Coronavirus Today: The (potential) upside of Omicron
Good evening. I’m Karen Kaplan, and it’s Friday, Dec. 17. Here’s the latest on what’s happening with the coronavirus in California and beyond.
Let’s be real: Almost everything we hear about the Omicron variant sounds scary. It seemed to come out of nowhere just a few weeks ago and already accounts for well over half of coronavirus cases in London. In South Africa, it reduced the effectiveness of the Pfizer-BioNTech vaccine to just 33%. In California, it’s infecting people who are not only fully vaccinated but got their booster shots too.
Even its name sounds a little too much like “ominous.”
But many scientists who are looking at the early Omicron data are feeling a little ... well ... hopeful.
“Is this the end of the pandemic?” asked one of them, University of Johannesburg coronavirus analyst Pieter Streicher.
Why does he think that’s even a possibility? It boils down to two apparent attributes of the Omicron variant: It spreads like wildfire, and it’s less likely to make people severely ill.
As my colleague Melissa Healy explains, a strain that is both highly transmissible and much less virulent is exactly the type that becomes an endemic “nuisance virus.” It never goes away, but it doesn’t do that much damage.
Four other coronaviruses — ones that cause the common cold — have already achieved this status. They make their hosts sick enough to cough or sneeze out infectious particles but not so sick they stay home and miss the chance to spread those germs to others. Each infection leaves some immunity in its wake, but most people remain susceptible most of the time. The virus and humanity reach a stalemate.
“That’s what we all hope,” said Dr. Stanley Perlman, a University of Iowa virologist who has studied coronaviruses for decades.
The preliminary findings about Omicron are based on population studies from South Africa and experiments conducted in labs. Observations from countries around the world back them up, but it will be another week or so before there’s enough hard data to be convincing.
Thus far, COVID-19 death rates across South Africa have dropped considerably despite the Omicron wave. If that continues to be the case for the next two or three weeks and there is no massive surge in hospitalizations, it “may well mark turning point in [the] pandemic,” according to Dr. Shabir Madhi, an infectious-disease expert at the University of the Witwatersrand.
Some scientists insist that kind of thinking is premature. Omicron’s behavior in the U.S. may be different than its behavior in South Africa, since the population there is much younger, among other differences.
Plus, Omicron’s propensity to spread may negate its lighter touch: If the variant is half as likely to make people severely ill but twice as transmissible, it’ll be a wash.
And then there’s the ever-present possibility that a new mutation will come along and change the game again. The coronavirus could become easier to contain — or it could make things worse.
William Hanage, an epidemiologist at Harvard’s School of Public Health, is among those who aren’t ready to breathe a sigh of relief.
“Only a fool would bet against Mother Nature,” he said.
By the numbers
California cases and deaths as of 4:28 p.m. Friday:
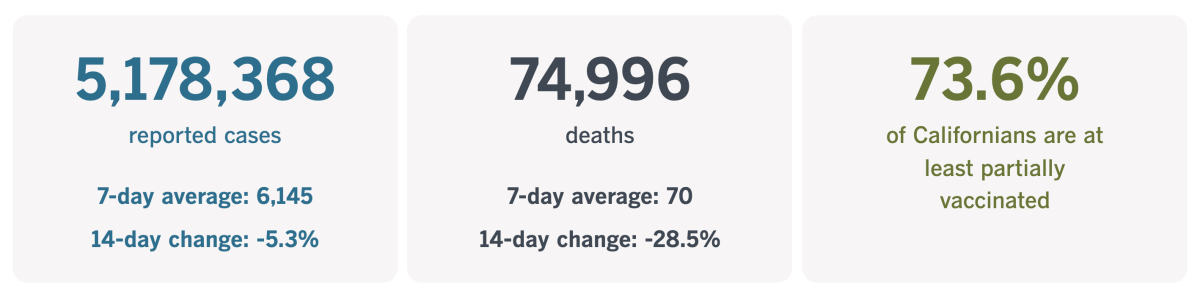
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Another pandemic casualty: upward mobility
Someday, the pandemic will be over. But for many of those who lost loved ones, life will never return to normal. It’s not just the emotional toll of knowing that parents, spouses or other cherished people are gone for good. It’s the way their absence affects the trajectory of their lives.
