Coronavirus Today: States’ fates diverge with Delta
Good evening. I’m Karen Kaplan, and it’s Tuesday, Sept. 21. Here’s the latest on what’s happening with the coronavirus in California and beyond.
The longer the Delta surge drags on in the U.S., the more pronounced the differences between states that have embraced COVID-19 vaccines and those that haven’t.
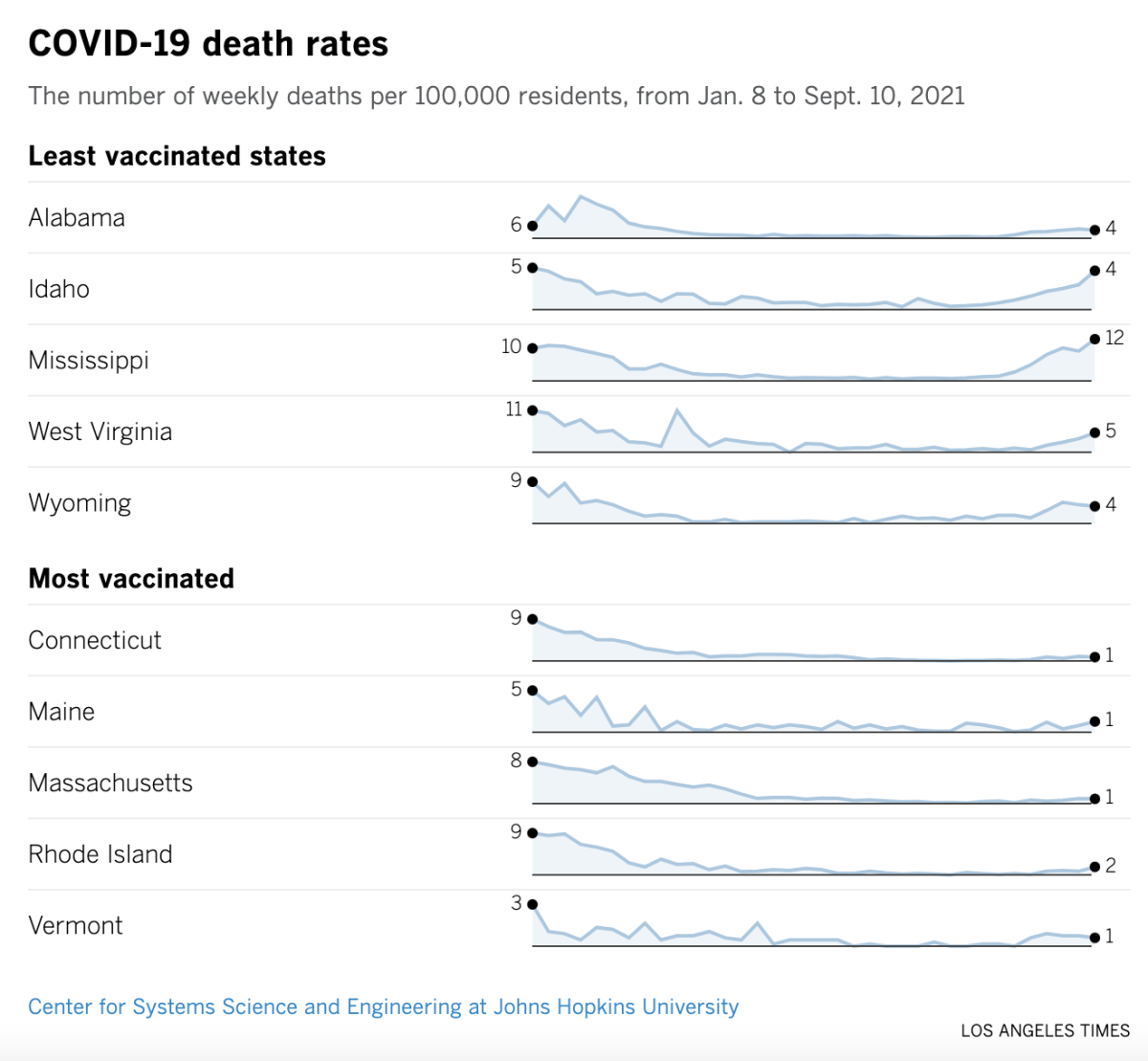
West Virginia, Wyoming, Idaho, Alabama and Mississippi have the lowest full vaccination rates in the country, ranging from 40.2% to 42.1%. At the other end of the spectrum are Rhode Island, Massachusetts, Maine, Connecticut and Vermont, where vaccinations rates range from 67.1% to 69%.
