Coronavirus Today: Experts are taking a softer stance on masking; it’s a different pandemic
Good evening. We’re Corinne Purtill and Karen Kaplan, and it’s Tuesday, Aug. 2. Here’s the latest on what’s happening with the coronavirus in California and beyond.
Perhaps nothing has come to symbolize this pandemic as succinctly as the humble face mask.
Be it pleated blue polypropylene, colorful fabric or the bulbous shell of an N95, it’s an accessory you probably never wore in public before the coronavirus arrived, and odds are you can’t wait to be rid of it.
In the early weeks of the COVID-19 era, when new infections were rising like crazy, we were asked to don face masks to “flatten the curve.” As schools began to welcome students back to campus, masks were an essential accessory to make communal learning safe. After scientists began to recognize that the coronavirus spread mainly through the air, masking was deemed necessary to protect those who were older or medically vulnerable.
Despite all these virtues, the mask has also been vilified as a symbol of unthinking obedience to authority and a tool to muzzle children and stifle dissent.
“It’s been a wordless signal of community resolve, and a noisy touchstone of struggle against government strictures,” our colleague Melissa Healy writes.
Even people who have worn them when asked over the last 2½ years are running out of patience for the face coverings. They haven’t made the coronavirus go away yet, and with each new variant more transmissible than the last, it seems unlikely they ever will.
Isn’t the definition of insanity doing the same thing over and over and expecting different results?

Regardless, Los Angeles County Public Health Director Barbara Ferrer had planned to reinstate L.A.’s indoor mask mandate if the county met the criteria set by the U.S. Centers for Disease Control and Prevention for having a “high” COVID-19 community level and maintained that status for two weeks. She later hinted that she might press pause on the unpopular mandate if there were “sustained decreases in cases, or the rate of hospital admissions moves closer to the threshold of medium.”
In the end, Ferrer didn’t have to decide whether to follow through with her original plan.
When the latest figures came out Thursday, the county’s level had dropped to “medium.” Using its own data, the county calculated new weekly coronavirus-positive hospital admissions as 9.7 for every 100,000 residents — just under the threshold to trigger the mask mandate. The CDC calculated a rate of 10.7, but Ferrer said the federal agency’s data were older than the county’s.
The news was celebrated by people like Michael Matteo Rossi. The 35-year-old filmmaker from Los Feliz wore his mask without complaint for more than two years. But even he’s hit his limit. He told Healy that his mask was lost somewhere in his car, and he hopes he doesn’t have to dig it out.
Fed-up folks like Rossi weren’t the only ones pleased that they could continue going about their lives mask-free. Some medical and public health professionals have softened their support for mask mandates as well.
The reason for their change of heart is not that masks (if used properly) have become less effective at preventing coronavirus transmission. It’s that the value of widespread masking just isn’t what it used to be.
That’s due to progress in other parts of the pandemic fight. With COVID-19 vaccines and past infections, the U.S. population has substantial coronavirus immunity. Those who get sick anyway have an array of effective treatments at their disposal. It also looks like infections caused by Omicron subvariants aren’t as dangerous as ones caused by earlier coronavirus strains.
Put that all together and the potential benefit of a mask mandate isn’t substantial enough to justify the inconvenience, public backlash and other costs that come with it, said Dr. Jeffrey Duchin, chief health officer of Seattle and King County.
“The threat has decreased,” Duchin said. “And for that reason, taking steps that are seen as inconvenient or costly or philosophically objectionable is less palatable and less desirable.”
Dr. Monica Gandhi, an infectious disease doctor who conducts public health research at UC San Francisco, agrees with that assessment — though she can understand why some health officials are still inclined toward mask mandates.
When new infections rise, “that feels scary to a public health officer,” she said, and a mask mandate “feels like something they can do.”
But just because you can do something doesn’t mean you should, she added.
“We’re in a very different place in the pandemic,” Gandhi said. “At this point, I do not think that widespread masking is necessary.”
