Coronavirus Today: When zero tolerance backfires
Good evening. I’m Karen Kaplan, and it’s Tuesday, March 22. Here’s the latest on what’s happening with the coronavirus in California and beyond.
On a good day in Hong Kong, a call for an ambulance to transport the body of a newly deceased COVID-19 victim will be answered within an hour.
But it’s been awhile since the city has had a good day. Now, in the midst of the deadliest outbreak in the world, it can take up to 48 hours for an ambulance to arrive.
“It’s a nightmare,” said an exhausted nurse who was caring for 150 COVID-19 patients at a temporary isolation facility with just one other co-worker. “It’s really shocking.”
What a difference a month makes.
On Feb. 18, Hong Kong’s cumulative COVID-19 death toll stood at 259. That’s roughly 10 deaths per month since the pandemic began.
The low figure seemed like a clear sign that the city’s zero-tolerance approach to COVID-19 was working. As my colleagues David Pierson and Stephanie Yang explain, the strategy relies on mass coronavirus testing for residents, isolation for those who test positive, quarantines for those who are exposed, and tight border controls to keep the virus out.
But as in the U.S. and Europe, people in Hong Kong were eager to resume their normal lives. They wanted to go to work, send their kids to school, and travel.
The highly transmissible Omicron variant was ready to take advantage when they let down their guard. Since mid-February, the number of daily cases increased by more than 800%. Experts predict that more than half of the city’s roughly 7.5 million residents will be infected by the time the current surge is over.
As of Tuesday, Hong Kong’s cumulative COVID-19 death toll was 6,364, according to the tracker maintained by Johns Hopkins University.

Many experts now say the city’s zero-tolerance policy deserves a big share of the blame.
For starters, it means the population had virtually no natural immunity to the coronavirus. That wouldn’t have been a problem if the virus could have been contained or eradicated, like the one that causes severe acute respiratory syndrome. (No cases of SARS have been reported anywhere in the world since 2004.)
Unfortunately, it’s way too late to contain this coronavirus. Having caused nearly half a billion confirmed infections and who-knows-how-many-more that were never officially documented, the virus is bound to become endemic. That means it will remain in circulation for the foreseeable future, eventually causing a predictable number of illnesses and deaths each year, like the flu.
Another problem with the apparent success of zero tolerance is that it reduced the urgency to get vaccinated.
That was particularly true among senior citizens, the group most likely to become seriously ill if infected. Experts say seniors were influenced by false claims that COVID-19 vaccines were risky for people who were elderly and frail. That misinformation hit a receptive audience: Hong Kong’s recent political unrest has made residents skeptical of health advice from government officials.
Considering there were so few COVID-19 cases, many people reasoned that the potential benefits of the vaccines weren’t big enough to warrant the possible risks.
As a result, when Omicron got to Hong Kong, fewer than 45% of those 70 and older were vaccinated. And among those who lived in assisted-living homes, fewer than 20% were vaccinated.
That helps explain why about 9 out of 10 recent deaths have occurred in patients 60 and older.
“This tragedy was entirely predictable, and it was entirely preventable,” Dr. Gabriel Leung, dean of medicine at the University of Hong Kong, told my colleagues. “We’ve had early, sustained, uninterrupted, privileged access to vaccines. And yet we are probably the only population in the global north that has such poor coverage of our most vulnerable.”
Some say it’s time for Hong Kong to revisit its zero-tolerance strategy.
“In the earlier phases of the pandemic, the goal of keeping cases as close to zero as possible was reasonable,” said Dr. Keiji Fukuda, who retired last year as director of the University of Hong Kong’s public health school. But now, “since the most likely scenario is that the world will be living with COVID-19 indefinitely, the value of a zero-case policy diminishes.”