That’s not the only thing that sets them apart. Since the end of April, the COVID-19 death rate in the low-vaccination states has risen to the point where it’s more than three times the rate in the high-vaccination states.
It would be easy to conclude that the states that pooh-poohed the lifesaving vaccines are now paying the price for their hubris. And there would be some truth in that.
But it’s not the whole story, my colleague Emily Baumgaertner reports. She looked closely at the two clusters of states and found there was much that set them apart besides vaccination rates.
The five high-vaccinated states are all in the Northeast, which was an early epicenter of the pandemic. By January 2021, they had endured 152 deaths for every 100,000 residents.
For the record:
9:04 p.m. Sept. 21, 2021An earlier version of this newsletter said the governors of all five of the states with the highest COVID-19 vaccination rates were Democrats. Two of them — Charlie Baker of Massachusetts and Phil Scott of Vermont — are Republicans.
With firsthand knowledge of COVID-19’s potential to cause death and destruction, the governors of these states — three of them Democrats — took an aggressive stance. They declared states of emergency, demanded that people quarantine or produce a negative coronavirus test when they arrived from another state, and imposed mask mandates. In Connecticut, for instance, a restaurant that allowed employees to work without face coverings could be fined up to $10,000 per violation.
In addition, residents of these hard-hit states were inclined to follow public health advice about social distancing.
Meanwhile, the coronavirus seemed to be less of a threat in the five low-vaccinated states. By January, they had absorbed 106 deaths per 100,000 residents — a rate 30% lower than for their counterparts.
In these states, rules about masks were seen as an infringement on personal liberty. Their governors — all Republicans — allowed mandates to expire. They also eased off other restrictions, like capacity limits on businesses. In Wyoming, bars, gyms and theaters resumed operations in early March, with Gov. Mark Gordon asking residents “to take personal responsibility for their actions and stay diligent.”
By late April, the cumulative death toll in the low-vaccinated states was up to 193 per 100,000 residents. That was an 82% increase for the year but still below the 213 COVID-19 deaths per 100,000 residents of the high-vaccinated states.
Recall that, through April, vaccines were still in short supply. The finger-wagging was aimed at people who were cutting the line to get a shot, not people who were passing them up.
But within a few more weeks, there were so many doses available that anyone who wanted a shot could get one (as long as they were at least 16 years old).
People in the Northeastern states jumped at the chance to protect themselves. Their governors helped things along by requiring health workers to get vaccinated; some of them required state employees to get vaccinated, too, or submit to weekly coronavirus testing.
That’s not what happened in the other states. The governors of Idaho, Wyoming and Alabama all issued orders banning vaccine passport systems, which would have required residents to show proof of vaccination to access state services or facilities. All five governors have declined to issue vaccination mandates for healthcare workers.
With such starkly different approaches to vaccination, the low-vaccinated states not only caught up to the death toll of the high-vaccinated states but also overtook them.