By the numbers
California cases and deaths as of 4:20 p.m. Tuesday:
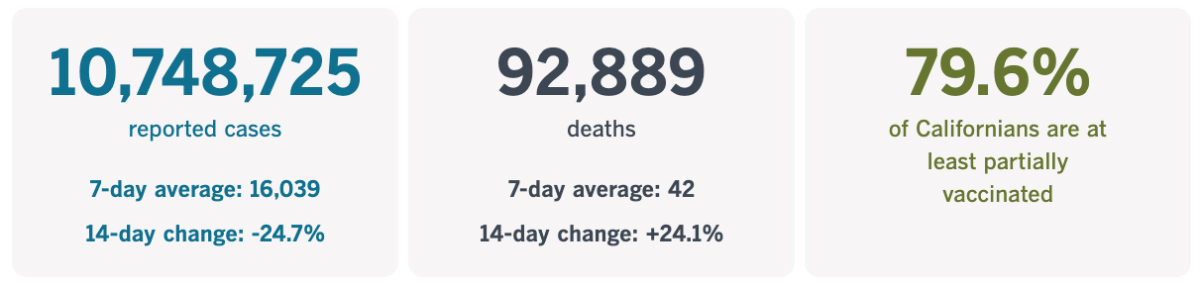
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Breathing easier indoors
Box fans, four high-quality filters and duct tape. Those are the components of a Corsi-Rosenthal box, an inexpensive DIY device that pulls coronavirus and other contaminants from indoor air as effectively as many commercial air filters do, at a fraction of the cost.
Researchers have found that changing the air in an indoor space just five times an hour can cut the risk of COVID transmission in half, The Times’ Emily Alpert Reyes reports. One study in Italy saw that benefit grow to an 80% reduction in COVID transmission in schools when indoor air was changed six times an hour.
Yet indoor air quality is often neglected. A June report from the U.S. Centers for Disease Control and Prevention found that most U.S. public schools had not made any major investments to improve indoor air quality since the pandemic began. When asked what steps they’d taken to improve ventilation in their classrooms, most schools reported simply opening windows or moving indoor activities outside. Fewer than 40% said they had replaced or upgraded their HVAC systems.
But there’s no need to wait until the next major capital improvement project to start cleaning up indoor air, engineers say. There’s no time, either.
“There are things we could be doing immediately and not waiting to spend millions of dollars to retrofit ventilation systems,” said UC Davis College of Engineering dean Richard L. Corsi, who helped develop the low-cost air filters that now bear his name.
It doesn’t help that the definition of “clean” indoor air is nebulous. There’s no federal standard or guidelines for what constitutes a well-ventilated room. The Environmental Protection Agency only has regulatory authority over the air we breathe outside buildings, not in them.
That has left many institutions to manage air on their own. In Los Angeles, the county Department of Public Health told Reyes it had connected schools with state grants to improve their ventilation systems and provided diagrams on the best places to put fans in school gyms. The county has also distributed HEPA air purifiers to more than 100 shelters for homeless people and other interim housing sites.
Some residents are taking the challenge up themselves. Reyes interviewed Alex LeVine, a cannabis company executive who has tricked out his own Studio City house with homemade air filters that pull contaminants from the air — and, in one case, pulse colored lights in time to Phil Collins’ ”In the Air Tonight.”
Who says filtration can’t be fun?
