Coronavirus Today: How universal healthcare could save lives
Good evening. I’m Karen Kaplan, and it’s Tuesday, Sept. 13. Here’s the latest on what’s happening with the coronavirus in California and beyond.
The United States accounts for a little more than 4% of the world’s population, but it’s responsible for about 16% of the world’s COVID-19 deaths.
There are lots of reasons why America’s mortality rate is so high: failure to take full advantage of lifesaving vaccines; resistance to simple precautions such as wearing masks in crowded spaces; and high rates of health conditions that make people who catch the coronavirus more likely to wind up severely ill, such as coronary artery disease and obesity
A recent study in the Proceedings of the National Academy of Sciences offers an additional explanation — our lack of universal healthcare.
If the U.S. had a universal healthcare system like the ones in Canada, the United Kingdom, Japan, or pretty much any other high-income country, more than 1 in 4 COVID-19 deaths here could have been prevented, the study authors estimate. That added up to 338,594 avoidable deaths as of March 2022.
The problem isn’t that the U.S. spends too little money on healthcare — indeed, on a per-capita basis, it spends far more than any other country. The problem is that our patchwork system of employer-based health insurance, Medicare for senior citizens and Medicaid for low-income Americans leaves a lot of gaps.
In 2019, just before the pandemic hit, those gaps were so big that nearly 29 million adults had no health insurance at all. Millions more were underinsured, meaning they had some kind of health plan but couldn’t afford the deductibles and copays they’d incur if they tried to use it.
Having so many people with no easy access to health services creates a variety of issues during a pandemic.
People who can’t afford to see the doctor regularly are more likely to develop a chronic health problem that makes them more vulnerable to a serious case of COVID-19. If they catch the coronavirus, they’re less likely to see a doctor or nurse right away and could miss their chance to nip their infection in the bud. Plus, while they’re getting sicker, they’re spreading the virus to others around them.
To make matters worse, the ranks of uninsured and underinsured Americans grew further in the early days of the pandemic. The stay-at-home orders were designed to protect the public’s health by impeding coronavirus spread. But they also forced companies to lay off millions of workers, depriving 14.5 million Americans of employer-sponsored health insurance.

The authors of the PNAS study, led by Alison Galvani of the Yale School of Public Health, performed a series of calculations to estimate the number of lives that could have been saved if the country had a universal healthcare system.
Their starting point was the 973,459 COVID-19 deaths that had been counted in the U.S. as of March. It’s widely acknowledged that many COVID-19 deaths are never reported as such on death certificates, and other researchers had already determined that about 24% of COVID-19 deaths here were missing from official tallies. Based on that, Galvani and her colleagues figured the actual U.S. death toll as of March was 1,282,555.
Four of the study authors had previously estimated that 26.4% of COVID-19 deaths could be blamed on a lack of universal health insurance. That was based on work showing that mortality rates were higher among groups that had less insurance coverage, and that having less insurance was correlated with higher odds of getting COVID-19, especially a serious case that required hospitalization.
When Galvani and the others put it all together, they concluded that 338,594 American lives were lost as of March 2020 because of the way we pay for healthcare.
The research team also estimated that if all COVID-19 hospitalizations had been billed at roughly the same rate that’s used for people covered by Medicare and Medicaid, the country would have saved a whopping $105.6 billion from the start of the pandemic up through March.
“Universal single-payer healthcare is fundamental to pandemic preparedness,” the study authors wrote. Not only would it have saved more lives, they added, but it also “would have done so at lower cost than the current healthcare system.”