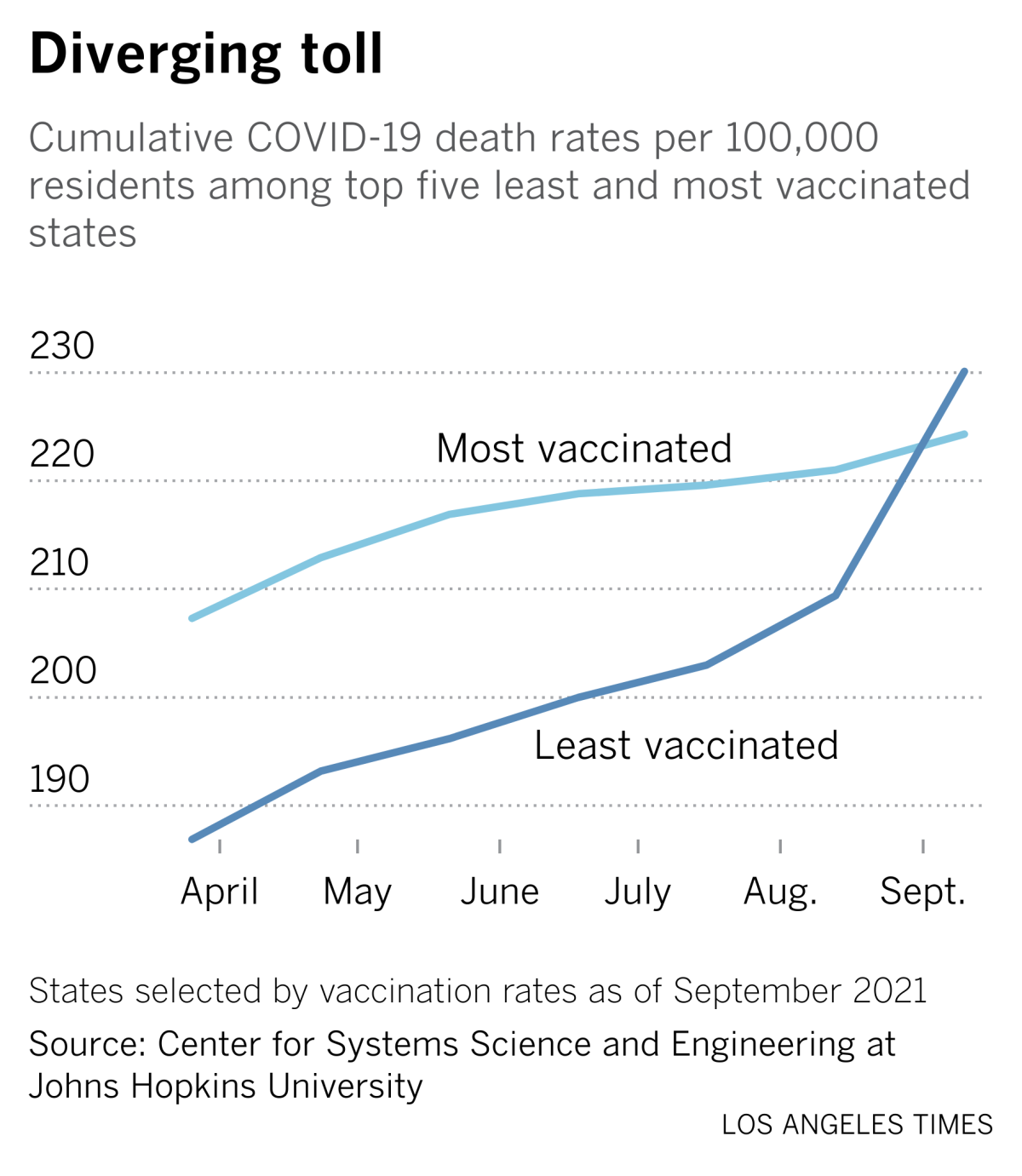
As of Sept. 10, the five states led by Republicans had tallied 230 deaths per 100,000 people, compared with 224 deaths per 100,000 in the states led by Democrats.
If present trends continue, that gap will get wider — and fast.
By the numbers
California cases and deaths as of 4:05 p.m. Tuesday:
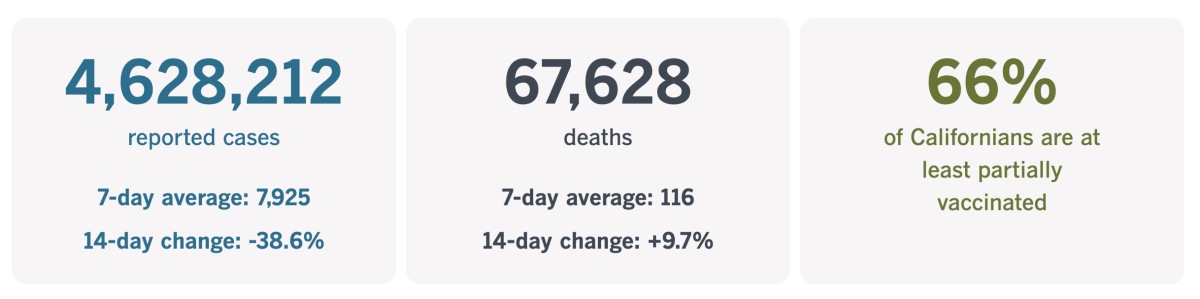
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
What about the next pandemic?