California’s vaccination progress
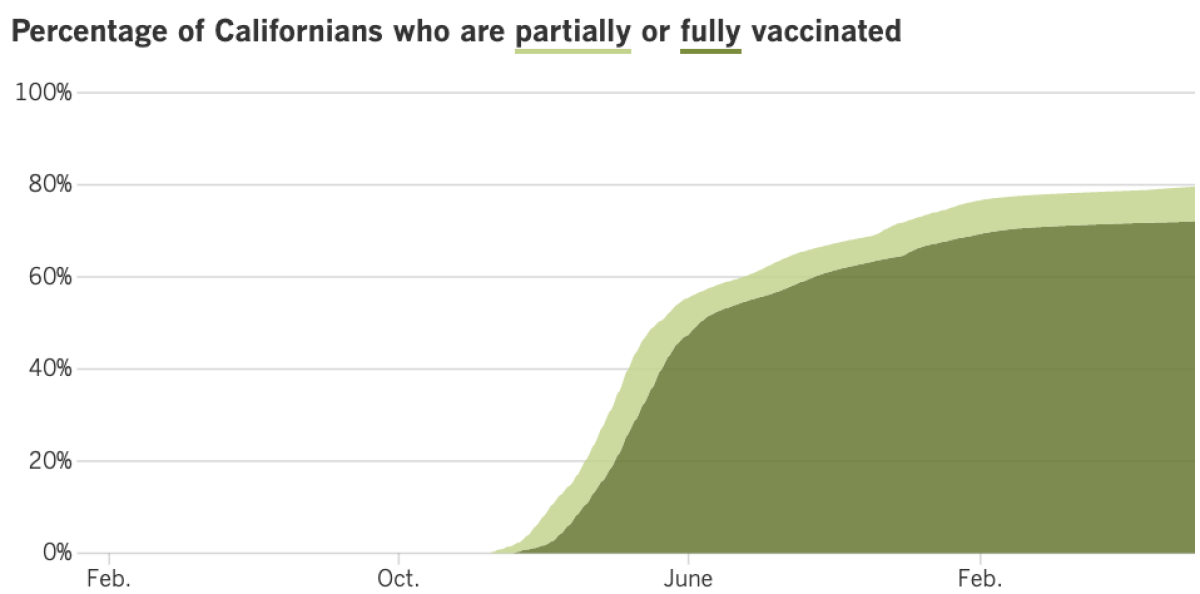
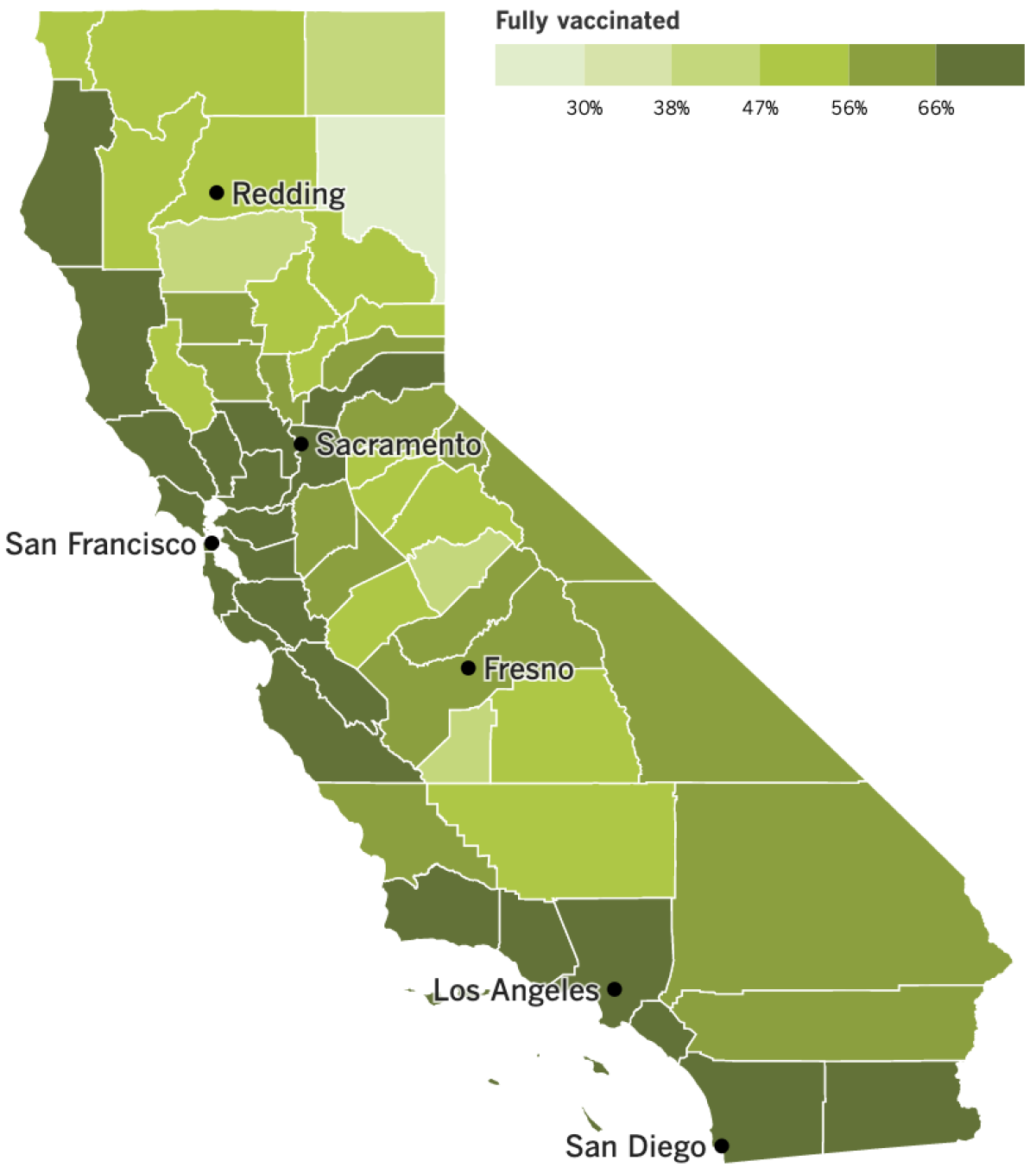
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
The hyper-transmissible Omicron variants have sent case numbers skyrocketing in recent months.
But health officials fear that they are also a harbinger of a devastating number of long COVID cases, our colleagues Rong-Gong Lin II and Luke Money report.
Thus far in the pandemic, infection with COVID has appeared to offer a grace period of protection against subsequent infections. But the most recent variants appear to have altered that timeline, speeding up the rate at which people can become reinfected. That’s particularly worrisome, as each individual infection carries the risk not only for acute illness but also the possibility of developing long COVID.
“Reinfection absolutely adds risk,” said Dr. Ziyad Al-Aly, clinical epidemiologist at Washington University in St. Louis and chief of research and development at the Veterans Affairs St. Louis Healthcare System.
Al-Aly is the lead author of a preprint study on U.S. veterans that found that the risk of developing heart or lung disease, blood clotting issues and other serious health problems — including death — rose with each subsequent infection.
“The additive risk is really not trivial, not insignificant,” Al-Aly said. “It’s really substantial.”
One of the most troubling risks of repeated infection is long COVID, in which symptoms persist for months or even years after the initial infection. Part of the maddening quality of the condition is that there are no clear indicators of who is most at risk. The condition has plagued people of all ages, including those whose initial COVID infections were mild or asymptomatic.
Its repercussions are already being felt in California. As Lin and Money have reported, an estimated 1 in 13 adults nationwide — and 1 in 14 in California — had current long COVID symptoms in early July, according to data collected by the Census Bureau and analyzed by the U.S. Centers for Disease Control and Prevention.
That study defined the condition as having symptoms lasting three months or longer that weren’t experienced prior to infection.
Dr. Anne Foster, vice president and chief clinical strategy officer for the University of California Health system, has a different name for it: a “mass disabling event.”
“The good news is that most long COVID will resolve, let’s say, after a year,” Foster said. “But there’s going to be some smaller subset that will have lifelong disability and impact to their health.”
A study from USC published last month found that 23% of people who had coronavirus infections between March 2020 and March 2021 were still reporting symptoms up to 12 weeks later.