By the numbers
California cases and deaths as of 4:50 p.m. on Tuesday:
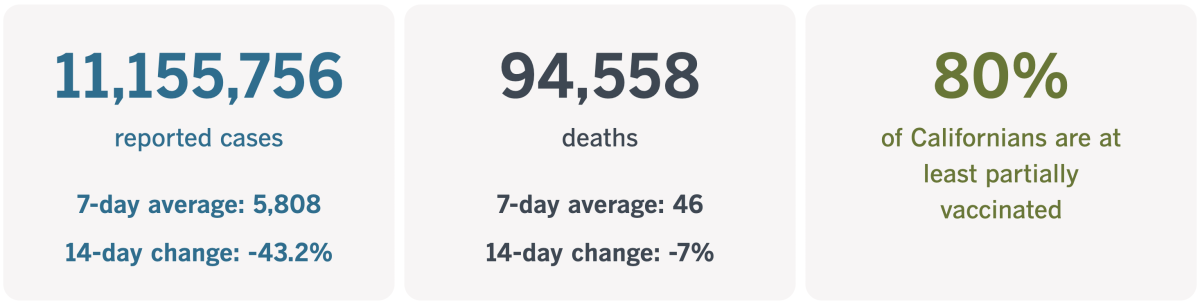
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
The healing power of dance
No one is glad the pandemic came along, but you have to admit it’s brought about certain changes we hope will endure. There’s the ability to keep your job while ditching your commute (as we discussed last week). There’s the proliferation of al fresco dining venues that are so much lovelier than parking spaces.
Melinda Fulmer clued me in to another great example: Dance fitness classes that value enthusiasm over skill. All you have to do is follow the instructor’s moves as best you can.
Classes like these took off during the pandemic. They don’t require specialized equipment or even prior experience. As long as you have a computer or mobile device capable of using a program like Zoom, you can join in.
And people did — from their living rooms, backyards and garages. It was a way to have a communal experience while maintaining a safe social distance. It was also cathartic, a means for turning anger, frustration and grief into happiness and a sense of accomplishment.
“So many of us were really having to face ourselves and be alone with ourselves,” said Emilia Richeson-Valiente, who runs classes from a studio in Glassell Park. “Dance fitness was an accessible medicine for people — a way to get out what we were really feeling and experience some joy.”

Going online during the shutdown not only kept Richeson-Valiente’s operation afloat but also expanded her reach. Her business, Pony Sweat, has more than doubled its Instagram following since the early days of 2020. Thanks to the expanded reach of the internet, the number of people who have taken one of her classes rose by more than 50%.
When dance classes were able to resume in person, the online gatherings continued as well. They allowed far-flung “ponies” (as members of the Pony Sweat community are known) to keep their connections alive. In fact, those relationships were so important that Richeson-Valiente went on tour this summer to meet ponies in Boston, New York City and Philadelphia.
Alyssa Aramanda, who attends classes in the studio, explained why they feel so vital and why so many people have embraced their “distinctly anti-perfectionist vibe,” as Fulmer put it.
“We come and commune here and everything explodes and it’s beautiful,” Aramanda said.
Ponies like her weren’t the only ones who figured out that dance fitness was a way to stay sane while staying in shape during the pandemic.
Before the coronavirus, Dance Church Chief Executive Clara Siegel said 40,000 people had taken classes at her Seattle studio. Today, that number is 144,000. “It has been really incredible,” she said.
Likewise, Sadie Kurzban continued to offer online classes at her New York-based 305 Fitness alongside in-person classes. In fact, demand is so great that she’s launched an instructor certification program.
Richeson-Valiente has expansion dreams too. She’s branched into aural aerobics (where participants hear music and instructional guidance without any visual element) and launched a dance aerobics video zine. She intends to hold more events and foster a community action arm so that Pony Sweat’s core values can be expressed beyond the studio.
After all, she said, “the point of Pony Sweat is for people to discover freedom of movement and expression in their own bodies.”