Politics and ideology aren’t just influencing the way states are handling COVID-19 now. In some cases, they’re undermining states’ ability to respond to future public health emergencies, too.
Spurred on by voters who’ve had it with lockdowns and mandates, Republican legislators in all 50 states have pressed for laws that would take power away from the state and local officials responsible for protecting the public from infectious diseases.
Some of those bills were never passed, and others were vetoed by governors. But in at least 26 states, there are now laws in place that permanently weaken the government’s ability to respond to outbreaks, according to a review by our friends at Kaiser Health News. That number could rise further, since a handful of state legislatures are still in session.
And it’s not just lawmakers. Three other states have seen public health powers reduced, via an executive order, a ballot initiative and a ruling by the state Supreme Court.
All this activity makes public health officials feel like they’re the enemy. But that enemy ought to be the coronavirus — or the measles, or Ebola, or the next pandemic flu that could jump from birds to humans at any time.

What exactly do these new measures do? Here are a few examples:
- In Arkansas, a new law makes it impossible to implement a mask mandate in schools or most other places, because they are “a burden on the public peace, health, and safety of the citizens of this state.” The only venues where they may be allowed are state-run healthcare settings and private businesses that choose to adopt them.
- In Idaho, it is now possible for a countywide public health order to be vetoed by county commissioners. Typically, these commissioners have no expertise in public health. But they do have to face the voters periodically, so their incentive to do what’s popular may outweigh their incentive to follow the science.
- In Kansas and Tennessee, the decision to close schools rests with elected school board members, not health officials.
- In Montana, any jurisdiction that tries to bolster state health measures with stronger rules of their own could wind up losing 20% of some funding.
More broadly, nine states have passed laws to ban or limit mask mandates. At least 16 more have put limits on health officials’ authority to implement mask mandates, to require people with known infections to isolate themselves, or to order quarantines for people who’ve been exposed.
At least 17 states now have laws that ban vaccination mandates or the use of vaccine passports, or they have made it easier for residents to sidestep vaccination requirements.
“It’s kind of like having your hands tied in the middle of a boxing match,” said Kelley Vollmar, executive director of the Jefferson County Health Department in Missouri.
Arkansas Gov. Asa Hutchinson has had second thoughts about signing the statewide ban on mask mandates. Last month, he called the Legislature into a special session and tried to get lawmakers to make an exception for schools. They wouldn’t.
Laws like these might make people feel as though they’re punching back against COVID-19, or sticking it to the health experts who keep asking them to do things they don’t want to do. The sense of exhilaration will be temporary, but the consequences of these new laws could be permanent.
“We really could see more people sick, hurt, hospitalized or even die, depending on the extremity of the legislation and curtailing of the authority,” said Lori Tremmel Freeman, head of the National Assn. of County and City Health Officials.
