Coronavirus Today: A COVID milestone for Latinx people
Good evening. I’m Karen Kaplan, and it’s Tuesday, April 19. Here’s the latest on what’s happening with the coronavirus in California and beyond.
Back in 1986, researchers noticed something surprising about Latinx people living in the southwestern United States: Their “health status” was remarkably similar to that of their white neighbors even though their socioeconomic status was significantly lower. The similarities were evident whether you looked at infant mortality, measures of functional health, or the risk of dying of cardiovascular disease or cancer.
Most notably, they reported, life expectancies were slightly higher for Latinx men and women than they were for white residents — in California and Texas, at least.
The findings were so confounding that the researchers dubbed it “an epidemiologic paradox.”
But it wasn’t a fluke. A 2015 Vital Signs report from the Centers for Disease Control and Prevention noted that although Latinx residents were nearly three times more likely than white residents to lack health insurance and had significantly higher rates of obesity (among other apparent disadvantages), their death rate at that time was 24% lower than it was for whites.
Medical experts aren’t entirely sure how to explain this. Usually, having chronic health problems isn’t conducive to a longer lifespan. Nor is it helpful to have less access to healthcare and less money to spend on things to keep your body in good shape, like fresh produce and gym memberships.
Fortunately, Latinx Americans have other things going for them. They’re younger than white residents, on average. They’re much less likely to smoke. The authors of the CDC report also speculated that self-selection works in their favor, since the people who immigrated to the U.S. were probably healthy, and those who were elderly or ill likely returned to their home countries.
Other research suggests a biological edge. As we age, our genes change the way they function. The speed with which those changes occur can be measured with a so-called epigenetic clock, and scientists have found that the clock advances more slowly for Latinx Americans than it does for white Americans.
Whatever the reason for this mortality advantage, it would take a lot to undo it. But the coronavirus may have pulled this off.
A study published last year in the medical journal Lancet found that COVID-19 reduced the average life expectancy of Latinx people in the U.S. from 81.8 years in 2018 to 78 years in 2020. A Latinx baby born in 2020 would still outlive a white baby by about eight months, on average, but that’s far less than the 3.2-year advantage he or she would have had in 2018.
The huge drop reflects the outsize toll COVID-19 has taken on Latinx communities, and especially on working-age adults. The younger the victims, the more years of life that were taken from them — and that means a bigger hit to average life expectancy.
New data from Los Angeles County suggest that by Year 2 of the pandemic, the longevity advantage for Latinx residents had been wiped out.
As my colleagues Andrew J. Campa, Rong-Gong Lin II and Emily Alpert Reyes report, the county’s Latinx residents suffered 756 deaths per 100,000 people last year. That’s up 48% from 2019, when the mortality rate was 511 deaths per 100,000 Latinx residents.
Meanwhile, the mortality rate for white residents increased from 630 to 678 deaths per 100,000 during the same time period. That means Latinx residents absorbed 78 more deaths per 100,000 people than did white residents.