The most common lingering symptoms reported in that study were headache, nasal congestion, abdominal pain, fatigue and diarrhea. But many long COVID sufferers describe severe ongoing heart, respiratory and neurological problems that in some cases have made it impossible to return to normal life.
Hannah Davis, a co-founder of the Patient-Led Research Collaborative, was diagnosed with COVID in March 2020 and still has “difficulty driving, reading and walking,” she told the U.S. House Select Subcommittee on the Coronavirus Crisis during a recent hearing.
Long COVID, she said, “has already impacted our workforce. Many people with long COVID can’t work or need reduced hours and struggle to apply for disability benefits. The financial impact is devastating and cannot be overstated.”
And finally: Just three days after testing negative and getting the all-clear to leave isolation, President Biden tested positive for the coronavirus once again on Saturday.
Biden, 79, first tested positive for the virus on July 21. He was treated with the antiviral drug Paxlovid, and was cleared to exit isolation July 27 after receiving negative tests. But “rebound” infections like Biden’s are not unheard of, particularly among patients treated with Paxlovid, an antiviral recommended for patients at risk of developing more severe disease. Most rebound cases don’t merit additional treatment, the CDC advised in May. The White House says Biden does not have further symptoms, and will resume working from home.
“I’m feeling fine, everything’s good,” Biden said in a video posted to Twitter, gesturing to his nearby dog. “Commander and I got a little work to do.”
Your questions answered
Today’s question comes from readers who want to know: Should I wait to get a booster until the one that targets Omicron comes out?
Considering how many people are becoming infected despite being fully vaccinated and even boosted, it’s no wonder this question keeps coming up. After all, the CDC estimates that 85.5% of the coronaviruses on the loose in the U.S. right now are of the BA.5 variety, and another 11.8% are BA.4 types. Those are the two subvariants that the new crop of boosters will be designed to recognize, along with the original coronavirus strain.
The Food and Drug Administration expects the updated shots to be ready this fall, but if you are eligible to get a booster right now, the advice of experts is unequivocal: Don’t wait.
“Definitely get it now!” Paula Cannon, a professor of molecular microbiology and immunology at USC’s Keck School of Medicine, told our colleague Jon Healey. The other vaccine experts he spoke to emphatically agreed with Cannon’s assessment.
Everyone who is at least 5 years old is eligible for one or two booster shots, depending on their age and the state of their immune system. Yet fewer than half of Americans who are booster-eligible have gotten even one extra shot, according to the CDC.
More than 17,600 Californians have been getting infected each day over the last week, including more than 5,600 per day in Los Angeles County alone. Those numbers are all the reason you need to get up to date on your vaccinations, said Dr. Otto Yang, an infectious diseases expert at UCLA’s David Geffen School of Medicine.
Here are two more: The booster you can get right away “remains extremely good at keeping people from getting extremely ill or dying,” he said. Plus, it’s not clear that the Omicron-specific shots will offer a huge advantage.
Data from the companies developing the shots show that targeted boosters were “only modestly better” than the current ones “in terms of antibody activity against Omicron,” Yang told Healey.
And who knows whether BA.5 and BA.4 will still be dominant by the time the new shots are ready?
“We could be looking at a completely new variant” by then, Cannon said. “So rather than trying to second-guess anything, we should stick with what we know, which is that boosters work well now, to top up people’s immunity.”