California’s vaccination progress
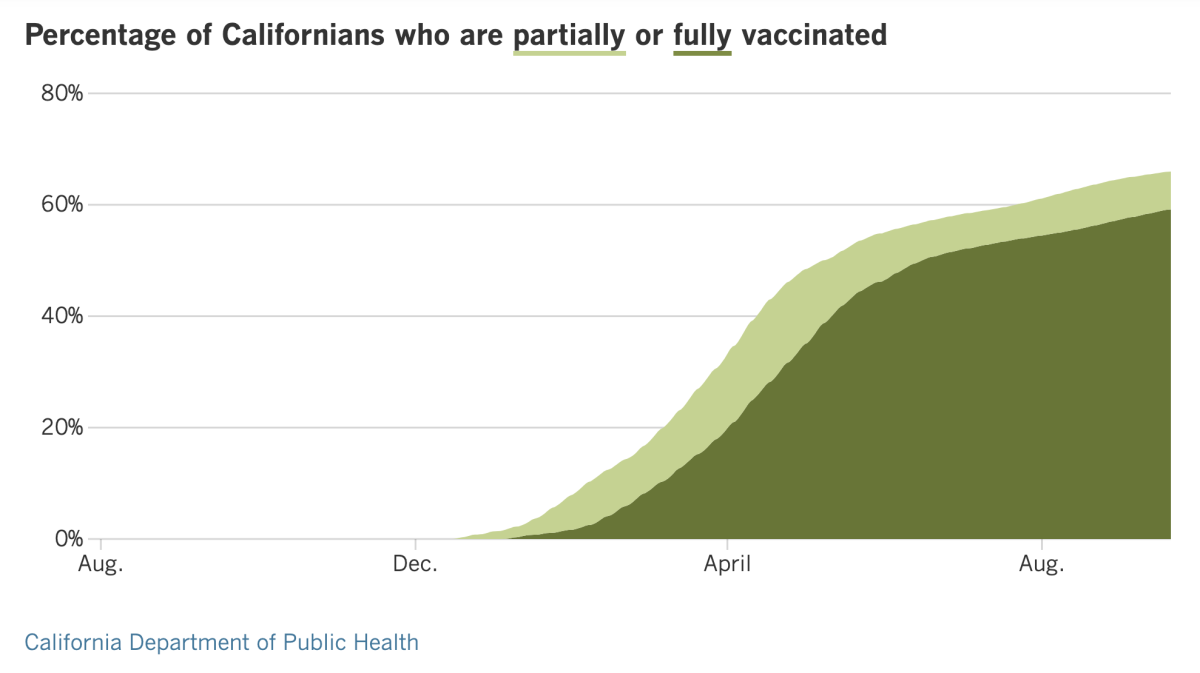
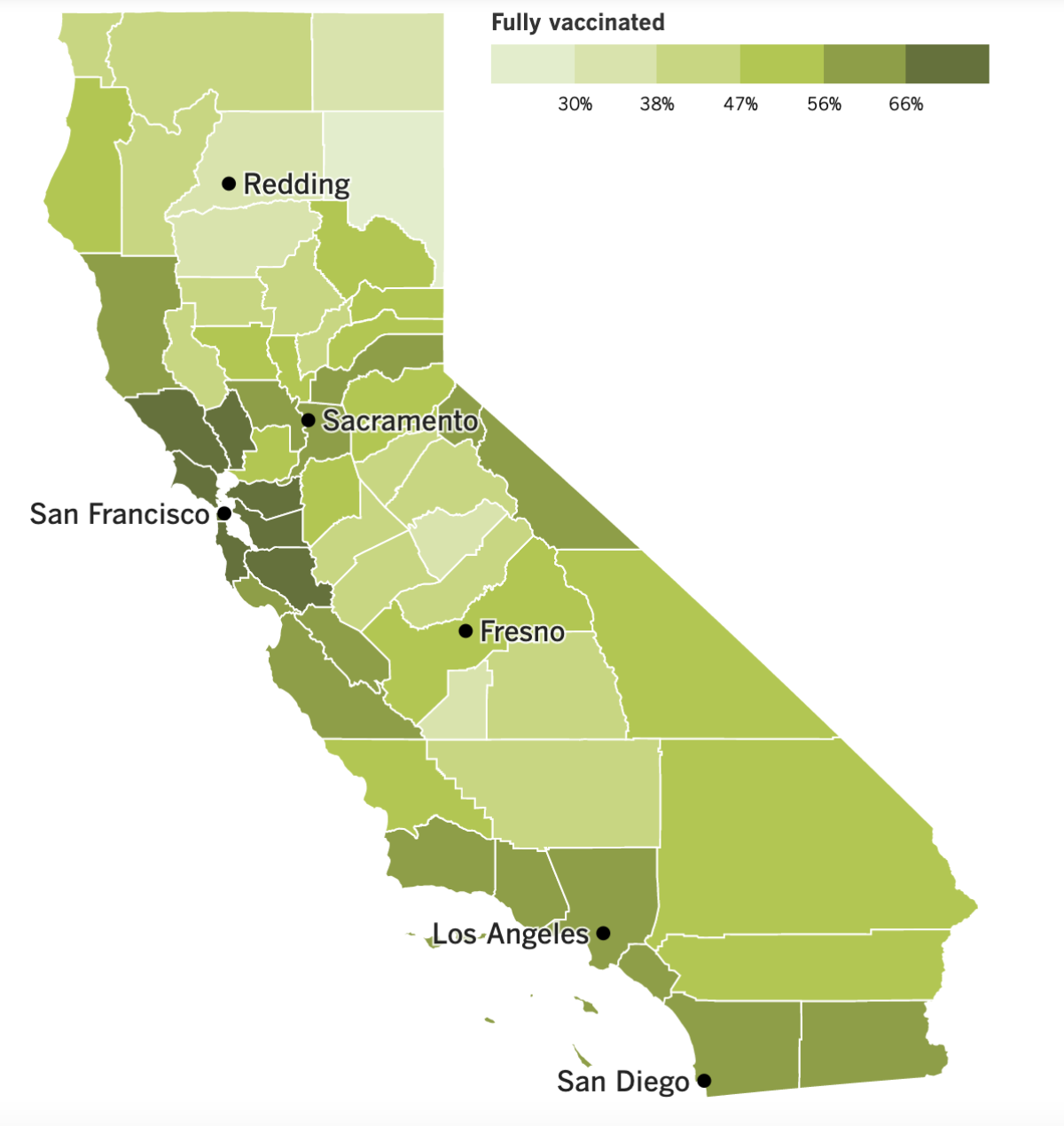
See the latest on California’s vaccination progress with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
In other news ....
Congratulations, California! Our coronavirus case rate is now lower than any other state in the nation, according to the Centers for Disease Control and Prevention.
As of Tuesday afternoon, the CDC says we’ve recorded 95.3 new coronavirus cases per 100,000 residents over the last seven days. The corresponding number for the country as a whole is 250.7 new cases per 100,000 people.
Experts attribute California’s success to its early efforts to counter the threat posed by the Delta variant, which spreads more readily than its predecessors. Some of those were statewide, such as rules requiring unvaccinated people to wear masks in indoor public settings.
Other efforts were more localized, including Los Angeles County’s decision to require everyone to wear masks indoors regardless of their vaccination status. Other counties followed suit.
With 59.2% of all state residents fully vaccinated, California is comfortably above the national average of 54.7% but not at the top of the list. Still, the state has boosted immunizations by requiring all healthcare workers to get vaccinated and by ordering school employees to get the shots or else submit to coronavirus testing at least once a week.
Multiple cities and counties have instituted vaccine-or-testing rules for their employees. And in L.A., the nation’s second-largest school system says students 12 and older will need to be vaccinated by January if they want to keep coming to campus.
