Coronavirus Today: Homeless people persuade their peers to get vaccinated
Good evening. I’m Karen Kaplan, and it’s Tuesday, Oct, 19. Here’s the latest on what’s happening with the coronavirus in California and beyond.
COVID-19 is a contagious disease. Luckily, enthusiasm for the vaccines that prevent it can be contagious too.
Don’t believe it? Then check out this story by my colleague Emily Alpert Reyes. She reminds us that even though ardent anti-vaxxers are the ones seeking attention, there are still plenty of unvaccinated Americans who can be persuaded to get the shots.
That’s especially true when the message comes from someone they know — which is why the Los Angeles County Department of Health Services is recruiting “peer ambassadors” to help them with their mission.
“Peers are able to communicate with their peers and build trust at an exponentially quicker and easier rate than we can,” said José Mata, a member of the county’s Housing for Health COVID Response Team. “We’ve seen peers convince people who have told us no — repeatedly.”
This particular effort is aimed at the county’s homeless population, which has lost at least 244 people to COVID-19 since the start of the pandemic, according to the L.A. County Department of Public Health.
As of late September, roughly 57% of unhoused people were at least partially vaccinated against COVID-19. That’s well below the countywide rate, which now stands at 69.4% according to the Times Tracker.
The peer ambassadors are people who live in tents, RVs and makeshift shelters. Some of them begin proselytizing within hours of getting vaccinated themselves.

That was the case for Zack Gustine, a former radio personality who recently got the Johnson & Johnson vaccine while sitting in front of his RV in Lincoln Heights. That same day, he was calling out to his friend Kimberly Conti from outside her former bookmobile.
“Have you gotten vaccinated already?” Gustine asked her. “Do you want to?”
When Conti expressed ambivalence, Gustine said he’d felt the same way. But when a nurse in red scrubs showed up outside his door, he realized that taking advantage of the opportunity was “kind of a no-brainer.”
“We bring it right to you,” Gustine assured Conti. “It’s super easy.”
Conti agreed.
Gustine also paid a visit to a friend in a tent draped in gray and blue tarps and asked her whether she’d been vaccinated yet. If she got the shot today, she would get a gift card, he said.
She said yes — and soon, she was calling out to others along the street: “Hey, you want to get a shot?”
By the end of the day, Gustine had persuaded four people to get vaccinated. At one point, he said he was disappointed that he couldn’t persuade even more. But he also seemed to recognize what he was up against.
“All of the people out here, basically, they’re scared of any big institutions of any kind,” he said. “You’re not going to undo a lifetime of that in, like, five minutes.”
By the numbers
California cases and deaths as of 5:45 p.m. Tuesday:
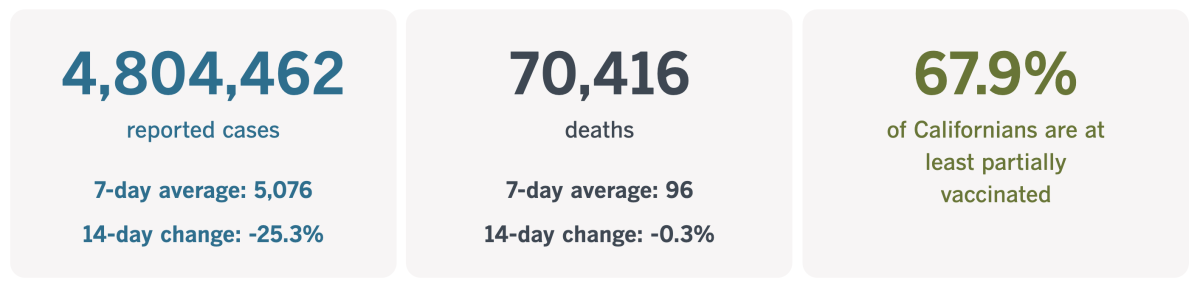
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Japan offers a glimpse of an alternative reality
What would it be like if people stopped resisting COVID-19 vaccines and got vaccinated? Take a look at Japan.
Tokyo, the capital city that is home to nearly 14 million people, is routinely reporting fewer than 100 new coronavirus cases per day. Residents are once again able to crowd onto trains, congregate in bars, and pretty much carry on with their regular lives.
As recently as mid-August, the city was reporting nearly 6,000 new cases per day. The Tokyo Olympics had just wrapped up, and the Delta variant was still expanding its footprint.
