Should you wait for the Omicron booster? Why experts say you should ‘get it now!’
If you’re like most Americans, you’ve gotten your primary doses of a COVID-19 vaccine, but you haven’t gotten the recommended booster shots. So if it’s been several months since your last primary dose, you’re probably due for a booster.
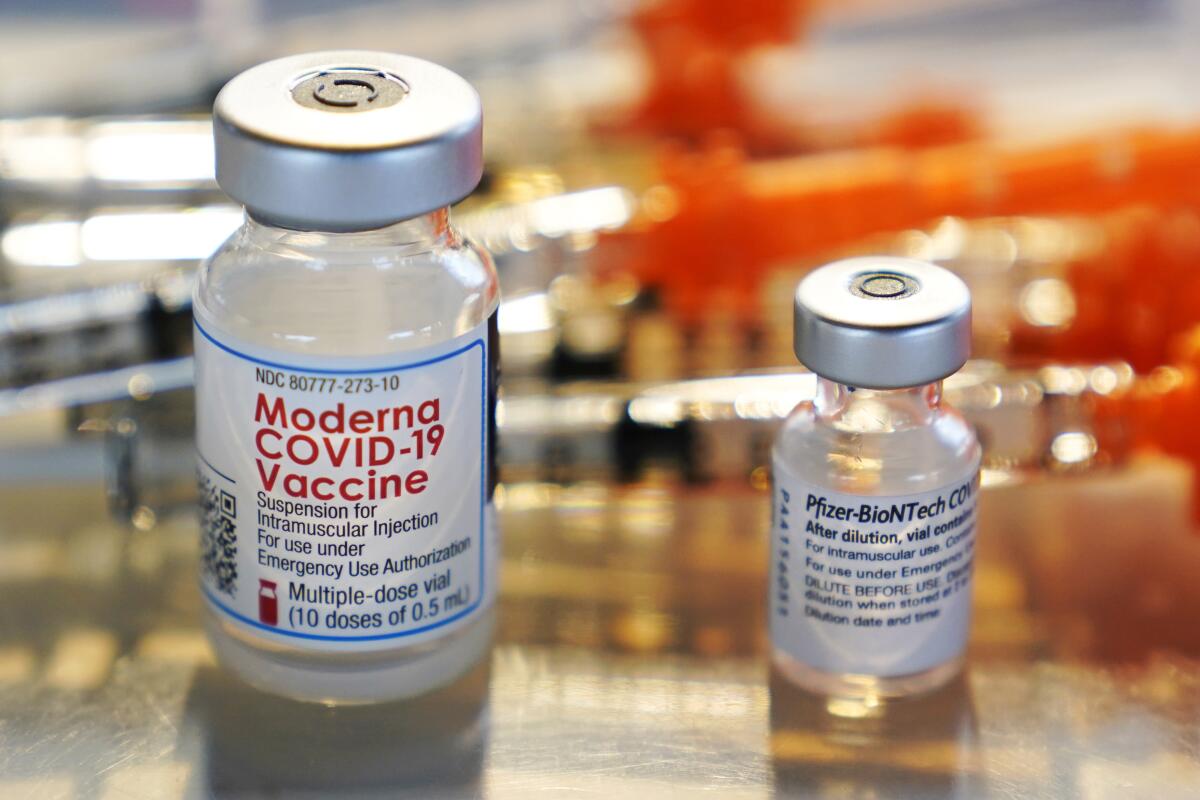
But the companies behind two of the more popular COVID-19 shots, Moderna and the team of Pfizer and BioNTech, have thrown a new variable into the mix. Last month, they said they had new versions of their booster shots that are designed to target the highly infectious Omicron family of COVID variants.
So you may be asking yourself, “Should I get a booster shot now, while cases are surging, or should I wait until the new boosters are ready, probably this fall?”
The answer, multiple vaccine experts said emphatically and without hesitation, is that there’s no time like the present.
“Definitely get it now!” Paula Cannon, a professor of molecular microbiology and immunology at USC’s Keck School of Medicine, said in an email.
“Trying to predict the future with this virus, even as close as the fall, is not a good idea,” she said. “And even with the more Omicron-specific vaccines, it’s still highly unlikely that they will provide absolute protection against infection.”
That hardly makes them useless, Cannon noted: “They will keep doing the much more important job that all the vaccines do, of protecting against severe illness and death.”
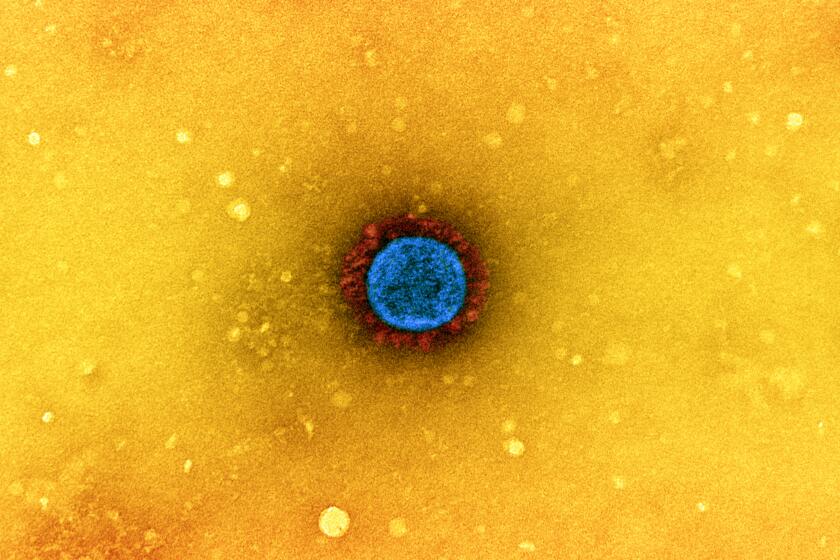
Determining which version of the coronavirus should be used to make COVID-19 vaccines and boosters is an exercise in educated guesswork.
