Study reveals likely reason for ‘stealth’ Omicron’s recent success
The ability to spread more easily from person to person appears to be the superpower that is driving an upstart sibling of the Omicron variant into wide circulation, a group of scientists has surmised.
That conclusion about the virus known as “stealth Omicron” is explained in a brief report published this week by the New England Journal of Medicine. It’s based on the team’s finding that the virus, whose official name is BA.2, is only slightly better than the dominant BA.1 at evading the protective effects of COVID-19 vaccines.
Both of the Omicron “subvariants” have a common core of genetic mutations. But each has a few that the other doesn’t. For instance, BA.2 lacks a mutation belonging to other versions of Omicron that makes it easy to differentiate them from the Delta variant. (Hence the “stealth” moniker.)
Epidemiologists can watch BA.1 and BA.2 compete against one another in a race to infect people and tell you which is winning. But scientists who study the evolution of viruses would like to understand not just which is winning, but why. As they gain more insight into how individual mutations change a virus’ behavior, they can be better prepared for its next genetic shift.
Right now, BA.2 is making a solid run against BA.1 in the United Kingdom, and may be implicated in the resurgence of COVID-19 there and in other European countries.
BA.1 is still the dominant coronavirus in the United States, and has been since early January. But BA.2 now accounts for 23.1% of new coronavirus infections here, according to estimates by the Centers for Disease Control and Prevention. A week earlier, it made up 13.7% of U.S. infections, and just 7.1% the week before that.
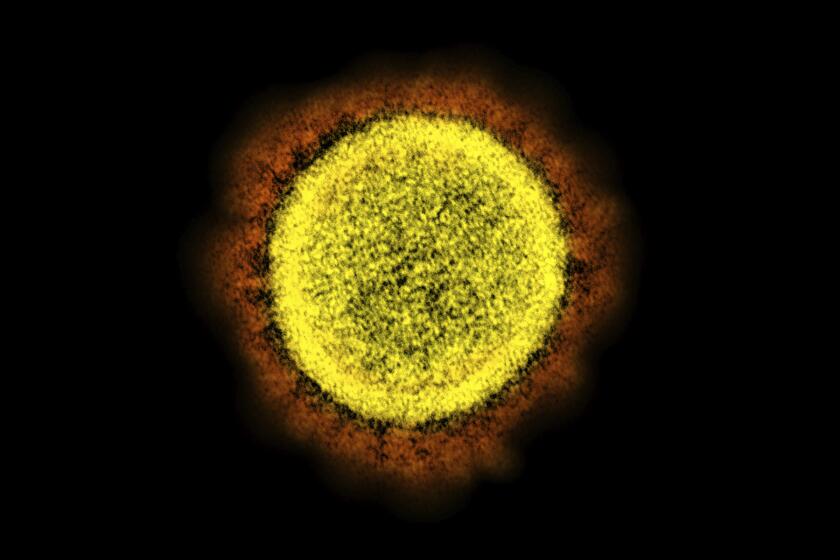
Given scientists’ growing understanding of the SARS-CoV-2 coronavirus’ behavior, as well as the locations of the the subvariants’ mutations, the list of potential attributes that could account for their success has been narrowed down to two prime suspects: immune evasion and transmissibility.
If the virus has gotten better at evading the protection conferred by either natural infection or vaccines, it could be running up its numbers by infecting people who were thought to have immunity. And if that’s the case, broader vaccination, additional booster shots or reformulated vaccines may be needed.
A study of healthcare workers finds that a second booster dose of Pfizer’s COVID-19 vaccine did little to prevent Omicron infections.
But if that’s not it, the best alternative explanation is that the virus has improved its ability to spread, and it might do that by many means. Perhaps it causes more asymptomatic infections, so people who are infected continue to circulate and infect others. Perhaps the virus lingers longer in the air and gets more chances to find new hosts. Perhaps it establishes itself more readily in the nose and mouth, where it’s more likely to be expelled into the path of new victims.
To find out, scientists from the Massachusetts Consortium on Pathogen Readiness set out to explore whether BA.2 was better at infecting people who should have had some immunity, either from a COVID-19 vaccine or a previous coronavirus infection.
Omicron is known to have found ways to elude the immune defenses of vaccinated people more readily than the original coronavirus that emerged from Wuhan, China, and the Alpha and Delta variants that came later. Omicron has also upended the effectiveness of COVID-19 treatments that worked by mimicking the immune system.
The researchers investigated whether the BA.2 subvariant further improved on BA.1’s powers of vaccine evasion. They recruited 24 healthy people and drew samples of their blood three times: after they received two doses of Pfizer-BioNTech vaccine; six months later when immunity was known to have waned and two weeks after they received a booster shot.
In a lab, they put those subjects’ plasma up against the original Wuhan strain of the virus, as well as BA.1 and BA.2. Then they measured the neutralizing antibody response.
The authors found that after two and three doses of vaccine, BA.2 was a little bit better than BA.1 at getting past the immune systems of vaccinated people. In subjects who’d had three doses of vaccine, levels of neutralizing antibodies — the immune proteins that thwart infection — were about 40% higher against BA.1 than they were against BA.2.
That may sound like a big difference, but it’s actually not, said Dr. Dan Barouch of Beth Israel Deaconess Medical Center, one of the authors of the new report.
The coronavirus variant known as BA.2, or the ‘stealth Omicron,’ now causes more than a third of new Omicron infections around the world.
“These are very different from the changes we saw between the Alpha and Delta variant, or when Omicron overtook Delta,” Barouch said. “Those were 20- and 40-fold differences. We were really talking about orders of magnitude differences in neutralizing antibodies.”
In this case, the smaller difference in antibody levels between BA.1 and BA.2 means that if you sent a large group of vaccinated-and-boosted people to a party where both subvariants were circulating, over the next week you’d find that BA.2 infected a couple of more people than BA.1. But if you exposed partygoers to the Wuhan virus and Omicron, the Omicron variant would likely have caused virtually all infections.
The good news, Barouch added, is that BA.2 hasn’t really bolstered Omicron’s ability to infect people who’ve been vaccinated. The bad news is that both BA.1 and BA.2 are already pretty good at that, he said.
There is some other pretty good news, though it’s very preliminary. In a test of eight people who’d recently been infected with Omicron (and given the timing, BA.1 was assumed to be the culprit), most of them had high antibody levels against the BA.2 variant. Only one person — an unvaccinated subject who’d had a very recent infection — lacked the antibodies needed to prevent reinfection.
That finding suggests that for the many vaccinated Americans that were infected during the Omicron surge, this stealth Omicron isn’t likely to cause a new wave of breakthrough cases.
And so, the scientists wrote, BA.2’s evident ability to muscle aside BA.1 “is probably related to increased transmissibility rather than to enhanced immunologic escape.”
That’s the beginning of the inquiry, not the end. From here, scientists want to explore exactly how BA.2 has managed to make itself even more transmissible than the already wildly infectious BA.1.