Health officials are still piecing together the story of how things turned around so dramatically. But at this point, they seem certain that COVID-19 vaccines have played a critical role.
That fact is a little surprising, considering Japan’s track record of vaccine wariness. The country has a history of fixating on the apparent side effects of immunizations rather than the much larger disease-preventing benefits.
For instance, about a decade ago, the Japanese government began promoting the HPV vaccine for adolescent girls. The shot blocks the dominant strains of the human papillomavirus, which are responsible for roughly 70% of cervical cancer cases.
At first, the vaccines were rolled out regionally, and more than seven in 10 eligible girls got them. But within weeks of being included as part of the national immunization program, reports emerged of girls “having difficulty walking or controlling their movements,” as a study in the medical journal Lancet put it. Their stories garnered tons of media coverage that was more emotional than analytical; indeed, it turned out the problems were unrelated to the HPV vaccine.
Still, the public’s reaction prompted the Japanese Ministry of Health, Labour and Welfare to suspend its efforts to promote the shots, and the immunization rate plummeted to less than 1%. The Lancet study estimates that the rejection of HPV vaccines over a six-year period resulted in at least 24,600 additional cases of cervical cancer and 5,000 preventable deaths.
That story helps explain why Japanese officials insisted on testing COVID-19 vaccines locally even after they’d been vetted through large-scale international trials. A study of the Pfizer-BioNTech vaccine involving just 160 Japanese people wasn’t big enough to provide much useful data, but it still delayed the shots’ rollout in the months leading up to the Olympics.