Janelly, Melanie, Leanna and Sergio Ayala — all of them 10 or younger — are in this unfortunate category. Their father, 37-year-old Sergio Ayala, died of COVID-19 in January. In addition to being a doting parent, he was a breadwinner with a good job as a field supervisor at his brother-in-law’s pest control company. He was also taking steps to become a barber and own his own business.
Once that dream was fulfilled, he had planned to start college savings funds for all four of his children. His partner, Lizeth Sanchez, was going to go back to school and study sociology. Instead, she will stick with her job at a medical device manufacturing company. She worries that she’ll only be able to send one of their children to college.
The family Sergio Ayala left behind is hardly alone, my colleague Alejandra Reyes-Velarde reports. In California, COVID-19’s victims include a disproportionate share of younger Latinos — people whose families relied on them for financial support.
There are a variety of reasons why COVID-19 has been particularly unkind to this demographic. To name a few: They’re more likely to work in essential jobs that increase their exposure to the coronavirus; they have higher rates of conditions like obesity and hypertension that are associated with severe COVID-19; and they are more likely to live in crowded and multigenerational homes, increasing the risk that if one family member catches the coronavirus, others will too.
When you add it all up, Latinos in California have lost roughly 370,000 years of potential life due to COVID-19, according to UCLA biostatistics researcher Jay Xu.
Some of those years would have been spent making families more financially secure and creating opportunities for upward mobility. Instead, those left behind will be struggling just to stay where they are and hoping they don’t fall further behind.
Prior to the pandemic, about 38% of Latinos in California were in the middle class, and more than half were in the lowest income bracket, according to a report from the California Latino Economic Institute. Thanks to the pandemic, many of those in the first category have slipped into the second.
A survey by the Pew Research Center found that, a year into the pandemic, 44% of Americans said either they or someone in their household had lost a job or taken a pay cut because of the pandemic. Among Latinos, that figure was about 60%.
When Latinos struggle, the whole state struggles.
“If Latinos are left behind, that’s going to have a significant impact on California’s overall economy,” said Mindy Romero, a political sociologist at USC. “You can’t leave behind your most populous community.”
Sanchez will do the best she can for her children, without Ayala’s help. But deaths like his have the potential to widen the class divide in the decades to come.
California’s vaccination progress
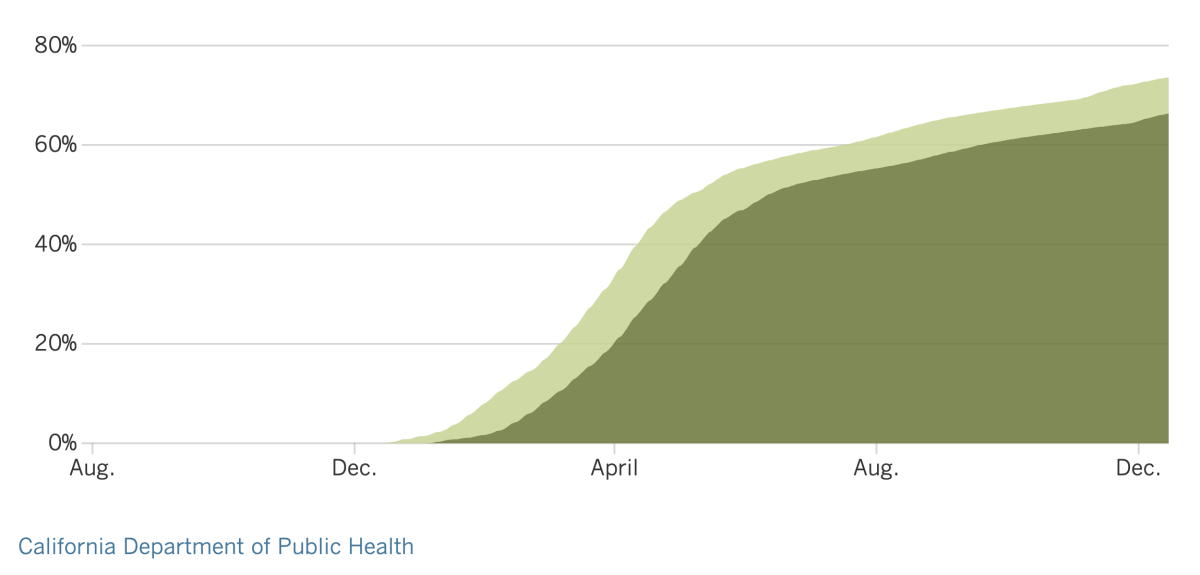
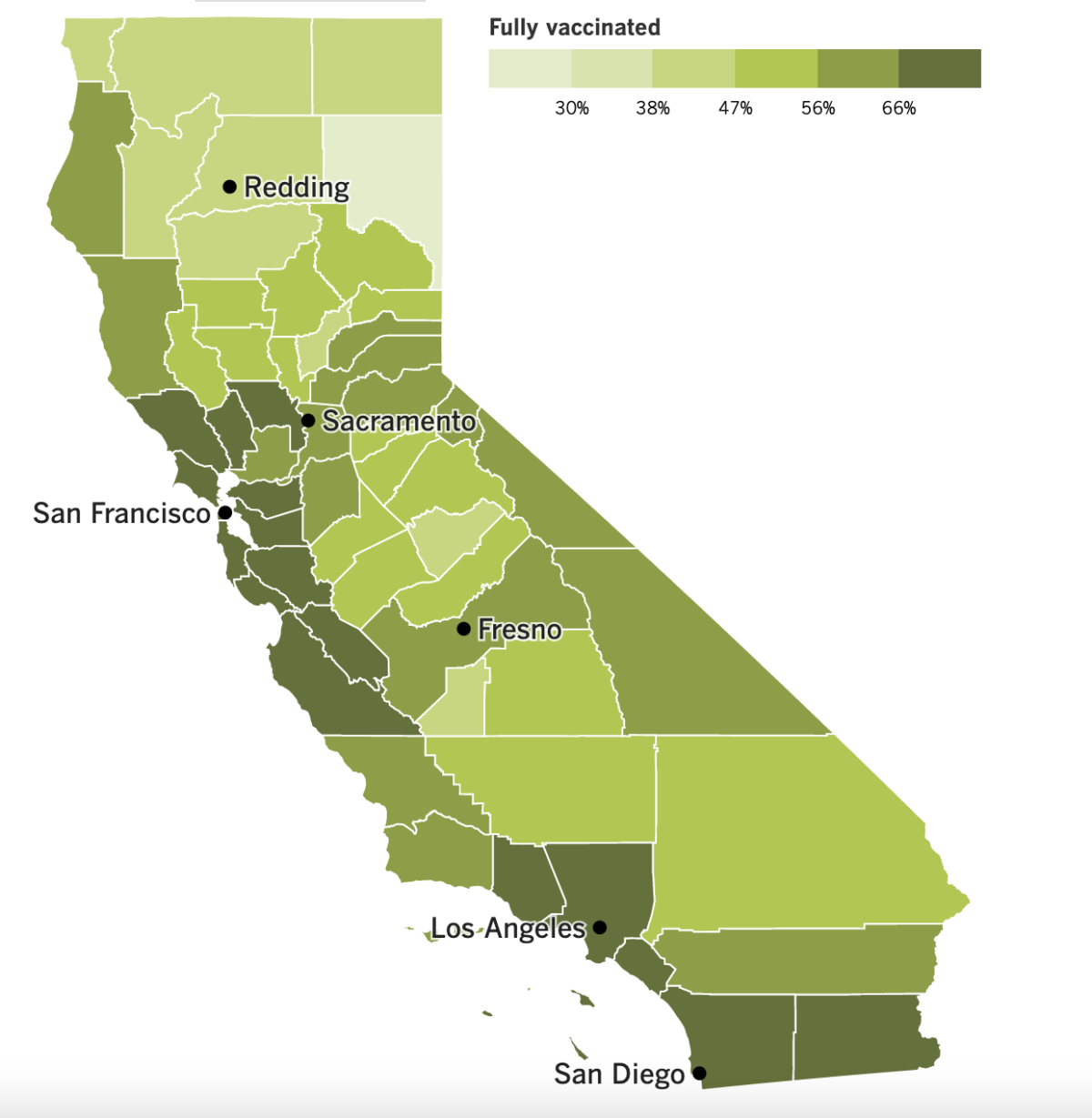
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
Winter is coming.