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures
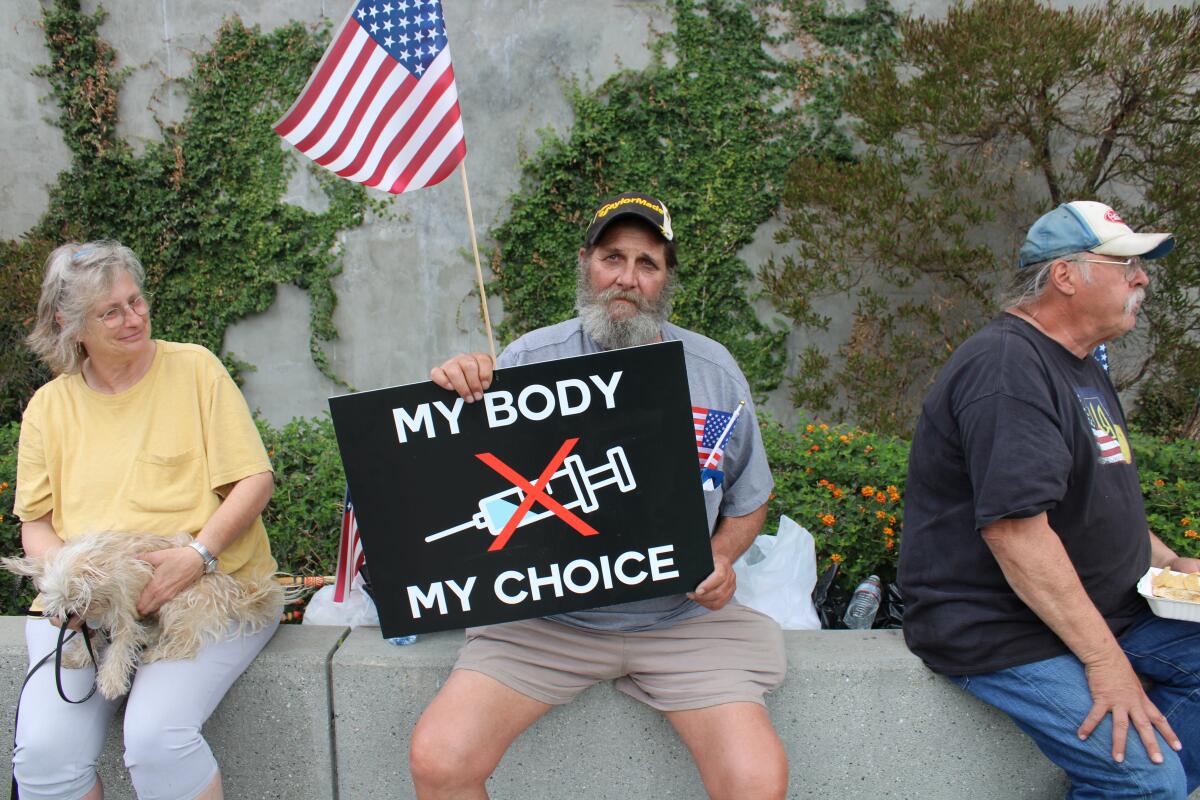
“My body, my choice.” For the last half a century, this slogan has been associated with the fight for abortion access. Yet since the outbreak of the pandemic, and the proliferation of public health measures to control the virus’ spread, this former rallying cry for reproductive rights has been increasingly co-opted by opponents of mask and vaccine mandates.
The sign above (carried by Steve Bova of Maryland) was one of many on display at an April anti-vaccine mandate rally in downtown Los Angeles. “Women say they can have an abortion because it’s their body,” said Tom Blodget, a retired Spanish-language teacher from Chico who wore a T-shirt bearing the slogan. Blodget opposes abortion, he said. But “if that’s a valid thing for a lot of people, why should I have to take an injection of some concoction?”
The enthusiasm with which vaccine and mask opponents have embraced the expression has led many reproductive rights advocates to distance themselves from it. In the wake of the June 24 Supreme Court decision that reversed the federal right to abortion, advocates for reproductive rights have retooled their language, opting for terms like “Bans off our bodies” and “Say abortion,” said Jodi Hicks, president of Planned Parenthood Affiliates of California.
“In this moment,” Hicks said, “to co-opt that messaging and distract from the work that we’re doing and using it to spread misinformation is frustrating, and it’s disappointing.”
Rachel Bluth of Kaiser Health News has more on the story here.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.





