encourages people to prioritize their health and helps people find the medical resources they need. In Fresno County, promotoritos are junior community health workers tasked with reducing the spread of COVID-19 through education and outreach.
Gallegos addressed her relatives’ misgivings with facts. Ultimately, she persuaded them to get the shots.
“My family is all vaccinated now,” she said, “but we learned the hard way.”
Along with 34 other students, Gallegos learned how to talk about COVID-19 vaccines in a way that would assuage people’s fears and motivate them to stay up to date with their booster shots. She told Heidi de Marco at Kaiser Health News that she joined the program so that other families wouldn’t have to lose a loved one, like hers did.
Now she’s the go-to source for her classmates when they have questions about COVID-19. That’s the result officials envisioned when they designed the program for teens 16 and older.
“Teenagers communicate differently, and they get a great response,” Sandra Celedon, chief executive of Fresno Building Healthy Communities, told de Marco. “During outreach events, people naturally want to talk to the young person.”

This idea goes well beyond Fresno. Students elsewhere in California, as well as in Colorado, New Mexico and Michigan, are being trained to serve as COVID-19 vaccine educators through the Oakland-based FACES for the Future Coalition. In Florida, high schoolers who participate in the Health Information Project talk to peers about vaccine safety, among other health issues.
Adults are counting on teens to help make the shots seem less threatening and hopefully improve vaccination rates, especially for the new Omicron-targeting booster shot. Only 16.3% of Americans have received it since it came out in September, according to the Centers for Disease Control and Prevention.
The figure is even lower for Latino Americans, around 8.5%, the CDC says. Language barriers and a lack of exposure to reliable information are two reasons why, and teens like Alma can help on both fronts.
“It makes sense we should look to our youth as COVID educators for their peers and families,” said Dr. Tomás Magaña of UC San Francisco. “And when we’re talking about the Latino community, we have to think deeply and creatively about how to reach them.”
Alma and her fellow promotoritos received 20 hours of training and now earn school credit plus $16 an hour for their outreach work. That includes visiting local businesses to distribute coronavirus testing kits and answer questions about COVID-19.