That “Game of Thrones” warning also applies to the real world, where the rapidly spreading Omicron variant and the destructive Delta variant are threatening to overwhelm hospitals in the coming weeks.
California’s COVID-19 forecasting models show that a winter surge could be worse than this summer’s Delta wave, which stretched hospitals to their limits in much of the state.
“We will, in fact, see a pretty significant surge in our cases,” said Los Angeles County Public Health Director Barbara Ferrer.
That’s already happening in Riverside County, which hasn’t had a break since patients sickened by Delta began filling hospitals months ago. It’s been so bad that patients have had to wait up to five hours just to be transferred from an ambulance gurney to a bed in the ER, said Bruce Barton, director of emergency management there.
Colder weather and holiday gatherings could make the situation even worse. And if patients go to hospitals, they’re likely to find them short-staffed because exhausted employees have left the industry.
The combination of Delta and Omicron is “a perfect storm for overwhelming our hospital system that is already strained,” said Dr. Regina Chinsio-Kwong, a deputy health officer for Orange County.
The problem isn’t limited to California. Omicron cases in the U.S. are doubling about every two days, said Dr. Rochelle Walensky, director of the Centers for Disease Control and Prevention. The CDC says there could be more than 1 million new coronavirus cases next week; around Halloween, there were 500,000 in a week.
President Biden didn’t mince words when he described the threat on Thursday: “For [the] unvaccinated, we are looking at a winter of severe illness and death,” he said. That was followed by the usual pitch to protect yourself and others by getting vaccinated and boosted.
Infections are also spiraling in the United Kingdom, hitting record highs. That prompted France to tighten entry rules for travelers from the U.K. In addition, Greece and Italy tightened entry requirements for all visitors this week while Portugal extended stricter border controls that were already in effect.
In the Netherlands, where a partial lockdown has been in place since November, the government ordered elementary schools to begin Christmas break a week early in hopes of heading off an Omicron surge. Dutch leaders also followed Britain’s lead by accelerating their booster shot campaign.
Back in the U.S., the CDC is easing up on schools by backing “test-to-stay” policies that let students remain in classrooms after they’ve been exposed to an infected person — but only if the exposed students are asymptomatic and test negative for a coronavirus infection. The CDC says the change will minimize disruptions for students without putting them at increased risk.
Previously, the guidance was for students to quarantine at home for 10 days if they came in close contact with an infected person. As of Friday, both policies are considered viable options. (Some schools may want to continue with quarantines because the monitoring needed for test-to-stay can be costly.)
The CDC said its decision was influenced by the experience of school districts in Chicago and L.A. County, which kept case rates in check when they implemented test-to-stay policies. L.A. Unified was not one of them — more than 2,000 LAUSD students enter quarantine in a typical week — but the nation’s second-largest school district was already planning to shift to a policy like the one endorsed by the CDC.
The CDC also made a change to its COVID-19 vaccine recommendations, saying Americans would be better off with either the Pfizer-BioNTech or Moderna shots than with the one from Johnson & Johnson. The updated advice was based on a reassessment of the risk of developing rare but serious blood clots after getting the J&J shot, as well as a recognition that the other vaccines have proved more effective.
Until now, all three vaccines were treated as if they were equally good. The fact that the J&J offering came in a single dose was expected to be an advantage, since it offered a simpler path to full immunization. But it hasn’t proven nearly as popular as its two-dose counterparts: Of the more than 200 million Americans who are fully vaccinated, only about 16 million got the J&J shot.
Although it’s not preferred, the J&J vaccine will remain an option for Americans who aren’t comfortable with the Pfizer and Moderna mRNA vaccines.
And speaking of the Pfizer vaccine, a very-low-dose version being tested in 2- to 4-year-olds did not prompt a strong enough immune response after two shots, the company said. The company will now test three doses to see if protection improves.
The dosage being tried is one-tenth the adult dose, and Pfizer said it had no plans right now to increase it. The two-dose version for 5- to 11-year-olds is one-third the adult dose.