California’s vaccination progress
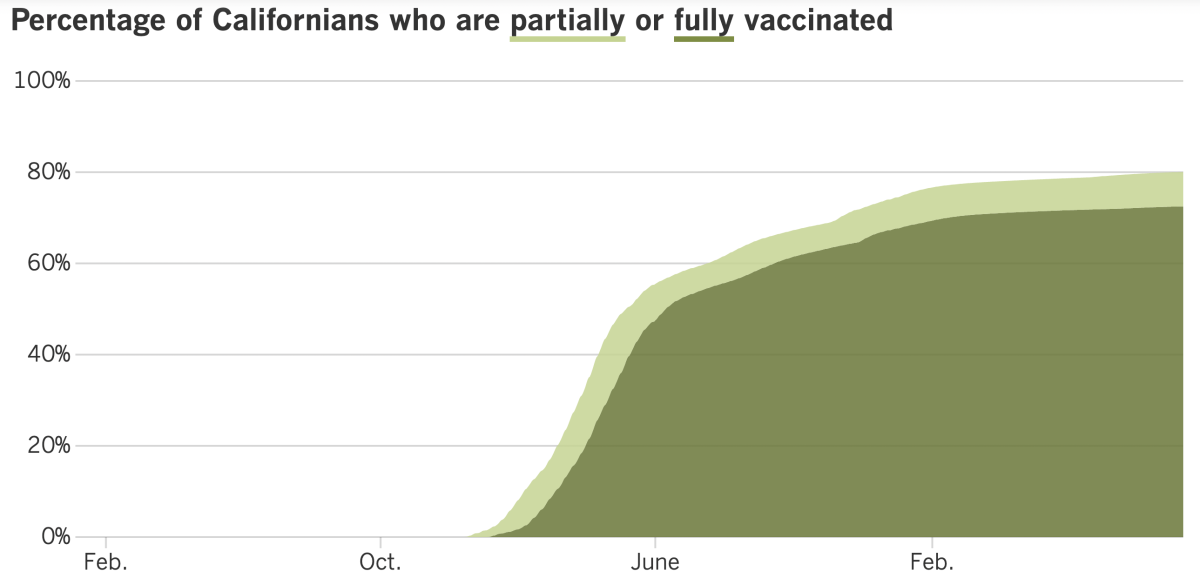
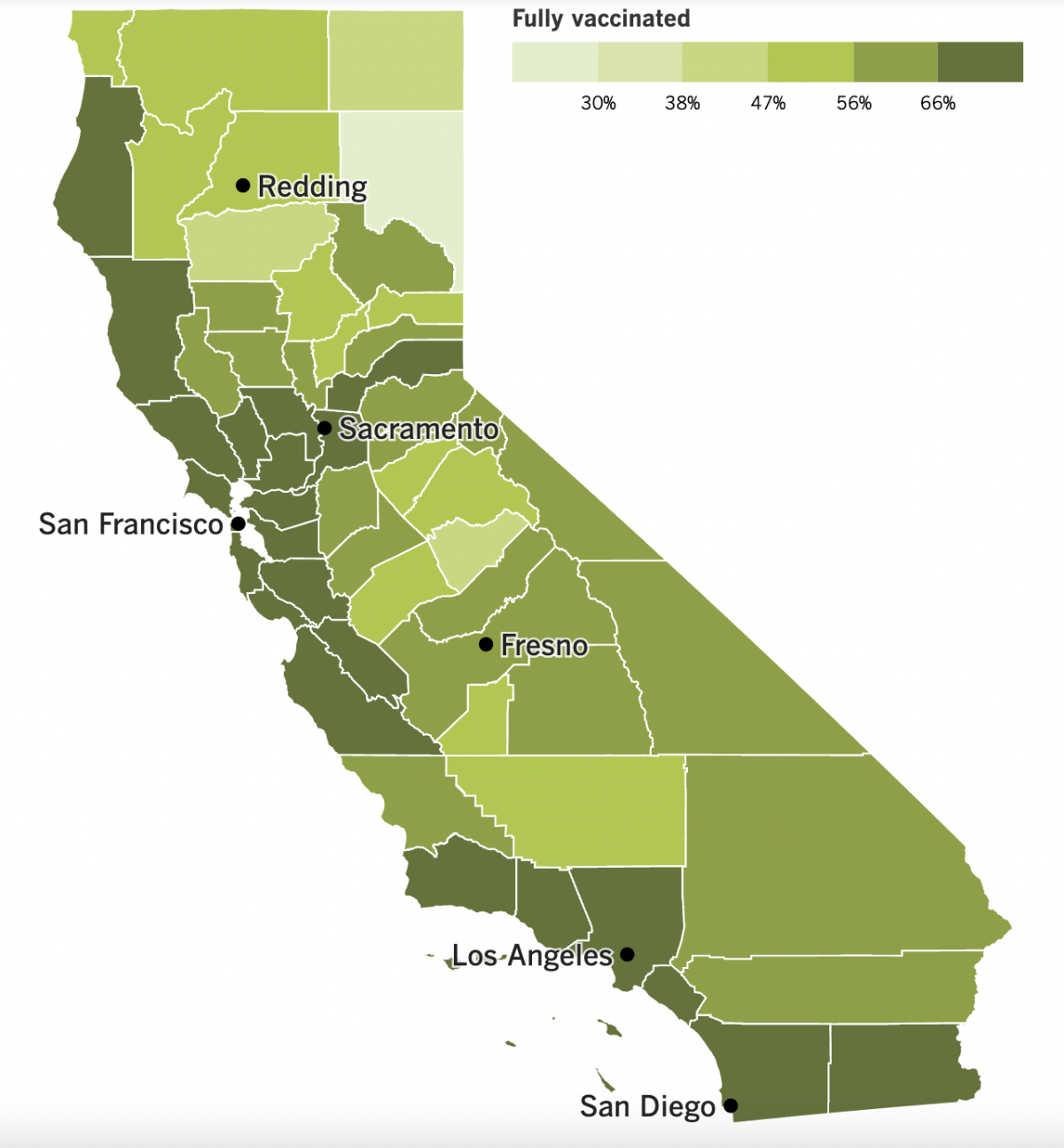
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
It’s time for a pop quiz: What killed the most Los Angeles County residents in the first four months of 2022?
