Coronavirus Today: A family shattered by COVID-19
Good evening. I’m Amina Khan, and it’s Thursday, Dec. 17. Here’s what’s happening with the coronavirus in California and beyond.
Yesterday, we took you inside California’s strained hospitals, where the flood of COVID-19 patients who are filling beds in intensive care units and spilling over into hallways is pushing doctors and nurses to the breaking point. Today, my colleague Maria L. La Ganga introduces us to a Cathedral City family devastated by COVID-19 — a family that saw seven members fall prey to the coronavirus. Two of them died.
Gabriella Alvarado, age 13, was the first member of the close-knit family to show symptoms. Her mother, 41-year-old Alexandria Cantu Macias, spent a week in the hospital because COVID-19 stole her ability to breathe. Macias’ mother, stepfather and mother-in-law all tested positive for the virus as well.
Alexandria’s husband, Luis Enrique Macias Sr., was sick for only a few days. He took a walk and told his pastor he was feeling better. But he was the first to die. He was 45.
Macias had wanted to start a Christian breakdance group and call it BDC, his son recalled at the outdoor funeral.
“I’m like, ‘BDC? What does that mean, Pops?’ He’d say, ‘It stands for Boogie Down Christ,’” said Luis Enrique Macias Jr. “That’s the kind of dad, son, uncle, brother he is — just a goofball.”
Alexandria’s sister, Tatyana Cantu Broughton, tended to elderly patients at Loving Care Living in Palm Springs. She adored the color purple and Dia de Los Muertos. She died of COVID-19 less than 48 hours after her brother-in-law. She was 37.
The virus is “like a thief in the night,” Alexandria said. “It comes in to steal and destroy, and you just don’t know when it’s coming in, when it’s going to affect you. ... It affects everybody.”
Some suffer more than others. Latino and Black people have experienced higher rates of hospitalization and death than their white peers. So have essential workers.
Those trends certainly apply to Macias’ family: Alexandria is a stock clerk at the Burlington store in Palm Springs. Her stepfather, Federico Cantu Hernandez, did prep work and washed dishes at an Applebee’s before the stay-at-home order led to staff cuts, and he works in construction now. Her husband Luis cleaned parking lots and emptied trash cans, handling maintenance duties for Black & White Sweeping in Indio. And Tatyana, of course, cared for seniors, cooking and helping them get dressed.
No adult in Alexandria’s immediate circle had the luxury of working from home. None could protect themselves and still earn a paycheck. That’s all the more reason why, as La Ganga writes, “the Macias family has seven reasons to be furious that you will not wear a mask, that you went to Thanksgiving dinner for 20 without a second thought, that you dismiss the coronavirus as not much worse than the flu.”
By the numbers
California cases and deaths as of 5:06 p.m. PST Thursday:

Track the latest numbers and how they break down in California with our graphics.
Across California
Hospitals throughout Southern California now have zero available beds in their intensive care units — the latest marker of how the pandemic is pushing healthcare systems to the brink. ICU bed availability in Los Angeles, Orange, San Diego, Riverside, San Bernardino, Ventura, Santa Barbara, San Luis Obispo, Imperial, Inyo and Mono counties was already just 0.5% on Wednesday before falling further Thursday.
The San Joaquin Valley, whose ICUs have hit 0% availability a few times in recent days, rebounded slightly to a still extremely scarce 0.7%. Read more here about how ICU capacity works.
Statewide, hospitalizations have been breaking records for 18 days straight. On Tuesday, 14,939 people in California were hospitalized with coronavirus infections. That’s more than six times the comparable number on Halloween.
It can take two to three weeks for a surge in infections to lead to a corresponding surge in hospitalizations, but once that happens, “the consequences can be sudden and severe,” my colleagues Luke Money, Rong-Gong Lin II and Soumya Karlamangla write. State officials have previously estimated that 12% of newly diagnosed coronavirus cases are likely to require hospitalization, and 12% of those in the hospital eventually end up in the ICU.