It’s not clear how long this setback may delay a COVID-19 vaccine for the youngest children. If the three-dose series is shown to work in a clinical trial, Pfizer and BioNTech said they’d seek emergency use authorization sometime before the end of June 2022.
Your questions answered
Today’s question comes from a reader who wants to know: How do I report a business that isn’t checking to see whether customers are fully vaccinated?
The reader who sent in this question said she’d been inside restaurants, coffee shops, salons and shopping centers in Los Angeles and wasn’t asked to show proof of vaccination as required under the SafePassLA program, which went into effect on Nov. 8.
For the first three weeks of the program, officials were issuing warnings instead of fines. The goal at the time was to educate businesses about what they were expected to do in order to increase compliance. As of Nov. 23, however, repercussions kicked in, with a first violation generating a warning and a second resulting in a $1,000 fine. Repeat offenders could find themselves racking up $5,000 fines for each offense.
Inspectors with L.A.’s Department of Building and Safety are tasked with enforcing the vaccine requirement — and they welcome your tips. You can fill out a form on the city’s SafePassLA website. Be prepared to provide the name and address of the delinquent business, along with your name, phone number and email address.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
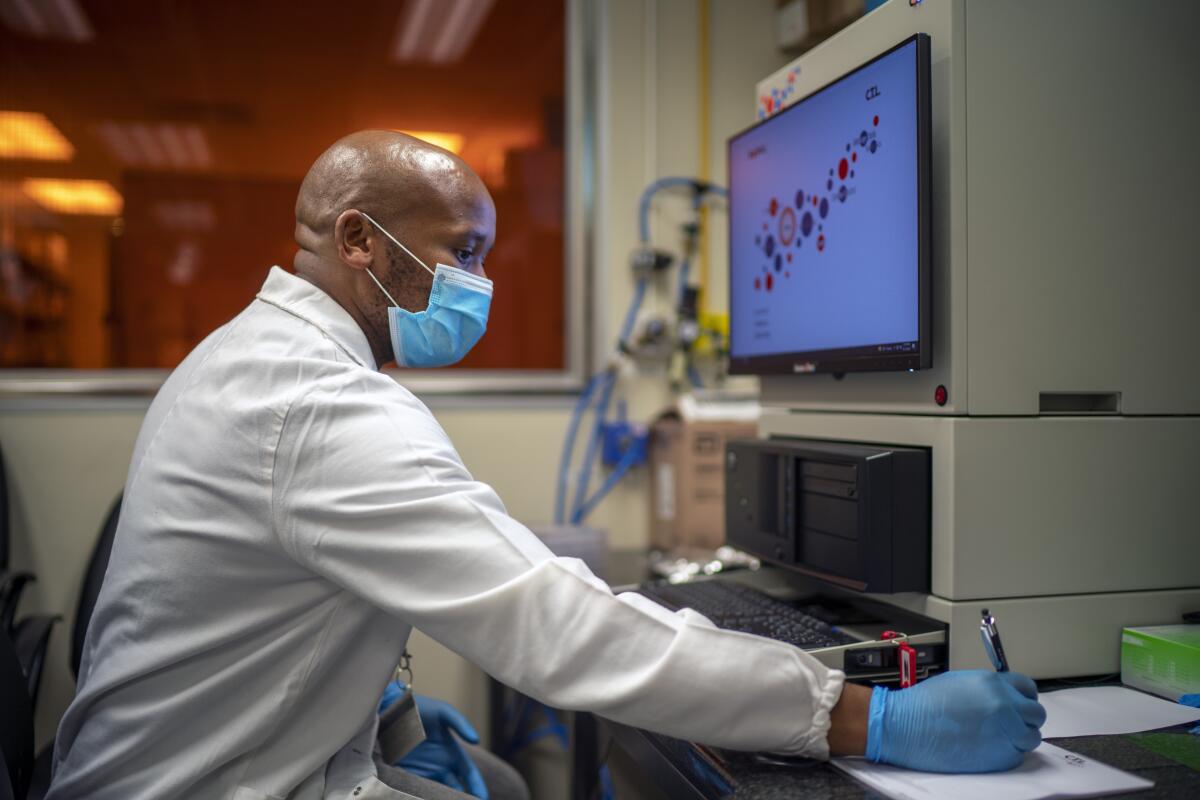
The pandemic in pictures
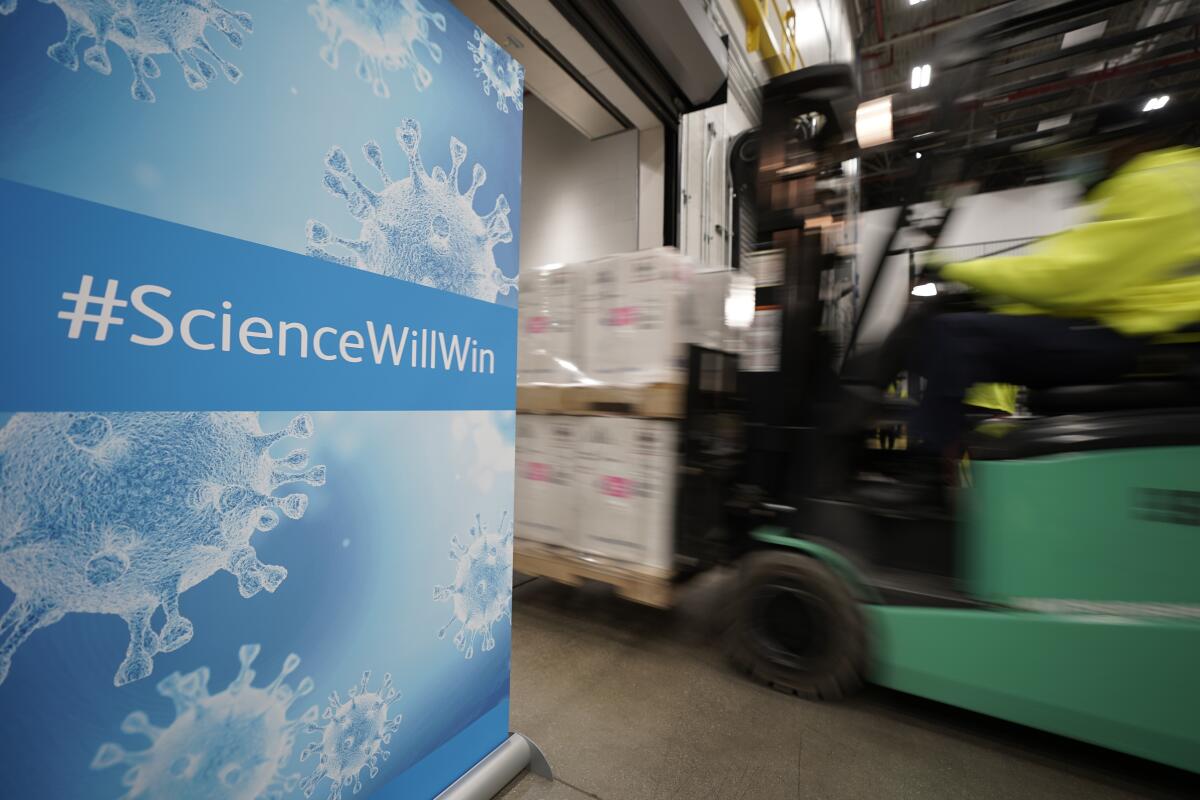
This picture was taken just over a year ago as the biggest immunization drive in American history got underway. It’s from a Pfizer manufacturing plant in Michigan, and the green forklift speeding by is moving boxes of COVID-19 vaccine.
After losing 300,000 Americans in less than a year, health officials were thrilled to see injections going into arms. It seemed like nothing short of a miracle that the shots — along with similar ones produced by Moderna — were developed in a matter of months and were at least 94% effective in clinical trials.
A year later, the U.S. death toll from COVID-19 stands above 800,000 despite the widespread availability of multiple vaccines. People who are fully vaccinated are 14 times less likely to die of the disease than people who are unvaccinated, according to the CDC. But numbers like that have a hard time breaking through the wall of misinformation that has scared millions of people away.
Dr. Francis Collins, director of the National Institutes of Health, said he and other experts underestimated how the spread of misinformation could hobble the “astounding achievement” of the vaccines.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