“I think it’s good that they’re aware and not afraid to share their knowledge about COVID-19,” said restaurateur Chris Vang, who received a visit (and some test kits) from Alma and three of her compatriots. “I’m going to give these tests to whoever needs them — customers and employees.”
California’s vaccination progress
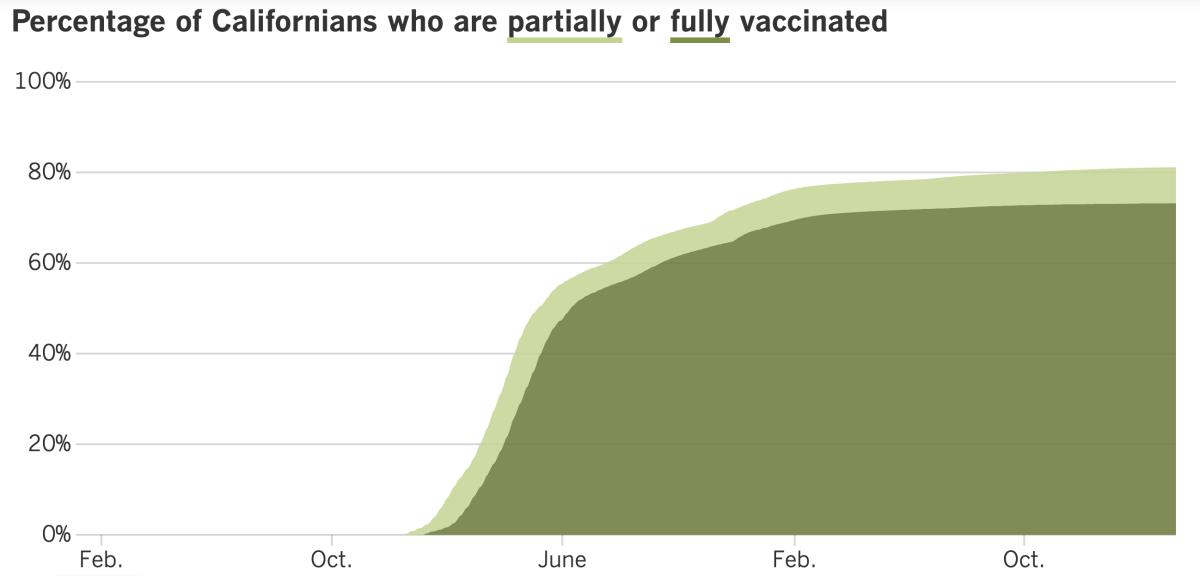
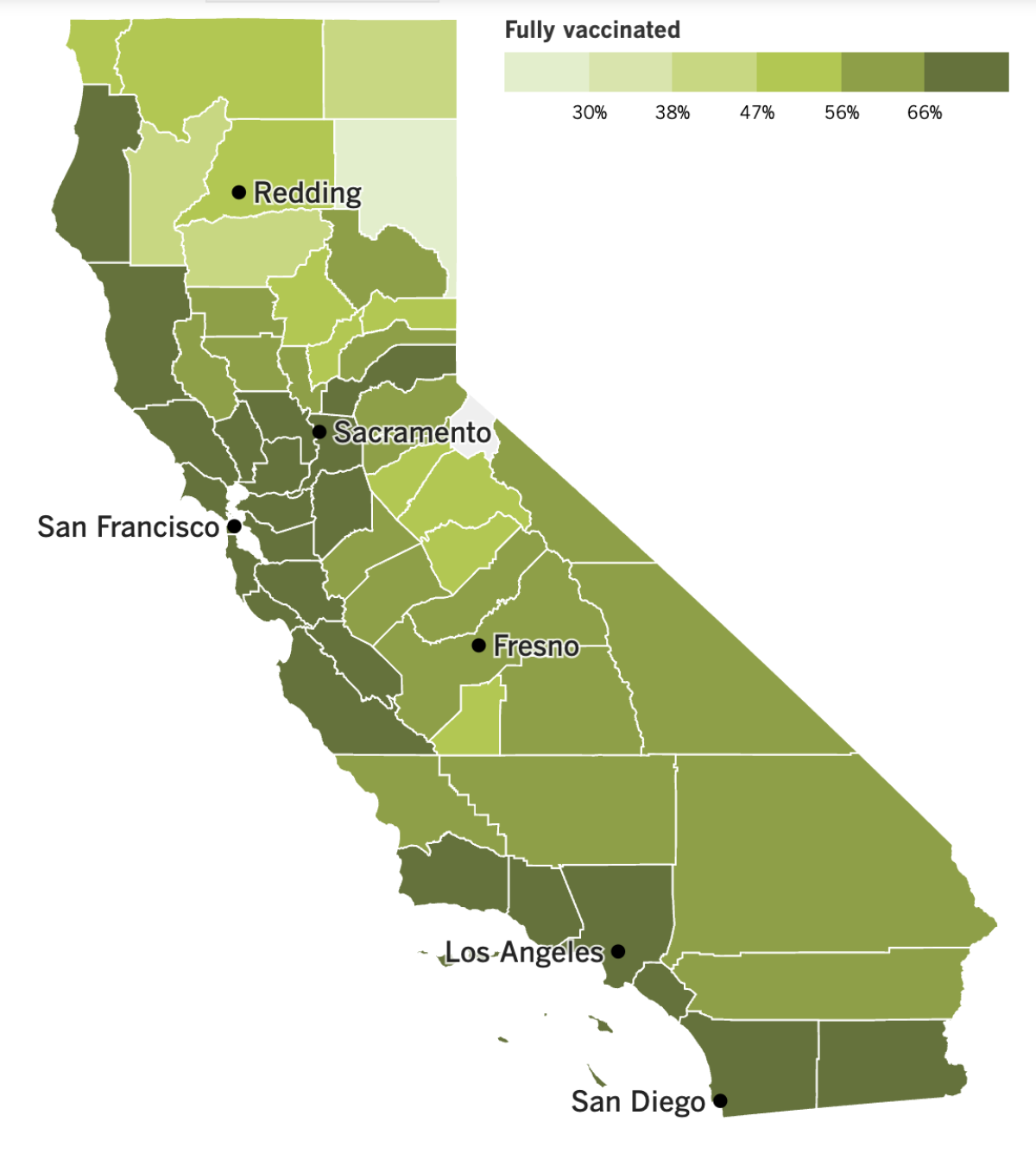
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
Saturday marked the three-year anniversary of the day the World Health Organization upgraded the COVID-19 outbreak to full pandemic status. It seems like a good moment to reflect on which side now has the upper hand — the coronavirus or us?
The virus is still killing more than 250 Americans each day, according to the CDC’s COVID Data Tracker, and the WHO’s Coronavirus (COVID-19) Dashboard indicates the global toll is several times higher. No one envisions a scenario in which the virus disappears, and as long as it keeps circulating, we could be just a few mutations away from a new variant that will erase our recent progress.
That said, humanity now has some hard-won immunity thanks to past infections and vaccines. That has made it possible for most people to return to a nearly normal way of life. (Unfortunately, immunocompromised people and others at high risk of becoming severely ill are becoming more vulnerable as pandemic precautions fall away.)
Dr. Stuart Campbell Ray prefers to look on the bright side. An infectious-disease expert at Johns Hopkins, he says that although the coronavirus has evolved to become more contagious, our collective immunity probably means that COVID-19 will never be as dangerous as it was in its first year.
But Dr. Eric Topol, head of Scripps Research Translational Institute in La Jolla, says the virus hasn’t given up — and neither should we.
“Whatever the virus is doing today, it’s still working on finding another winning path,” Topol said. “I wish we united against the enemy — the virus — instead of against each other.”
Long COVID is another reminder that 2023 is not the same as 2019. In a recent survey by USC’s COVID-19 Pandemic Research Center and the Los Angeles County Department of Public Health, more than half of county residents who came down with COVID-19 reported symptoms that persisted more than four weeks after they became infected.