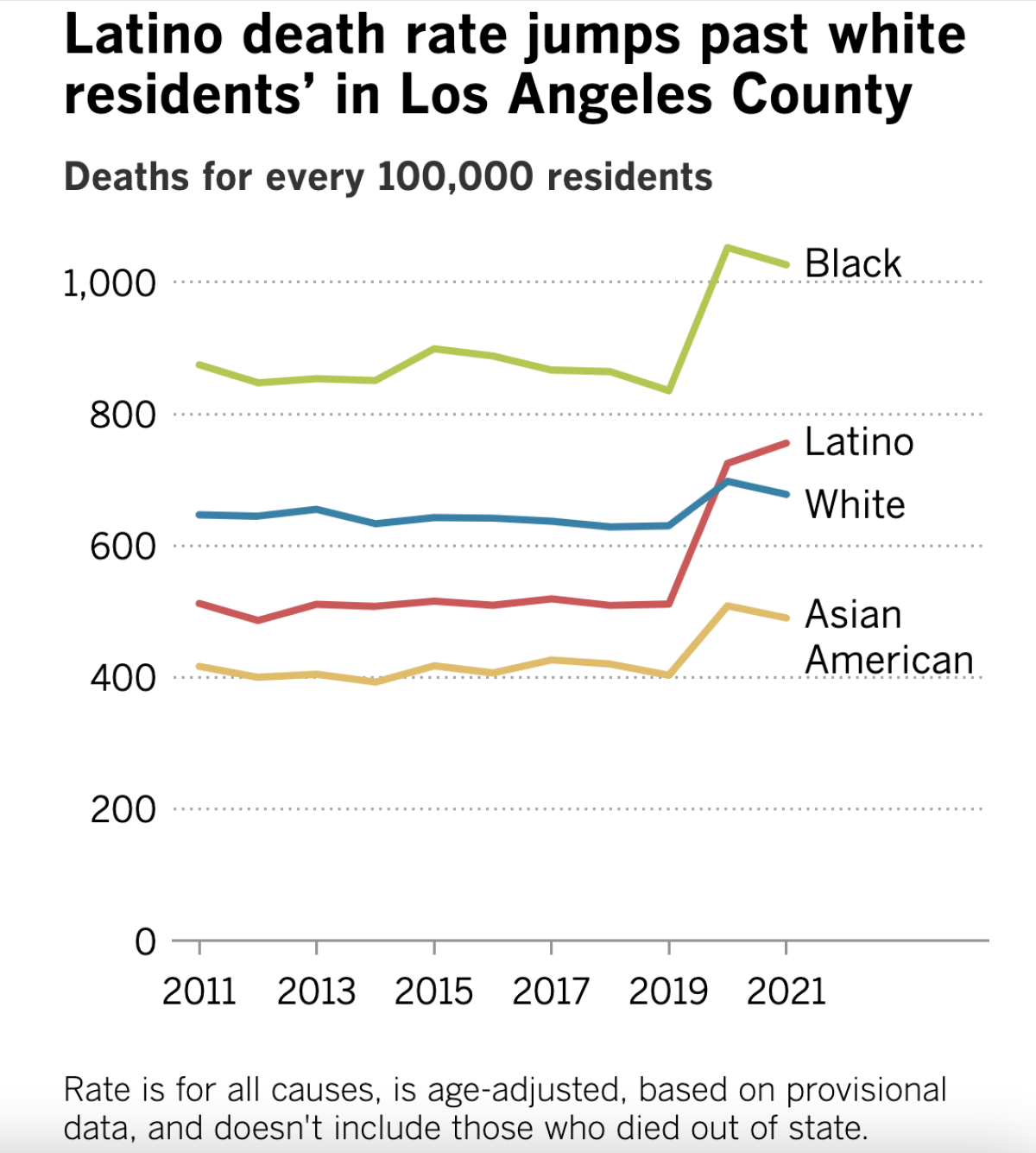
Although Latinx people experienced the largest increase in mortality rate, Black residents had the highest mortality rate both before and after the onset of the pandemic. In 2019, they experienced 835 deaths per 100,000; in 2021, that number rose to 1,027 deaths per 100,000.
Not all of the county’s deaths in 2021 were caused by COVID-19, of course, but the new disease accounts for most of the increase seen since 2019. (A caveat: These mortality rates are based on provisional data and don’t include L.A. County residents who died outside of California. But the figures have been adjusted to account for the age differences among racial and ethnic groups.)
Ironically, some of the factors that allowed the paradox to exist in the first place surely helped erase it once a highly infectious disease was added to the mix. These include the prevalence of tight-knit, multi-generational families who often work together and live under the same roof.
If just one member of the family became infected with the coronavirus, he or she would be primed to spread it to many others — including elderly relatives, who are particularly vulnerable due to their age. And that risk was higher to start with, since Latinx adults were more likely to have jobs that required them to be out in the world instead of holed up at home.
“We work in stores and factories, sell food and clean, and we’re going to run into people,” Carlos Montes, a Chicano activist living in Boyle Heights, told my colleagues. “Being essential [workers] really hurt us because we got sick and then spread it our families.”