By the numbers
California cases and deaths as of 5:40 p.m. on Tuesday:
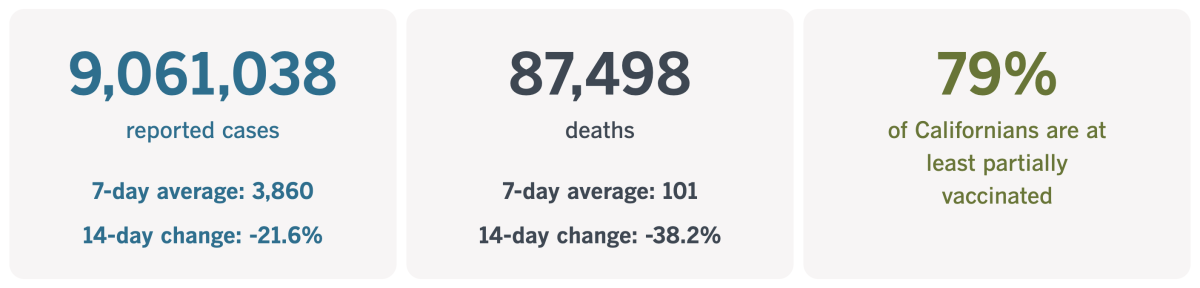
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Sometimes medicine really is the best medicine
It’s hard to imagine a company that channels the organic/wellness/GMO-free ethos better than Dr. Bronner’s, the Southern California soap maker whose product labels remind us to “be generous, fair & loving to Spaceship Earth and all its inhabitants.” It sells its products in bottles made of 100% recycled plastic, seeks out Fair Trade suppliers to source its raw materials, and backed the hemp industry in its fight against the U.S. Drug Enforcement Agency.
Last summer, when the Delta variant was pushing COVID-19 cases up for the first time since the devastating winter surge, Chief Executive David Bronner was looking for ways to boost his workers’ vaccination rate without instituting a mandate. His solution: Offer a $1,000 bonus to employees who opted to get the shots.
It seemed like a move befitting a good corporate citizen. And although many commended it, the company also weathered a wave of criticism and a slew of pledges to stop buying its products.
“I’ve had DrBronner soap in my bathroom consistently since at least 2012. Never again. Not a cent,” one longtime customer wrote on Twitter.
“Nooooooo !!!!! Say this isn’t true,” another critic tweeted. “Health can’t be found in a vial.”
Perhaps none of the messages captures the extent to which the company’s detractors are living in a parallel universe better than this one:
“Lost a customer. Cannot believe you are bribing your employees to get a vaccine that doesn’t even work! Those that are vaccinated are the ones spreading covid…you are the ones to blame for killing people now. The vaccine doesn’t stop you from getting it or spreading it!”
(It should go without saying that all of those claims are wrong.)
Ironically, some of the most off-base advice about COVID-19 vaccines is coming from social media influencers who claim to be all about health and nutrition. To hear them tell it, there’d be no need for COVID-19 vaccines or antiviral treatments (let alone ventilators or ECMO machines) if people would just eat right, exercise and take their vitamins.
And to make matters worse, the pandemic has actually increased the visibility of influencers who are spreading dangerous misinformation and conspiracy theories, my colleague Laura Nelson reports.

Renée DiResta, the technical research manager at the Stanford Internet Observatory, said it’s easy to understand why people are drawn to supporters of dietary supplements and mega-doses of vitamins: It’s the kind of actionable advice that makes a person feel like he or she in control of an uncertain — even scary — situation.
“These are natural human impulses, and it’s very, very hard to counter,” said DiResta, who helps track online misinformation about COVID-19 vaccines.
Nelson spoke to a high school science teacher who explained the situation more bluntly.
“People who are conspiracy theorists can’t deal with the unknown,” said the teacher, who counts her husband among them. “But if you show that you’re scared of something, that’s a sign of weakness. So instead, they’re telling themselves that they know more about the virus than other people. It gives them a feeling of power.”
The Center for Countering Digital Hate, a research group based in London, issued a report that traced two-thirds of the online misinformation about COVID-19 vaccines to a dozen influencers. Eight of the 12 are connected to health, wellness and nutrition. They include Dr. Joseph Mercola, whose advice about using vitamins and supplements to treat COVID-19 prompted a warning from the Food and Drug Administration; his YouTube channel was shut down for violating the service’s ban on vaccine misinformation.