If so, things will get far worse in the weeks to come. Consider this: For the first time, more than 50,000 new cases were reported in California in a single day, an L.A. Times tally finds. Wednesday’s new record of 51,724 far outstrips the single-day record set just two days prior, when 42,088 cases were logged Monday.
In Los Angeles County, officials expect that hospitals will be overwhelmed by a wave of patients even larger than the most dire forecasts had predicted. There were more than 1,000 COVID-19 patients in intensive care units as of Wednesday, and if present trends continue, there could be 1,600 to 3,600 coronavirus patients in need of ICU beds by early January. That’s a frightening prospect for many healthcare workers.
“There are simply not enough trained staff to care for the volume of patients that are projected to come and need care,” said Dr. Christina Ghaly, the county’s director of health services. “Our hospitals are under siege, and our model shows no end in sight.”
In Orange County, authorities have forbidden hospital emergency rooms from redirecting ambulances to other medical facilities, after 20 of the county’s 25 emergency medical centers became so overwhelmed with COVID-19 patients that they started refusing to accept patients and diverting ambulances elsewhere. “This is not sustainable,” said Carl Schultz, emergency medical services director for the Orange County Health Care Agency.
The 393 deaths logged across California on Wednesday also broke the record set Tuesday, when 295 deaths were recorded.
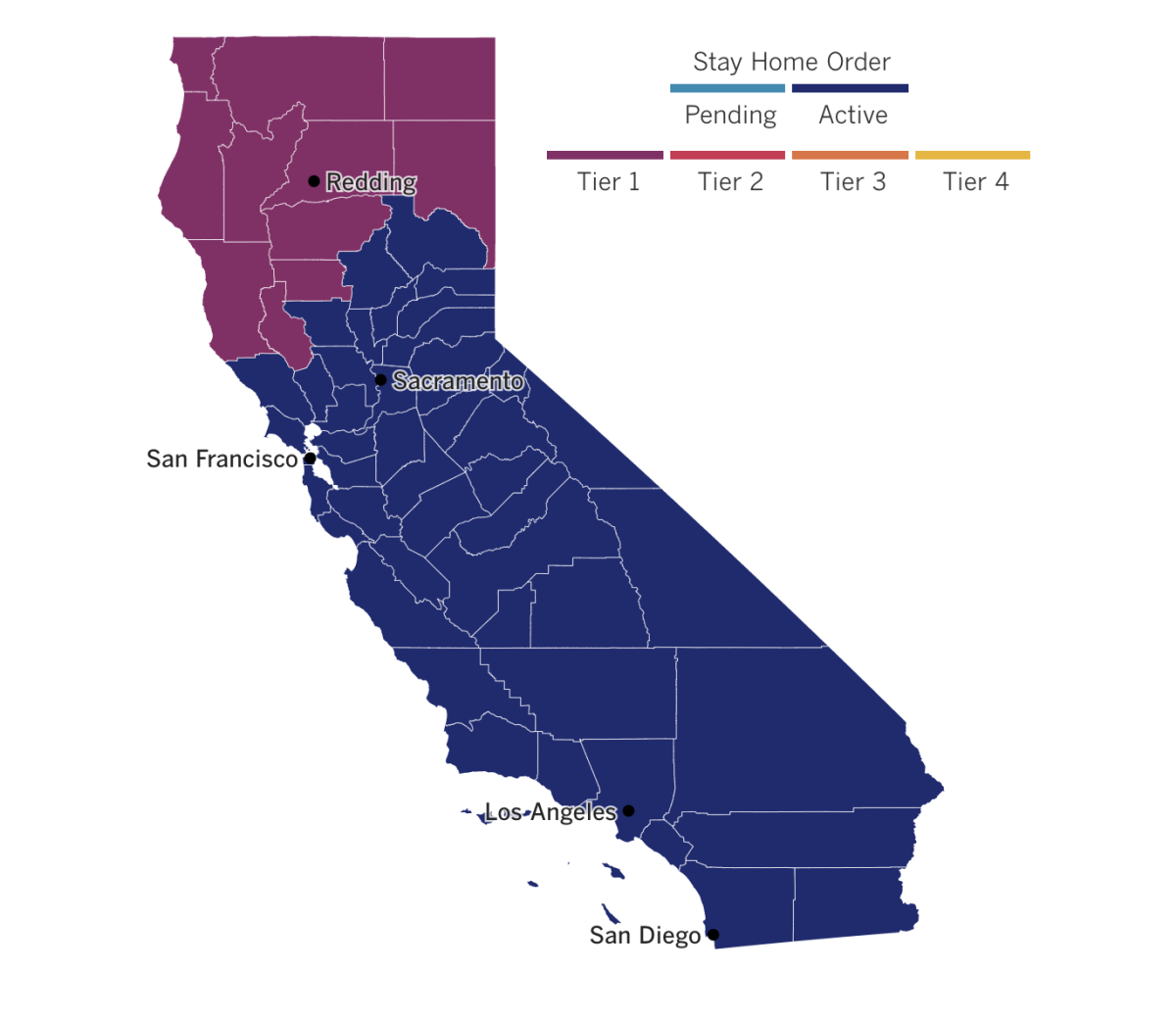
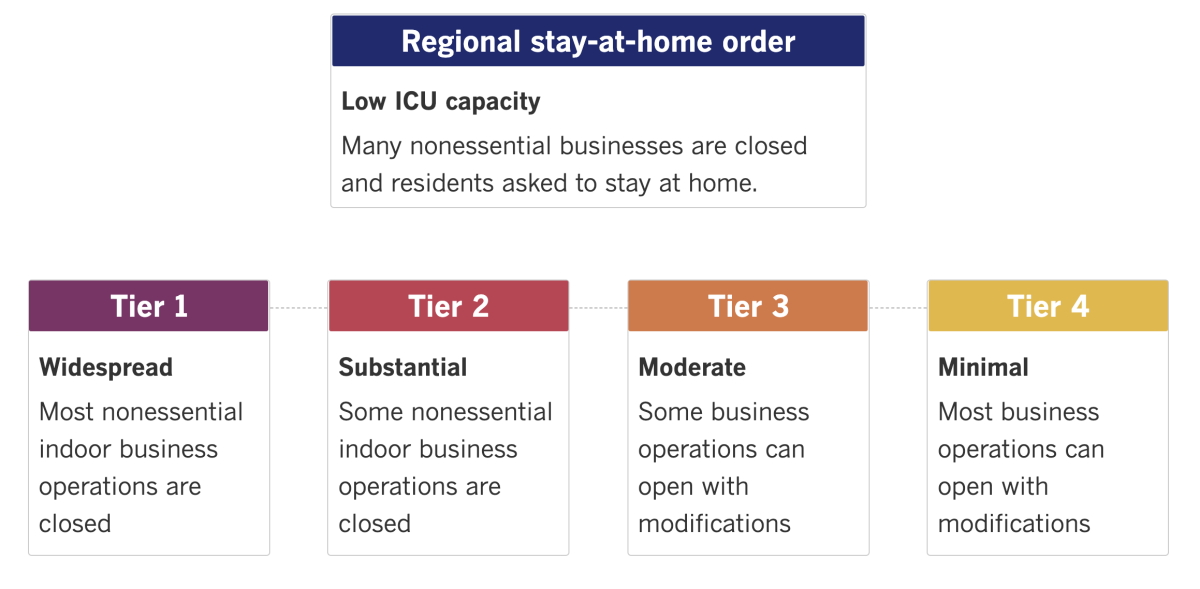
See the latest on California’s coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
A second COVID-19 vaccine has moved one step closer to the waiting arms of millions of Americans. A government advisory panel Thursday endorsed the shot made by Moderna and the National Institutes of Health, voting 20 to 0 that its benefits outweigh its risks for those age 18 and up. (One member abstained.) The Food and Drug Administration is expected to green-light the vaccine for emergency use within a matter of hours or days.