Raul Claros, a community organizer who lives in Chinatown, lost his father to a combination of COVID-19 and cancer. Staying a safe distance from his dad was a real emotional challenge for him and other family members.
“We take care of each other’s families because we migrated here together and brought our families here to live,” he said. “It’s the whole village approach.”
It sustained the community for years — until it didn’t, he said: The “village got blown up in 2020.”
By the numbers
California cases and deaths as of 5:35 p.m. Tuesday:
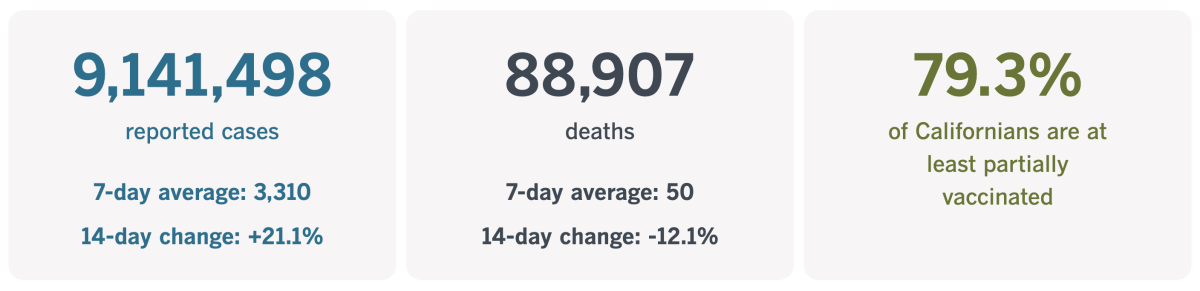
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Why vets are struggling with our pandemic pets
America’s pet population has exploded during the pandemic. Surveys conducted by the American Pet Products Assn. found that 14% of Americans — including 22% of millennials and 25% of Gen Z-ers — had acquired a pet since the coronavirus turned our lives upside-down.
The American Society for the Prevention of Cruelty to Animals has done its own research and estimates that about 23 million U.S. families expanded to include a new dog or cat in the COVID-19 era. And despite early fears that these animals would be abandoned in short order when their novelty wore off, 90% of those dog owners and 85% of the cat owners still had their pandemic pets more than a year into the outbreak.
That’s good news for the critters, and the families that love them. But it means a lot more work for the nation’s veterinarians. And now that we’re in Year 3 of the pandemic, they’re burning out.
When you think of overworked medical professionals, you probably picture nurses triaging patients in a hospital emergency room, or doctors inserting breathing tubes in the ICU. But after reading this story produced by our friends at KQED in partnership with NPR and Kaiser Health News, you’ll be visualizing exhausted vets too.
It’s not just that the number of pets has increased. It’s also that more people have been working remotely, which means they’re spending a lot more time around their pets than they used to. Now they’re noticing coughs, episodes of vomiting and other behaviors that prompt them to call a vet.
Dr. Kathy Gervais works 12-hour shifts at the SPCA’s veterinary hospital in San Francisco. Some patients are puppies or kittens getting checkups and shots. But many of the animals they see are suffering. About five animals are euthanized every day, and the emotional toll adds up.
“I dare you to try to talk to a veterinarian who’s been in practice more than five years who doesn’t know somebody who has committed suicide,” Gervais said. “I, unfortunately, can count on more than 10 fingers: classmates, colleagues, people I’ve dated.”

Surveys bear this out. A 2015 report published by the Centers for Disease Control and Prevention found that nearly 1 in 10 veterinarians suffered “serious psychological distress,” about 1 in 6 had contemplated suicide since joining the profession, and more than 1 in 100 had attempted it.
My colleague Justin Ray spoke with Dr. Carrie Jurney last fall about the pressures she and other veterinarians face on a daily basis.
“I spent a lot of time talking about euthanasia and how sometimes it’s a blessing to help your patients pass peacefully,” Jurney said. “But if you talk about euthanasia every single day as the appropriate way to end suffering, and you yourself are suffering, you can see how there can be some transference there. You can certainly see where a veterinarian who has means can get in a headspace where they start to think that taking their own life is a solution when it’s absolutely not.”