No one denies that a healthy diet and exercise are good for you, said Dr. Danielle Belardo, a cardiologist and vegan in Newport Beach. Where people go wrong is in thinking that those things are a substitute for medicines and vaccines, she said, and “that anything that isn’t natural is harmful.”
Belardo said many of her vegan patients initially questioned the need for the COVID-19 vaccine. In her view, those patients had simply fallen under the sway of people who promoted — and in some cases, profited by selling — products like juice cleanses and dietary supplements.
Her patients weren’t lost causes. They’d simply “found the wrong echo chamber,” Belardo said. All of them are now vaccinated, she added.
California’s vaccination progress
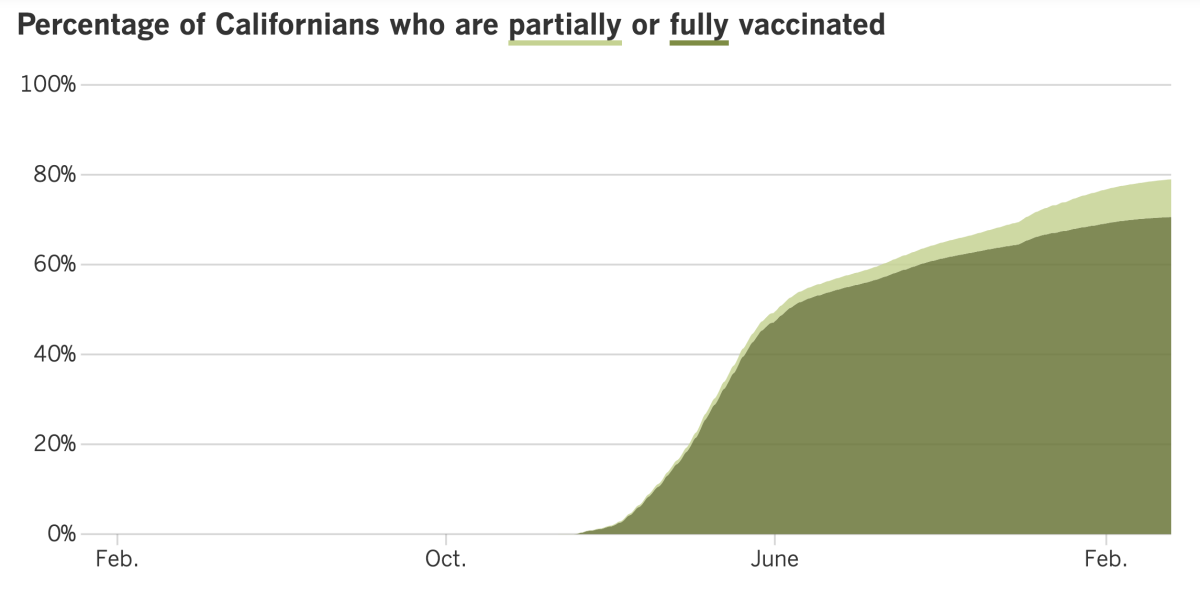
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
Coronavirus cases are either flat or still declining across California. But that’s not the case in Asia, Europe or parts of Africa, and that has some officials concerned that an upswing may be inevitable here as well.
The most recent update from the World Health Organization reported an 8% increase in weekly global coronavirus cases, the first week-to-week jump since late January. It happened to coincide with a relaxation of mask rules and vaccine requirements in Los Angeles County and elsewhere.
But what has really caught experts’ attention is the Omicron subvariant known as BA.2, or “stealth Omicron.” It’s 30% to 60% more contagious than the original Omicron, and it’s making up a growing share of new cases in the U.S.
As of Saturday, BA.2 accounted for 35% of the coronavirus specimens nationwide, according to estimates from the Centers for Disease Control and Prevention. Just five days earlier, it made up 22% of specimens; a week before that, the figure was less than 13%.