It took until May 10 for the country to vaccinate just 1% of its population, and it crossed the 10% mark on June 23, according to Our World in Data. By then, nearly 45% of Americans were fully vaccinated. But as vaccinations here have leveled off, they’ve continued to climb in Japan. Today, 67.9% of the Japanese population is fully vaccinated, compared with 56.3% of people in the U.S.
Importantly, the immunizations are not concentrated among senior citizens. Younger and middle-aged adults who are more likely to gather with people from other households have embraced the shots as well, experts say.

“Rapid and intensive vaccinations in Japan among those younger than 64 might have created a temporary condition similar to herd immunity,” Kazuhiro Tateda, a virologist at Toho University in Tokyo, told the Associated Press.
Other factors certainly contributed, including a general willingness to mask up. (Wearing masks was a common practice even before the pandemic.) And though Japan never had full lockdowns, people stayed away from crowded nightlife areas as the Delta variant sent the nationwide number of new cases above 23,000 per day. (In earlier surges, that figure never even reached 6,500.)
But the role of COVID-19 vaccines can’t be ignored. Dr. Hiroshi Nishiura of Kyoto University credits the shots with averting 650,000 coronavirus infections and 7,200 deaths between March and September.
If the U.S. had the same vaccination rate as Japan, the number of fully immunized Americans would increase by 38.6 million. Just imagine how many infections and deaths would be prevented here in that scenario.
California’s vaccination progress
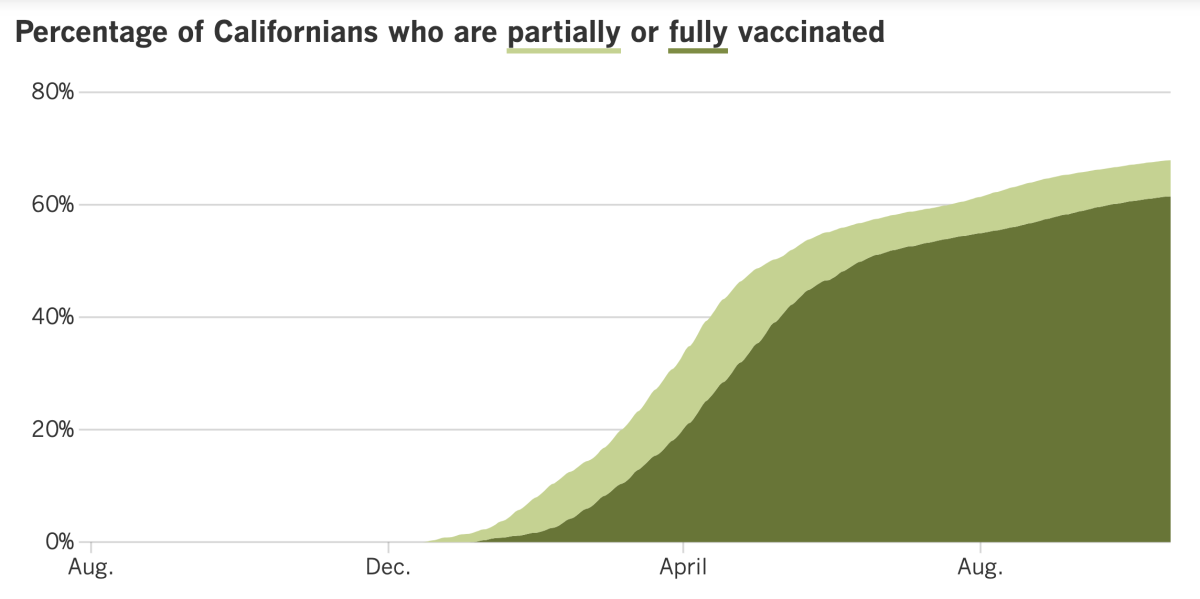
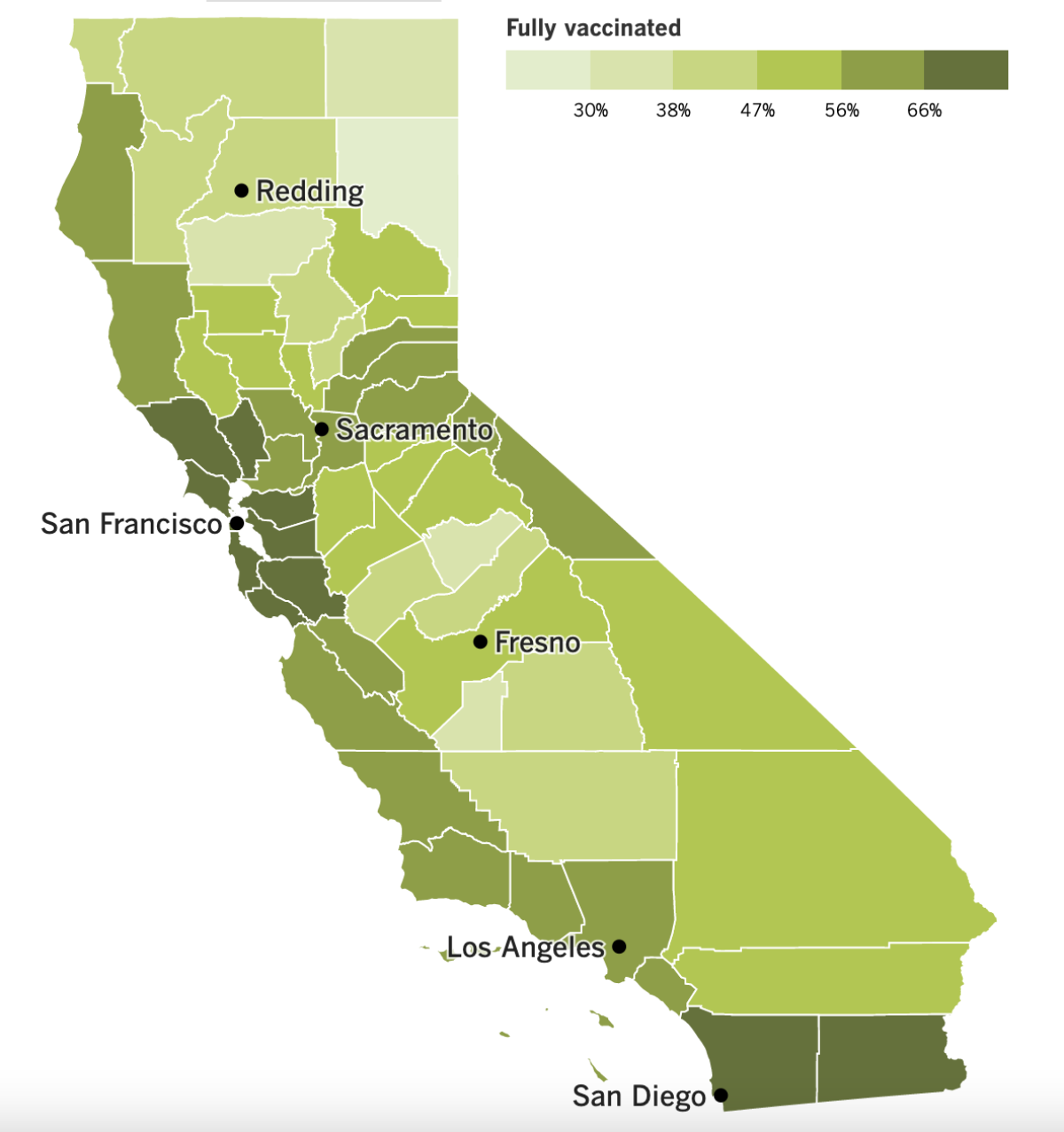
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
Los Angeles Unified has something to teach us about vaccine mandates: They work.