The pandemic has taken the worst aspects of a vet’s job and made them even worse, she said. The high volume of patients means clinic appointments must be scheduled months in advance. Those who opt for an emergency room visit can find themselves waiting for 10 hours or more.
“People who are arriving at an E.R. with a sick animal, they don’t want to hear that it’s a 10-hour wait,” she said. “And so, unfortunately, a lot of people have been really combative recently.”
Jurney is well aware of the toll. In addition to her work as a veterinary neurologist, she is the president of Not One More Vet, a nonprofit based in San Francisco that’s devoted to preventing veterinarian suicides.
Gervais has also stepped up to support her struggling colleagues. She helped organize the Veterinary Mental Health Initiative, which has assisted more than 200 vets and veterinary technicians through support groups and one-on-one services.
In exchange for putting up with the long hours and hostile owners, vets earn an average of about $110,000 per year. That may sound like a lot, but it’s about half the average salary for doctors who treat humans.
If you’re a pet owner, here’s something to keep in mind the next time your animal is unwell:
“Even when you do your job perfectly, you don’t always get to win. Sometimes Mother Nature wins no matter how good you do your job,” Jurney said. “Unfortunately, a lot of grieving pet owners in the last few years decided to take to social media to berate their veterinarian when things don’t go perfectly. It’s a really challenging and stressful situation.”
California’s vaccination progress
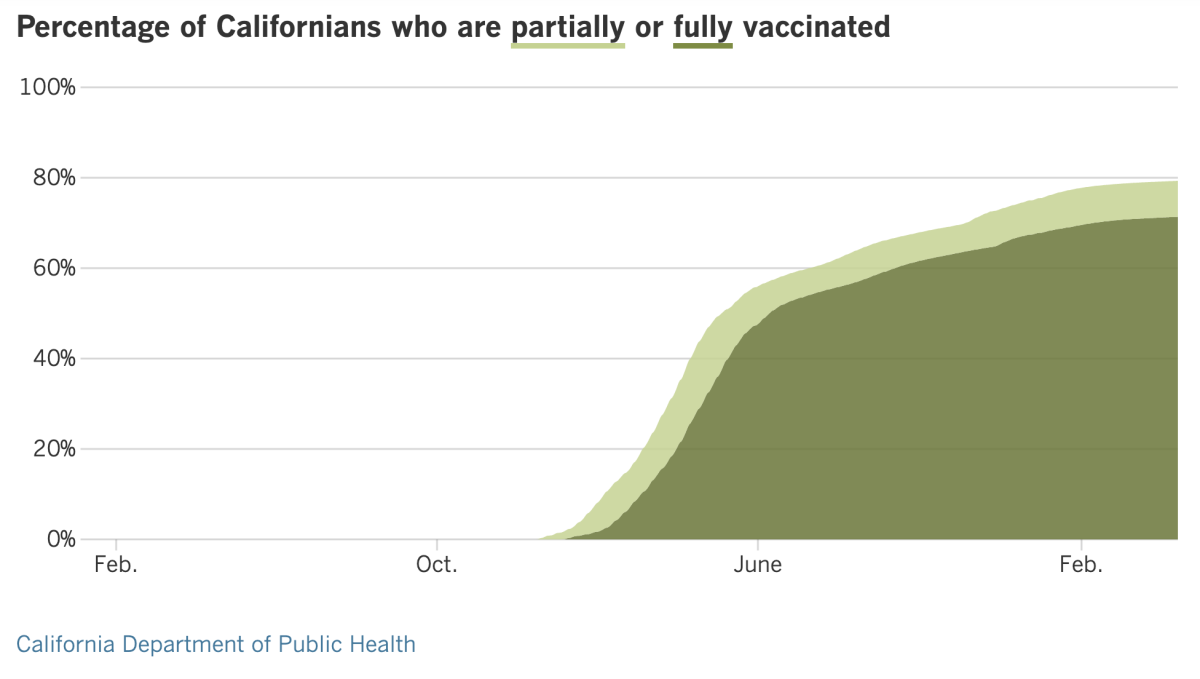
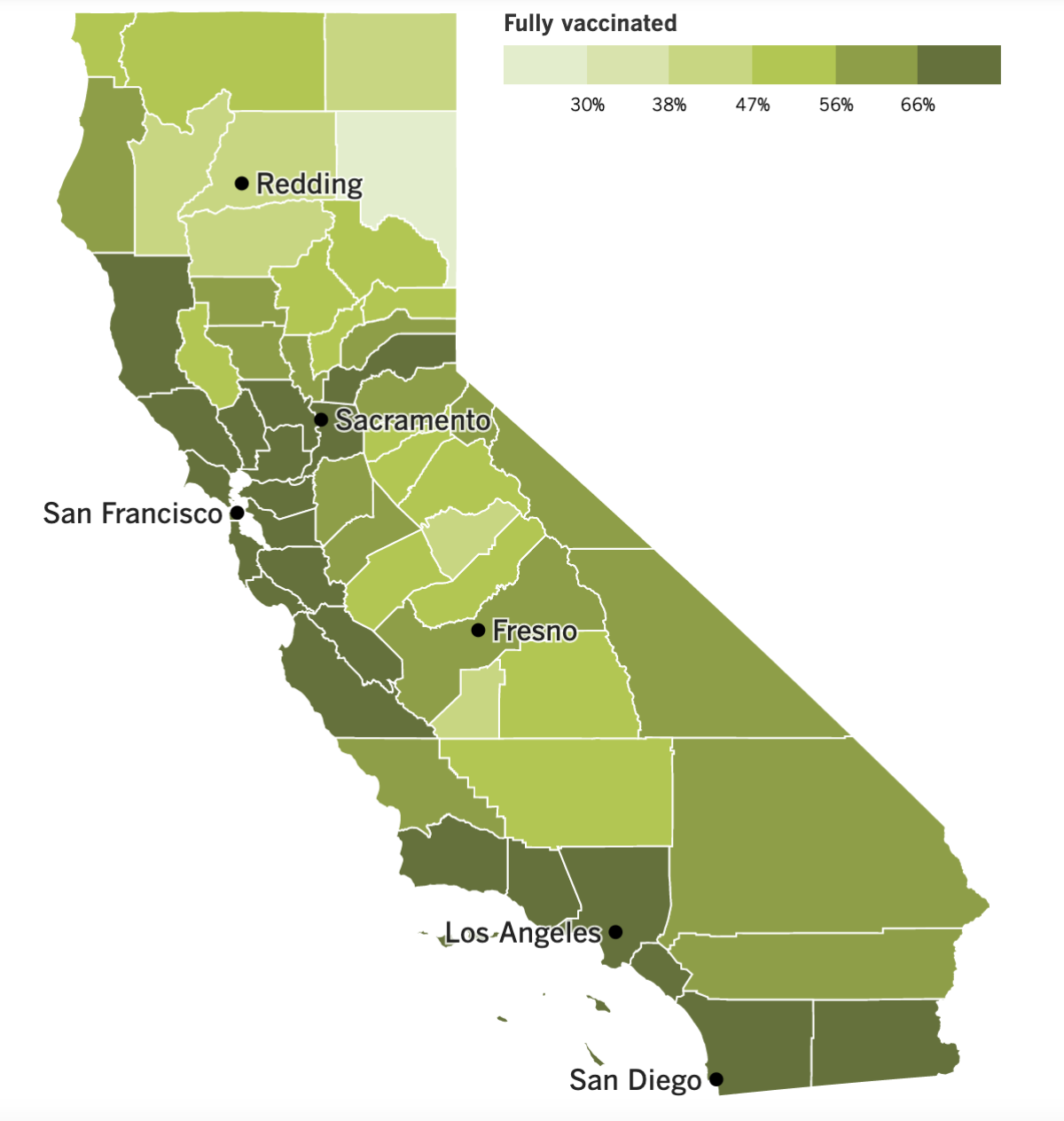
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
The big news this week (so far) comes courtesy of a federal judge in Tampa, Fla., who voided the CDC’s national mask mandate for people traveling on planes, trains, buses and other forms of public transportation.