In L.A. County, BA.2 accounted for 6.4% of coronavirus specimens analyzed between Feb. 20 and 26, the most recent data available, according to Public Health Director Barbara Ferrer. But BA.2 is already dominant in some parts of the state, such as Palo Alto. And it will probably account for the majority of cases in San Diego County in the near future, according to Kristian Andersen, a microbiologist at the Scripps Research Translational Institute.
In a new study, scientists surmised that BA.2’s superpower is its enhanced transmissibility, not its ability to evade an immune system fortified by vaccination or past infection.
The scientists came to this conclusion after subjecting blood plasma from 24 healthy volunteers to BA.2 and its cousin BA.1, as well as the original coronavirus strain from Wuhan. BA.2 was a little bit better than BA.1 at getting past the immune defenses of people after two and three doses of vaccine. And once people were boosted, exposure to BA.1 elicited a slightly higher level of antibodies compared to exposure to BA.2 — a measurable difference but too small to have a big real-world effect, the study authors said.
The significance of BA.2’s rise is unclear. An estimated 95.3% of Southern Californians and 95.6% of people in the San Francisco Bay Area have some coronavirus immunity either through vaccination or a past infection (or both), so another surge that strains hospitals isn’t necessarily in the cards. And even as BA.2 grows, the coronavirus as a whole isn’t (for now at least).
“Interestingly — and this gives me hope — it is not driving up the levels overall,” said Dr. Sara Cody, the Santa Clara County public health director. “I don’t know why, but it isn’t.”
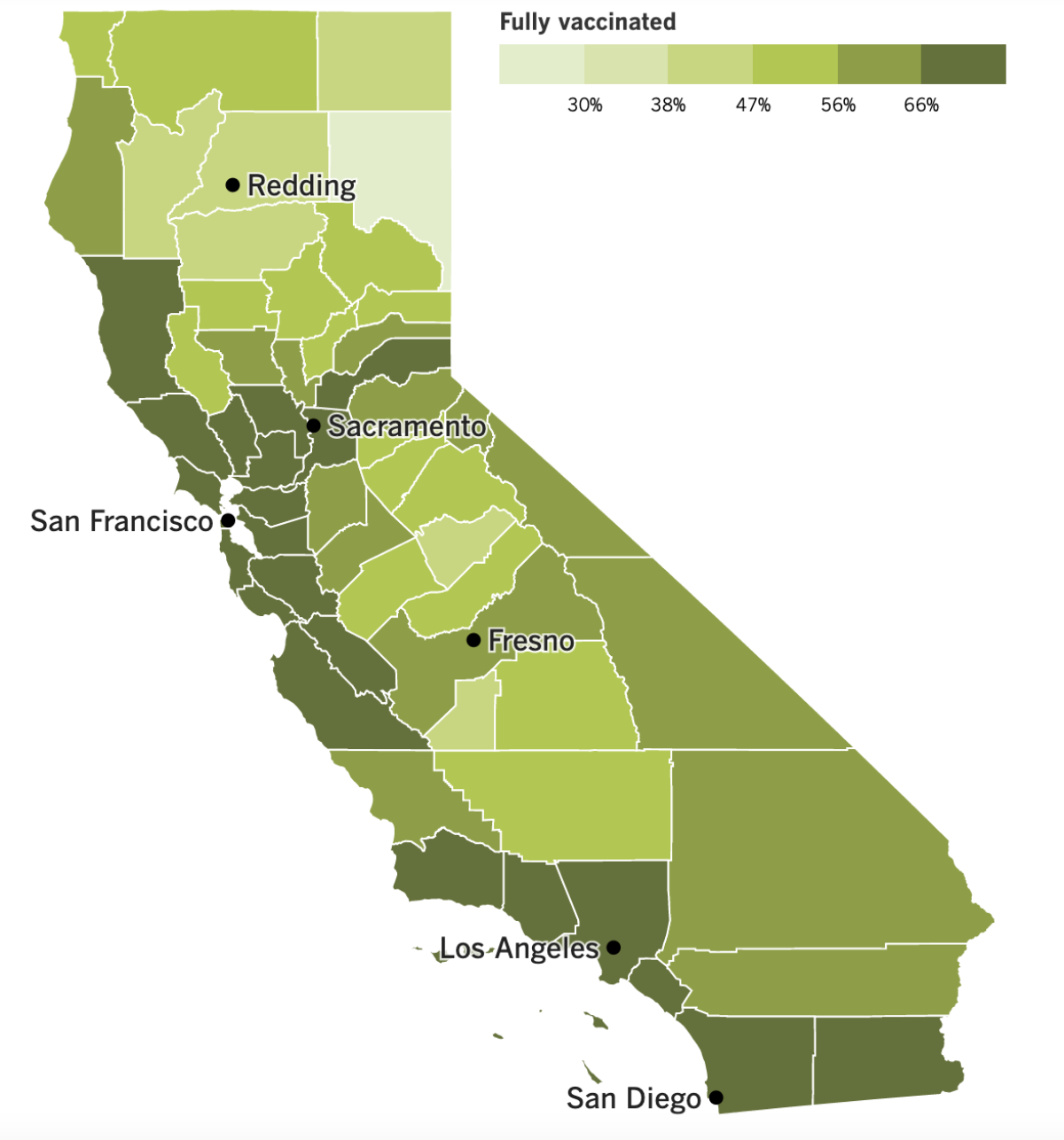
If Californians want some insurance against BA.2, they should be sure to get themselves vaccinated and boosted (if they haven’t already). A data analysis by my colleagues Luke Money and Sean Greene demonstrates the protective value of vaccines during the state’s recent Omicron surge.
The Bay Area had the second-highest case rates during the surge, but it had the lowest hospitalization and death rates. It’s probably not a coincidence that 80% of residents are fully vaccinated and 50% are boosted.
Rural Northern California had nearly 5,000 coronavirus cases per 100,000 people since Dec. 1, and the San Joaquin Valley approached 7,400, whereas Southern California had more than 10,000. Yet the death rates in all three regions were comparable — 32.2 per 100,000 people in the Southland and the San Joaquin Valley, and 31.7 per 100,000 people in Northern California.