On Tuesday, San Francisco International Airport became the first U.S. airport to require all workers to be vaccinated. That includes airline employees and SFO’s retail tenants and contractors, who will be subject to fines if they don’t comply. People who are exempt for medical or religious reasons will have to be tested weekly instead.
Airport director Ivar C. Satero said the directive would ensure the airport was protected in advance of the upcoming holiday travel season, which is likely to be busier than last year’s. “We have an obligation to provide a safe airport facility for the traveling public and our onsite employees,” he said.
Some parts of the state are still struggling, particularly the San Joaquin Valley. In some hospitals, critically ill COVID-19 patients must wait days to be transferred from the emergency department to a bed in the intensive care unit.
Most hospitals in Fresno County are running at 108% to 110% of standard capacity, according to Dan Lynch, director of the Central California Emergency Medical Services Agency. Clovis Community Medical Center is up to 130% of capacity.
With such high patient loads, nurses face challenges in administering monoclonal antibody treatments to newly diagnosed patients. The antibodies are designed to help counteract the coronavirus before it gets a chance to establish itself and attack the body’s organs — ultimately keeping patients out of the hospital.
“A lot of our clinics and hospitals are just saying that they don’t have the resources to commit that amount of time,” said Dr. Rais Vohra, the interim Fresno County health officer.