In a 59-page ruling, the judge said the CDC lacked the authority to issue the mask rule in the first place. U.S. District Judge Kathryn Kimball Mizelle wrote that the agency didn’t follow proper rule-making procedures and failed to justify why masks were needed.
As a result, the White House acknowledged that the mask order “is not in effect at this time.” The Justice Department asserted that the order was “a valid exercise of the authority Congress has given CDC to protect the public health.” Even so, it said it won’t appeal the ruling unless the CDC decides that “a mandatory order remains necessary for the public’s health.”
The upshot is that, for now, individual operators can decide for themselves whether to keep mask mandates in place for their employees and customers. Several large airlines — including American, United, Southwest, Delta and Alaska — have already opted to stop policing mask use.
“Masks are no longer required on domestic flights, select international flights (dependent upon the arrival country’s requirements) or at U.S. airports,” United Airlines wrote in a tweet that included photos of a towering dinosaur sculpture at O’Hare International Airport, seen with and without a face covering. “More comfortable keeping yours on? Go right ahead … the choice is yours (you look dino-mite either way)!”
In California, the Metrolink commuter rail service system made mask use optional on its trains and in its stations “effective immediately,” though it reminded riders that the CDC’s advice was still to keep masks on while indoors. The Bay Area Rapid Transit rail system ended its mandate once the Transportation Security Administration acknowledged the CDC’s rule was no longer in effect.
Other transit agencies, including the L.A. County Metropolitan Transportation Authority and the L.A. Department of Transportation were more upfront about asking riders to keep wearing masks for the time being.
Other pandemic rules are being rolled back as well. As of Wednesday, California is no longer recommending that people quarantine for five days after being exposed to the coronavirus, as long as they remain asymptomatic. State officials made the change to help employers and other institutions that were inconvenienced when apparently healthy workers were required to stay home. (Anyone who develops COVID-19 symptoms following a coronavirus exposure, or who tests positive for an infection, should still isolate at home for at least five days.)
Local health officials can keep the older, stricter rules in place if they so choose. L.A. County modified its quarantine guidance on Friday to largely align with the state’s. But there are a few extra conditions here: For 10 days after exposure, people who were in close contact with an infected person must wear “a highly protective mask” whenever they’re around other people. They’re also required to get a coronavirus test three to five days after their last exposure to the infected person.
Another difference: The old quarantine rules remain in place for people in high-risk settings like jails, homeless shelters and assisted living facilities.
In another easing, state officials decided last week to delay a requirement that students get a COVID-19 vaccination before starting the next school year. The first-in-the-nation vaccine mandate for students made headlines when it was announced in October, with the caveat that it wouldn’t go into effect until at least one vaccine for children 12 and older received full approval from the Food and Drug Administration. Since that hasn’t happened yet, Gov. Newsom said the soonest the state mandate would go into effect is July 1, 2023.
Kelly Gonez, president of the Los Angeles Board of Education, said she was “disappointed to see the state pushing back their timeline” because vaccines protect the community and only about 67% of California’s children 12 to 17 years old are vaccinated.
L.A. Unified had planned to implement its own vaccine mandate in January but opted to delay enforcement until the start of the next school year to avoid forcing thousands of students into independent-study alternatives. Now it’s unclear whether the district will postpone the mandate again.
Speaking of vaccines, Pfizer said it had new data showing that 5- to 11-year-olds would benefit from a COVID-19 booster shot. That data came from a study of 140 kids who received a booster six months after they were fully vaccinated. In general, the booster revved up their immune response; in a subset of 30 children who were analyzed more closely, their virus-fighting antibodies increased by a factor of 36. All of this information was conveyed in a news release and hadn’t been vetted by independent scientists.
Moderna is testing a new COVID-19 booster shot that combines its original vaccine with another designed to target the Beta variant. The company said people who received its combo shot produced more antibodies capable of fighting several variants than did people who got the regular booster. The results “really give us hope” that the company can design a shot aimed squarely at Omicron, said Dr. Jacqueline Miller, a Moderna vice president. These results were posted online and hadn’t been reviewed by outside experts either.