Why wasn’t Southern California’s death rate higher considering it had so many more infections? It could be that 69% of SoCal residents were fully vaccinated, compared with 53% of people in NorCal and 55% of those living in the San Joaquin Valley. (Booster rates were similarly skewed.)
Here’s another practical reason to get vaccinated and boosted now if you haven’t already: The U.S. government may have to stop footing the bill for the shots in the near future.
Congress and the White House are stuck in a stalemate over the Biden administration’s request for $22.5 billion in COVID-19 funding. Republicans say the trillions of dollars they’ve already allocated should cover the administration’s expenses, but when House Speaker Nancy Pelosi tried to negotiate cuts with GOP leaders, she ran into problems with fellow Democrats.
The upshot is that the Health Resources and Services Administration said it would stop paying for coronavirus tests and COVID-19 treatments for the nation’s 28 million people without health insurance. Claims will no longer be accepted after midnight tonight. If the money situation isn’t resolved, the agency will stop buying COVID-19 vaccines for uninsured people after April 5.
“The lack of funding for COVID-19 needs is having real consequences,” said a spokesman for the Health Resources and Services Administration. “We have begun an orderly shutdown of the program.”
In other news from Washington, D.C., White House Press Secretary Jen Psaki tested positive for a coronavirus infection on Tuesday, less than five months after a previous infection. As before, she is experiencing mild COVID-19 symptoms, she said. Psaki had two “socially distanced meetings” with Biden on Monday, but he doesn’t qualify as a “close contact” under CDC guidelines, and he tested negative on Tuesday.
The coronavirus has caught up to a slew of dignitaries in the past week. Irish Prime Minister Micheal Martin tested positive on Wednesday night while in Washington to celebrate St. Patrick’s Day (and was informed of his test result during an event with Biden and Pelosi). Both German President Frank-Walter Steinmeier and King Harald V of Norway tested positive on Tuesday.
China reported some significant cases of its own over the weekend. Two elderly COVID-19 patients in the country’s northeastern province of Jilin died of COVID-19, becoming the country’s first pandemic fatalities since January 2021.