With COVID-19 cases surging nationwide, demand for monoclonal antibodies has increased by a factor of 20. The U.S. Department of Health and Human Services has responded by reserving the treatment for the hardest-hit areas, which means patients in many parts of California will find them harder to get, said Dr. Regina Chinsio-Kwong, a deputy health officer for Orange County.
On the vaccine front, officials at Pfizer said Monday that the COVID-19 vaccine it developed with BioNTech works well for children ages 5 to 11, and that it won’t be long until the company asks the Food and Drug Administration to authorize it for emergency use for kids in that age group.
The reformulated vaccine contains a dose that’s only a third as high as the one given to adolescents and adults. Even so, after two shots, the antibody levels in children are as strong as in teens and young adults, the company said.
Dr. Peter Marks, who heads the FDA center that evaluates vaccines, said he hoped the agency would be able to evaluate the data within “a matter of weeks” once it’s submitted.
Meanwhile, Johnson & Johnson said Tuesday that a second dose of its vaccine strengthened recipients’ immune response. When study subjects received a second dose two months after the first, the regimen was 75% effective at preventing moderate to severe cases of COVID-19, the company said.
In another analysis, J&J said a booster given after two months increased antibody levels by a factor of four to six. When a booster dose was given after six months, antibodies rose by a factor of 12.
Neither J&J’s nor Pfizer’s results have been published or vetted by other scientists.
The Biden administration is leaning on vaccines to simplify its pandemic travel restrictions. Starting in November, all foreigners will be allowed to fly into the U.S. if they have proof of vaccination and a negative coronavirus test.
The new policy will allow noncitizens with work permits to return to their jobs in the U.S. and enable holiday reunions. It replaces a hodgepodge of rules that have kept many people out of the country for 18 months, irritating allies in Europe and other places where coronavirus case rates are lower than they are here.
Under the new policy, unvaccinated American citizens who have been abroad will need to be tested a day before they come home, and again after they return.
And finally, the U.S. has reached another grim milestone: The number of Americans who have died of COVID-19 has matched the number that died during the flu pandemic a century ago.
That number is about 675,000. Those deaths represented a larger share of the U.S. population back then, since the number of Americans has tripled over the last 100 years. Still, the death toll for the current outbreak is still rising — forecasters at the University of Washington predict it will reach 776,000 by Jan. 1.
Some experts say the COVID-19 pandemic has an extra layer of tragedy because the country has failed to take full advantage of the vaccines that were made possible by scientific advances since 1918.
“Big pockets of American society — and, worse, their leaders — have thrown this away,” said Dr. Howard Markel, a medical historian at the University of Michigan.
Your questions answered
Today’s question comes from readers who want to know: Is it unhealthy for kids to wear masks all day?
Absolutely not. And don’t be fooled by rumors circulating on social media that claim otherwise.
There’s no need to worry about masks becoming germy or trapping unhealthy levels of carbon dioxide. If the mask is reusable, all you have to do is wash it at the end of the day. Throw it in the laundry just like your underwear, and make sure it’s completely dry before you wear it again. (The CDC has tips for cleaning your mask here.)
If the mask is disposable, be sure to discard it after one wearing and replace it with a fresh one.
Choosing a mask that fits well will help kids avoid skin irritation. (It should go without saying that all this advice applies to adults too.)
Some people have raised concerns that kids won’t learn to pick up on important visual and social cues if the faces they see are covered by masks. Experts counter that if children with vision and hearing impairments can adapt, so can other kids.
Besides, the evidence about masks hindering learning is weak — but the evidence that masks help protect children from the coronavirus is strong.
Arizona’s Maricopa County is home to 166 schools in Phoenix and the surrounding area. Coronavirus outbreaks there were more than twice as likely to crop up in schools without mask mandates than in schools with them, according to the county’s public health department.
Patterns like that have been observed around the country. Plus, wearing masks is particularly effective when it’s combined with other preventive measures, like social distancing.
“There isn’t a single intervention that will win the day,” said Dr. Joshua Schaffzin, director of infection prevention and control at Cincinnati Children’s Hospital.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
Resources
Need a vaccine? Keep in mind that supplies are limited, and getting one can be a challenge. Sign up for email updates, check your eligibility and, if you’re eligible, make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