Good news for those who aren’t fond of sticking a swab into their nose every time they have a COVID-19 symptom: The FDA has issued an emergency use authorization for a device that can detect the coronavirus in a sample of your breath.
The InspectIR COVID-19 Breathalyzer isn’t meant for home use — you’ll have to find one at a hospital, doctor’s office or mobile testing site. In tests, the device correctly identified positive test samples 91.2% of the time and correctly flagged negative samples 99.3% of the time. Results were available in less than three minutes.
And finally, the CDC unveiled a new center Tuesday that it hopes will be able to forecast future disease outbreaks the way the National Weather Service forecasts storms.
The Center for Forecasting and Outbreak Analytics aims to solve some of the data collection problems that have hampered the government’s response to COVID-19, perhaps by adopting the kinds of population sampling practices used in the United Kingdom and elsewhere. Improving access to data from state governments and from hospitals would also help, its leaders said.
“Better data and analytics will give us better responses to protect all Americans,” said Dylan George, the center’s new director of operations.
Your questions answered
Today’s question comes from readers who want to know: Where can I go to participate in the “Test to Treat” program?
Test to Treat is a Biden administration initiative designed to streamline access to COVID-19 care. It allows a person to get tested for a coronavirus infection and, if the result is positive, get immediate access to prescription pills that greatly reduce the risk of becoming severely ill.
Los Angeles County, which launched its version of Test to Treat about a month ago, now has more than 70 participating locations, including 20 CVS MinuteClinics and 11 Walgreens drug stores. It’s also available at Children’s Hospital Los Angeles, City of Hope in Duarte, Keck Hospital of USC near Boyle Heights, Ronald Reagan UCLA Medical Center in Westwood, Western University of Health Sciences in Pomona, and a variety of community hospitals, urgent cares, clinics and pharmacies.
The L.A. County Department of Public Health has a complete list of options here. You can also call (833) 540-0473 for assistance.
If you’re going to a CVS, the county advises you to start with an E-Clinic appointment, which you can request online.
To find a Test to Treat location anywhere in the country, type your address or ZIP Code into the search bar on this site from the U.S. Department of Health and Human Services.
The all-in-one program is not just about convenience. The two medications the program offers — Paxlovid from Pfizer and molnupiravir from Merck — work best when started as soon as possible after COVID-19 symptoms start. If it’s been six or more days since your symptoms began, you’ll need to be treated with intravenous drugs instead, according to Dr. Franklin Pratt, a senior physician with the public health department.
That said, it’s not necessary that you get tested at the Test to Treat location. If you confirmed a coronavirus infection at another testing site, or by using an at-home test, you can bring your test results with you and be evaluated for a prescription, which can be filled immediately.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The lovely photo above, of people celebrating the Easter Vigil Mass at the Cathedral of St. Paul in Minnesota, looks entirely normal. And that’s what makes it so remarkable.
For many Christian congregations, Sunday marked the first time since 2019 that they had gathered together in their houses of worship to celebrate one of their holiest days. Easter 2020 occurred just weeks into the country’s initial lockdowns, and virtual services were still a thing a year later as the country was recovering from the devastation of its first pandemic winter.
Easter 2022 was different.
“We hadn’t seen a crowd like this for two years,” said John Faison, senior pastor at Watson Grove Baptist Church in Nashville, where about 700 worshipers gathered Sunday (with masks). “Eyes were lighting up. People just felt good.”
Nearly 4,000 congregants came to pray in the newly renovated sanctuary of Purpose Church in Pomona. The full 150-member choir, band and orchestra participated in Sunday’s services for the first time in two years.
“It’s a sweet homecoming in so many ways,” said Tina Tong, worship producer for the 152-year-old nondenominational congregation.
COVID-19 safety protocols that called for good-quality masks and social distancing were in effect at Christ Church Lutheran in Minneapolis, but those were minor inconveniences in the scheme of things.
“The gift of being in the same physical space for the first time in three years is so grounding and beautiful,” said pastor Miriam Samuelson-Roberts. “We do not take it for granted.”
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