Was it:
a) Car crashes
b) Influenza and pneumonia
c) COVID-19 cases caused by the “mild” Omicron variant
Considering that you’re reading Coronavirus Today, you probably guessed that the correct answer is C. But you might be surprised to learn just how deadly Omicron was.
Between January and April, there were 31.8 COVID-19 deaths for every 100,000 county residents, according to Public Health Director Barbara Ferrer. That compares to 3.5 motor vehicle deaths and 5.9 flu and pneumonia deaths per 100,000 residents during that time.
The figures are based on an analysis of death certificates. And they’re not the only numbers that may prompt you to take Omicron more seriously.
More than 4,800 L.A. County residents have died as a result of COVID-19 this year, a period when versions of the Omicron variant were pretty much the only game in town. The bulk of those deaths involved senior citizens, but 25% occurred in residents younger than 65.
Here’s more reason not to give Omicron the brush-off: The COVID-19 mortality rate for county residents over 80 was three times higher between May and July than it was during the same period last year. For Angelenos between the ages of 65 and 79, the mortality rate during those months was 1½ times higher in 2022 than in 2021.
And Los Angeles isn’t unique. Scientists are cautioning that even though new boosters are here and pandemic precautions are falling by the wayside, the end is not yet in sight.
One reason is that Omicron is particularly adept at evolving new ways to circumvent the immunity people have gained through vaccination and past infections. The up-and-coming subvariant known as BA.4.6 has been making slow but steady progress in wresting market share from BA.5; as of Tuesday, it accounts for about 9.2% of all SARS-CoV-2 coronaviruses circulating in the U.S., up from 8.3% a week ago and 7.5% the week before that, according to data from the Centers for Disease Control and Prevention.
Dr. Ashish Jha, the White House COVID-19 response coordinator, said the disease probably would be with us for the rest of our lives, and other experts warned that it will keep on causing serious illnesses. Even in the best-case scenario where updated boosters are rolled out early and no new variants come along, models predict the country could experience 111,000 deaths between August 2022 and May 2023.
Even when the outbreak is finally under control, the country will still have to tend to the millions who suffer from long COVID. A new research initiative was announced last week to dig deeper into one of the leading hypotheses about what causes the mysterious syndrome — that reservoirs of SARS-CoV-2 lingering in the body are responsible for symptoms that last months or even years.
More than $15 million has been committed to the Long COVID Research Initiative, and the goal is to raise $100 million. Some of the initial funds are from the Chan Soon-Shiong Family Foundation, which is led by Los Angeles Times owner Dr. Patrick Soon-Shiong.
Scientists who receive grants from the initiative will work in their own labs, but they’ll keep one another apprised of their findings and share ideas. The first results are likely to be months away, if not longer.
Speaking of long COVID, a report released Tuesday by the World Health Organization said at least 17 million people in the European Union had experienced the syndrome’s lingering symptoms by the end of 2021.
About 1 in 3 women experienced symptoms that lasted at least three months, including fatigue, breathlessness and cognitive dysfunction, according to the report. The same was true for about 1 in 5 men.
Patients who became sick enough to be admitted to a hospital were much more likely to get long COVID, according to the report. Still unclear is whether the condition is more common among vaccinated or unvaccinated people.