The Centers for Disease Control and Prevention urges everyone who’s at least 5 years old to get one to two booster shots, depending on their age and the health of their immune system. That’s because the protection offered by the vaccine fades over time.
But Dr. Thomas Campbell, an infectious disease specialist at the University of Colorado School of Medicine, said CDC data show that while two-thirds of the U.S. population has received the full course of primary doses (two shots in the case of Moderna and Pfizer’s vaccines, or one of the Johnson & Johnson vaccine), just under half of that group has gotten one booster shot. And less than 30% of the adults over 50 who’ve gotten one booster have gone on to receive the second recommended follow-up, Campbell said.
As a result, “only a small percentage of the people across the population” have received all the vaccine doses the CDC recommends, he said. Rather than waiting for the next generation of shots, Campbell said, “people should get the boosters that they’re eligible for now.”
He also noted that the forthcoming Moderna and Pfizer boosters, like the current ones, are available only to people who have received both of their primary doses. So if you stopped after one shot, you need to get the second one. Those shots provide certain forms of protection that the new boosters will not.
We look at the science behind the need for COVID-19 booster shots.
Dr. Otto Yang, professor of medicine and associate chief of infectious diseases at the David Geffen School of Medicine at UCLA, said the question of whether to wait for the new boosters “has come up quite a lot,” and that “different people have different opinions.” But his advice? “Get it now, and then worry about the variant-specific booster later.”
One major reason to get the shot now, he said, is the summer surge in reported cases. Another is that the current vaccine “remains extremely good at keeping people from getting extremely ill or dying.”
But a third reason, he said, is that the upside appears to be relatively small. Data from Moderna shows that its targeted booster “was only modestly better” than the current one “in terms of antibody activity against Omicron.”
And besides, antibodies are only part of the story when it comes to battling COVID.
When the coronavirus attacks the body, the immune system steps up, trying to respond quickly and powerfully enough to stop the virus from running wild.
Vaccines stimulate two different parts of the body’s immune system: antibodies, which mainly try to stop a virus from infecting a cell, and T cells, which can kill infected cells and stimulate the production of more antibodies. To oversimplify a bit, Yang said, antibodies seek to prevent an infection from spreading throughout your body, and if that fails, T cells try to prevent the infection from doing much damage.
The antibodies initially generated by the vaccine can prevent the coronavirus from latching on to healthy cells and fueling an infection. But SARS-CoV-2 has evolved, and variants like Omicron have changed enough that those antibodies may not recognize them.
“That’s why the vaccines have not been very good at preventing people from getting infected” by Omicron, Yang said. But the variant is about 97% the same as the original, he said, so the T cells stimulated by the vaccines aren’t hindered from doing their job.
“That’s why the vaccines have continued to work very well in preventing us from getting [extremely] sick and dying,” Yang said. And that’s why “the new vaccine is not going to be much better than the original, if at all, in preventing severe illness and death.”
L.A. County coronavirus weekly death rate 70% higher than in Bay Area: Why so much worse?
Research shows that vaccine-induced T cells fade over time, as do the antibodies. That’s why the CDC has recommended booster doses. At this point, the CDC is not recommending a second booster for people under 50 with healthy immune systems, or a third booster for people 50 and older or who are immunocompromised.
Many experts believe that annual or semi-annual COVID-19 boosters may ultimately be needed, but researchers are still studying the longer-term effectiveness of the vaccines.
“The thing people have to realize,” Campbell said, “is that we’re learning how to use these vaccines as we’re using them.”
One other X factor, according to Cannon, is the evolutionary path SARS-CoV-2 follows.
“We don’t even know that the virus variants circulating in the fall will still be Omicron and friends,” she said. “We could be looking at a completely new variant. ... So rather than trying to second-guess anything, we should stick with what we know, which is that boosters work well now, to top up people’s immunity.”
The bottom line, Cannon said: If you’re eligible for another dose, “you should definitely go ahead and get a booster now.”
About The Times Utility Journalism Team
This article is from The Times’ Utility Journalism Team. Our mission is to be essential to the lives of Southern Californians by publishing information that solves problems, answers questions and helps with decision making. We serve audiences in and around Los Angeles — including current Times subscribers and diverse communities that haven’t historically had their needs met by our coverage.
How can we be useful to you and your community? Email utility (at) latimes.com or one of our journalists: Jon Healey, Ada Tseng, Jessica Roy and Karen Garcia.