Meanwhile, Samoa went into lockdown on Saturday as the country grappled with its first unexplained coronavirus infection of the pandemic. A woman who was about to leave the island nation tested positive, suggesting that a previously undetected outbreak had been going on for days or weeks. The woman had gone to church, a hospital, stores, a library and a travel agency after she felt ill.
And finally, let’s wrap up with some good news: The pandemic may have driven Americans to heavy drinking and drug use, but cigarette smoking hit an all-time low in 2020.
So says a report released Thursday by the CDC. Just 12.5% of adults were using traditional cigarettes that year, and only 3.7% used electronic cigarettes. Health experts outside the CDC said higher prices for tobacco products and new pandemic routines deserved some of the credit.
“People who were mainly social smokers just didn’t have that going on anymore,” said Megan Roberts, an Ohio State University researcher. Parents who suddenly found themselves spending a lot of time at home with their kids may have been motivated to cut back for that reason as well, she said, or they could have been scared to learn that smokers face a greater risk of becoming severely ill with COVID-19.
Your questions answered
Today’s question comes from readers who want to know: When can I get another COVID-19 booster shot?
Variations of this question have been showing up in our inbox for weeks, most recently from a 65-year-old with several preexisting conditions who said he had his first booster shot back in October.
The short answer is that there are no immediate plans to make a second booster shot widely available in the U.S., but the prospect is definitely on the Food and Drug Administration’s radar.
In fact, the FDA’s vaccine advisory committee has a meeting scheduled for April 6 to discuss further boosters, including the possibility that some shots might be tailored to neutralize specific coronavirus variants. Committee members will meet with experts from the CDC and the National Institutes of Health to discuss a a framework for deciding when additional booster shots would be needed, and for whom.
No votes are on the agenda, which means the FDA committee would have to meet at least one more time before the FDA could authorize a second booster shot. After that, the CDC would hold meetings of its own to decide whether to recommend a second COVID-19 booster and, if so, who should get it.
Vaccine makers would like to see additional doses made available in the U.S. Last week, Pfizer and BioNTech submitted an application to the FDA seeking emergency use authorization for a second booster aimed at people ages 65 and up. Two days later, Moderna asked the agency to authorize a second booster dose of its vaccine for all adults. Making it available to everyone ages 18 and up would give doctors and patients more flexibility to protect people with chronic health problems that put them at higher risk of severe COVID-19, regardless of their age, the company said.
If the prospect of having to wait many weeks or even months to get another shot makes you nervous, here’s some reassuring news from researchers in Israel:
In a study of 821 healthcare workers who were fully vaccinated and boosted with Comirnaty (the Pfizer-BioNTech vaccine), those who received a second Comirnaty booster were only 30% less likely to experience a new coronavirus infection and 43% less likely to develop COVID-19 symptoms. In addition, people who got a booster dose of Spikevax, the Moderna vaccine, were just 11% less likely to become infected and 31% less likely to become ill.
The researchers said the issue wasn’t that a second booster had low effectiveness. It was that the first booster was still doing its job, leaving less room for improvement.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The man in the photo above is Chen Weiming. He created the piece behind him, a sculpture that depicts Chinese President Xi Jinping’s head as a giant coronavirus.
The picture was taken last June. Not long after, the sculpture burned to the ground. All that remained were the large red letters that spelled out “CCP Virus.” It was Chen’s way of blaming the COVID-19 pandemic on the Chinese Communist Party.
Chen accused the Chinese government of destroying his work and “wanting to shut down our free speech.” This month, federal prosecutors agreed and filed charges against five people accused of stalking and harassing Chen and others at the behest of the Chinese government.
Zhao Lijian, a spokesman for the Chinese Foreign Ministry, called the charges an “unwarranted denigration and and smearing against China.”
But no one can deny that the tale laid out by the prosecutors is worthy of a movie or a bestselling book. In addition to Chen, the story involves an Olympic figure skater and a scholar. You can read all about it here.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