And finally, a deadly earthquake in Sichuan province has prompted rare protests against China’s strict COVID-19 lockdowns.
The magnitude 6.8 quake struck last week, killing at least 93 people and causing extensive damage to homes. Buildings shook in the provincial capital of Chengdu, where 21 million residents were ordered to stay at home after a spike in coronavirus infections. Anxious residents tried to flee their apartment buildings after the shaking stopped, but police and health workers forced them to stay put.
As of last week, about 65 million people in 33 Chinese cities were under varying levels of lockdown. Residents of Wuhan, believed to be the epicenter of the pandemic, protested in front of police even though the Communist Party could sentence them to years in prison for vague crimes such as “picking quarrels and provoking trouble.”
“Lift the lockdown, refuse to be tested,” the residents chanted in videos making the rounds on the internet.
Your questions answered
Today’s question comes from readers who want to know: Should I get the new COVID-19 booster right away or wait until closer to winter?
That’s up to you. But as you make up your mind, experts advise that the greater your risk of serious illness, the sooner you should get the bivalent shot.
“We do hear from people who say, ‘You know, I want to maximize my protection for the late fall and the winter holidays in particular. And I might wait,’” said Los Angeles County Public Health Director Barbara Ferrer. “For people who are in relatively good health and younger, that may be an appropriate assessment.” But for older people and others at higher risk, she added, “I wouldn’t delay.”
Whenever you get the new booster, know that it will take two weeks for it to take full effect. (That’s the same as with previous vaccine doses.) The booster will retain its peak effectiveness for about four or five months after the injection date, said Dr. Peter Chin-Hong, an infectious diseases specialist at UC San Francisco.
That means if you get the booster tomorrow, you’ll be fully protected by the end of the month and can expect to remain that way until mid-January or mid-February.
If the last two winters are any guide, late January and early February will be periods when you’ll want to have strong vaccine protection. In 2021, the country’s seven-day average of new cases peaked on Jan. 14 and began to flatten in late February, according to the CDC’s COVID Data Tracker. In 2022, the peak came on Jan. 15 and remained at pre-surge levels until the last week of February.
Experts expect another wave of cases at the end of the year, but it won’t necessarily follow the previous patterns. Vaccines weren’t available until the first winter surge was in full swing, and the second winter surge was fueled by a coronavirus variant that was a less-than-perfect match to the available vaccine.
The new boosters are a perfect match to nearly 90% of the viral specimens currently in circulation. That could translate into better protection this time around.
“We hope that with this new bivalent vaccine, we might reduce our chances of a third huge winter surge,” Ferrer said.
More than 67,000 Americans are still becoming infected each day, on average. If that makes you nervous, you can’t go wrong by getting the booster now.
Rolling up your sleeve “as soon as eligible seems like a pretty straightforward call to me,” said Dr. Robert Wachter of UCSF. “While some may choose to wait for cases to begin ticking up later in the fall, ‘timing the market’ usually doesn’t work.”
That said, if you’ve had a recent infection, your immune system is already primed and the CDC advises you to wait at least three months to get the booster. Also, if your last dose of vaccine was administered in the last several weeks, you’ll need to wait until at least two months have passed before you’ll be eligible for another one.
When you’re ready to make an appointment, this guide will walk you through the steps.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The woman in the photo above is New Zealand Prime Minister Jacinda Ardern. Her government made news Monday for dropping nearly all of its COVID-19 rules.
No longer will Kiwis be required to wear masks when they go shopping or take public transportation. Nor will they be subject to any vaccine mandates, even if they work in healthcare. Tourists from overseas will be welcomed to the island nation without regard to their vaccination status.
Steps like these would hardly be remarkable in most places, considering that the world seems more than ready to return to its pre-pandemic ways. But New Zealand is different. This is a place that went into a nationwide lockdown last year in response to a single instance of coronavirus spread.
Moves like that helped the country keep its COVID-19 death toll to 65 as recently as late March. Then the Omicron variant sneaked past its defenses, forcing Ardern to acknowledge that the virus would never be eradicated. Even so, New Zealand has recorded fewer than 2,000 deaths among its 5 million residents.
Only two main rules remain in effect: People who test positive for an infection must isolate for seven days, and masks must be worn in hospitals, nursing homes and other healthcare facilities.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