Once authorization is granted, Moderna will start shipping millions of doses that are earmarked for health workers and nursing home residents. The influx of shots would join those from Pfizer and BioNTech, which were authorized last week and were first injected into health workers’ arms Monday. Both vaccines show roughly the same level of protection — 95% for Pfizer, 94% for Moderna — and both require two doses (spaced three weeks apart for Pfizer and four for Moderna).
The review came amid reports of apparent allergic reactions to the Pfizer vaccine in two Alaska health workers. One had a severe reaction that included shortness of breath and the other had less serious side effects including lightheadedness. But the two vaccines, which use the same technology, are not identical, said Moderna chief medical officer Dr. Tal Zaks. “I would not necessarily assume” that any reactions would be the same, he said.
If you’re looking for a vote of confidence, take note: President-elect Joe Biden and Vice President Mike Pence are set to get their COVID-19 shots soon. Transition officials say Biden will receive the vaccine publicly as soon as next week, while the White House says Pence and his wife Karen will get it Friday.
Biden said Dr. Anthony Fauci, the nation’s top infectious-disease expert, advised him to get the vaccine “sooner than later.” The incoming president has said he wants to keep front-line healthcare workers and vulnerable people top priority for vaccination, but he has also noted the importance of getting the shot himself as a way to build confidence among Americans.
“I don’t want to get ahead of the line, but I want to make sure we demonstrate to the American people that it is safe to take,” he said.
Though the arrival of a COVID-19 vaccine was heralded in Great Britain, Canada and the United States, that hasn’t been the case in Russia. In Moscow, clinics that offered shots of the Sputnik V vaccine to healthcare workers and teachers — the first members of the public prioritized to receive it — were reportedly empty.
Sputnik V was touted by Kremlin officials and state-controlled media as a major achievement after it was approved Aug. 11. But many Russians expressed concern that the vaccine was rushed out while still in late-stage testing.
Dzhamilya Kryazheva, a teacher in Krasnogorsk near Moscow, didn’t want to take a chance on the new shot. “I don’t intend to experiment on my body. I have three children,” she said. But for many healthcare workers, the choice to get vaccinated was easy. “Every day, we carry out corpses. What’s there to think about?” said Dr. Marina Pecherkina, an infectious-disease specialist in the eastern city of Vladivostok.
French President Emmanuel Macron tested positive for the coronavirus Thursday after developing COVID-19 symptoms, following a week of meetings with numerous European leaders. Many of them, including the Spanish, Portuguese and French prime ministers, are now in quarantine because they had contact with him.
Macron got tested as soon as symptoms first emerged and will self-isolate for seven days, the Elysee Palace said in a statement. The 42-year-old president will continue to work and conduct state affairs at a distance. His wife, Brigitte, 67, will also be in quarantine. She tested negative on Tuesday and has no symptoms, officials said.
European Union leaders met in person last week in Brussels. Television images showed the leaders wearing masks, generally practicing social distancing and occasionally using hand-sanitizer dispensers in the room.
Your questions answered
Today’s question comes from readers who want to know: If I get the vaccine now, will there be enough available for me to get the required second dose in a few weeks?
Given how officials have stressed that there are very limited supplies of vaccine, it’s natural to wonder whether there’s any risk of running out. But my colleague Noam Levey says authorities have planned for this issue.
Operation Warp Speed, the federal effort to develop and distribute COVID-19 vaccines, is specifically holding back second doses so that there will be enough on hand to give people their second shot.
Health and Human Services Secretary Alex Azar discussed the plan on “Face the Nation.”
“We’re shipping 2.9 million doses of vaccine,” Azar said on Dec. 13. “So whenever they get them in arms, that’s 2.9 million people getting vaccinated. We’re reserving that second dose of vaccine so they can get that later.”
So if you’re one of the first in line to get your shot, there should be a second shot waiting for you in a few weeks. Just be sure to get the same shot that you got the first time — the vaccines can’t be mixed and matched. And make sure you get it in the correct time frame.
It’s crucial that you get that second dose if you want to be protected.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them.
Resources
Practice social distancing using these tips, and wear a mask. Here’s how to do it right.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