The most common symptoms were extreme tiredness or fatigue, brain fog and a cough that won’t go away. Others included depression or anxiety, body aches, sleep problems, headaches, joint pain, breathing problems and the loss of taste or smell.
Perhaps the most troubling finding was that 77% of those with long COVID said their symptoms interfered with their ability to engage in routine activities like going to work, seeing friends and taking care of personal needs. About 25% of the long-haulers said they faced “significant limitations.”
“Most people with long COVID slowly begin to improve. However, there are also people who have had long COVID for many months, or even years, sometimes resulting in a disability,” said Barbara Ferrer, the health department’s director. She added that “no one’s immune to long COVID, even if you’re healthy and even if your infection is mild.”
Speaking of coronavirus infections, California Gov. Gavin Newsom has one for the second time. He tested positive Wednesday after he came down with mild COVID-19 symptoms and was able to keep working remotely (including firing up Zoom to announce a lawsuit against Huntington Beach over its ban on certain types of housing projects).
The governor aside, most of California is looking good on the CDC’s COVID-19 Community Level map. The number of counties in the “medium” category is down to nine, with Sacramento being the most populous among them. The rest of the state — including all of Southern California — is in the “low” zone. Los Angeles, Orange, San Diego, Riverside, San Bernardino, Ventura and Santa Barbara counties all saw their case rates fall in the last reporting week.
Remember that upscale nursing home on L.A.’s Westside where 13 residents and one nurse died during the early weeks of the pandemic? Three managers there were charged with 13 counts of elder abuse and five other charges on Tuesday. All of the charges are felonies.
The deaths occurred during an outbreak in March 2020 that began when Silverado Beverly Place admitted a patient from New York City, which was the country’s COVID-19 epicenter at the time. The nursing home’s policies said not to accept new patients from high-risk areas, yet the man was accepted without being tested for a coronavirus infection. He developed COVID-19 symptoms the next day and still wasn’t quarantined, prosecutors said.
By the time the virus had spread through the facility, 45 employees and 60 residents were infected. Silverado has already been sued in civil court. The company that manages the facility had no immediate comment on the criminal charges.
And finally, the pandemic has produced countless instances of partisanship, but last week it delivered the reverse. On Friday, members of the House of Representatives voted unanimously to declassify the U.S. intelligence community’s information about the origins of COVID-19. I’m not kidding — the vote was 419 to 0.
The bill had already passed the Senate by unanimous consent. It’s now up to President Biden to decide whether to sign it.
As mentioned earlier, the U.S. Department of Energy recently determined the pandemic virus escaped from a lab. The FBI previously came to the same conclusion, while other agencies disagree or remain undecided.
Whatever evidence they have ought to be shared with the public, said Sen. Josh Hawley (R-Mo.), who sponsored the bill. “The American people deserve to know the truth,” he said.
Rep. Jim Himes (D-Conn.), the highest-ranking Democrat on the Intelligence Committee, agreed, saying “transparency is the cornerstone of our democracy.”
Your questions answered
Today’s question comes from readers who want to know: Does it still make sense for my choir to have a vaccination requirement, especially if it only applies to the initial shots and not boosters?
To a certain extent, yes.
“Any immunity, either via vaccination or natural infection, is better than none,” said Dr. Edward Jones-Lopez, an infectious disease specialist with Keck Medicine of USC.
That said, if your choir plans to stick with its vaccination requirement, it might as well amend it to include the new bivalent booster, Jones-Lopez said.
The initial two-dose regimen of COVID-19 vaccines from Pfizer-BioNTech and Moderna did a great job of protecting people, but the more time that passes, the greater the need for the updated booster shots, he said. The coronavirus continues to evolve, and the Omicron subvariants in circulation today are quite different from the strain that the original vaccines taught the immune system to recognize. Plus, antibodies and certain other immune system cells wane over time.
“Booster shots are absolutely recommended,” Jones-Lopez said. “The best recommendations for any group meetings would be to be up to date on all vaccinations.”
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The photo above may look like a throwback to the pandemic’s early days, but it was taken this month. So if all those mask-wearing commuters seem like residents of a parallel universe ... well, you’re on the right track.
They’re in Tokyo, and their face coverings are notable because as of Monday, the Japanese government dropped its 3-year-old request for members of the public to mask up.
Commuters weren’t the only ones slow to take the government up on its offer. Fans with tickets to Monday’s World Baseball Classic games at the Tokyo Dome showed up with face coverings. Workers in shops, restaurants and airlines kept their masks on, even as they posted signs to let customers know they could remove theirs.
Japanese Prime Minister Fumio Kishida was maskless when he arrived for work, but several members of parliament donned face coverings for a televised budget committee meeting.
“From today, mask wearing is left up to individual judgment,” Kishida told reporters. “We are not forcing anyone to wear it or take it off.”
If the past is any guide, those masks are likely to remain in place for some time. The Japanese government told residents last summer that they could stop wearing masks outdoors, but they’re still a common sight.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