Faced with the prospect of losing their jobs, thousands of vaccine-hesitant school district employees opted to get a last-minute shot before the deadline on Friday. As a result, 97% of all employees were eligible for work on Monday. The high compliance rate included those who were granted exemptions for medical or religious reasons.
Even better: 99% of classroom teachers are now at least partially vaccinated. So are 99.4% of those who belong to the administrators union.
About 500 members of United Teachers Los Angeles — which includes teachers, librarians, counselors and nurses — opted not to get vaccinated and could lose their jobs. Roughly half of those unvaccinated workers are teachers.
LAUSD employees who are only partially vaccinated now have until Nov. 14 to get their second shot.
The high vaccination rates meant the nation’s second-largest school district didn’t need to deploy thousands of supervisors and staff to school campuses and classrooms.
Are you paying attention, L.A. City Council?
On Tuesday, city officials put forward a plan to extend their vaccine mandate one more time. The deadline for city workers to get vaccinated had been set for Wednesday, but the plan would change that to Dec. 18. Employees who remain unvaccinated after that date would face “corrective action” — though it’s not yet clear what that would be.
The extension must be approved by the City Council to go into effect. Columnist Steve Lopez hopes that it won’t.
“Either Mayor Garcetti or the City Council, or both, need to reject this take-your-time vaccination plan, quit coddling and get tough,” Lopez writes. “Does anyone have a spine?”
The city’s vaccine mandate was issued in August, triggering lawsuits from police officers and firefighters. If the extension goes through, it will be the latest example of local politicians doing the bidding of the police and firefighter unions, Lopez writes.
He adds that the majority of local cops and firefighters have rolled up their sleeves, and that a vocal minority of “flat-Earth fools” is undermining the public’s trust in all of them.
Washington State University football coach Nick Rolovich refused to comply with a vaccine mandate in his state, and on Monday he lost his job as a result.
The Cougars’ head coach had been the highest-paid employee in Washington state, with a salary of more than $3 million a year. Apparently, that wasn’t enough of an incentive to get immunized.
Rolovich had applied for a religious exemption to the mandate, though he wouldn’t explain his reasons for wanting one. Four of his unvaccinated assistant coaches were fired as well.
“This is a disheartening day for our football program,” athletic director Pat Chun said in a statement. “Our priority has been and will continue to be the health and well-being of the young men on our team.”
Finally, COVID-19 has claimed a high-profile and beloved victim: former Secretary of State Colin Powell.
Powell was vaccinated, but he was battling a type of blood cancer called multiple myeloma that weakens the immune system. In addition to leaving him more vulnerable to infections, it also meant his body wasn’t well equipped to produce a robust response to the vaccine. Studies have found as few as 45% of people with this cancer develop sufficient levels of coronavirus antibodies after getting the vaccine.
Doctors and public health officials fretted that Powell’s breakthrough infection would discourage people from getting vaccinated. But Dr. Ed Lifshitz, medical director of the Communicable Disease Service at New Jersey’s Health Department, said that was the wrong lesson to take away from this loss.
“The way that you help those who are most vulnerable is by not letting the virus get to them in the first place,” he said, “and the best way to do that is to go out there and get vaccinated.”
Your questions answered
Today’s question comes from readers who want to know: Can I get a COVID-19 booster shot designed for the Delta variant?
Maybe someday, but not yet.
In principle, it wouldn’t be hard to make a vaccine (or booster) that targets the Delta variant in particular. Companies could follow the same recipe as before, except instead of using the genetic code of the original coronavirus strain as the main ingredient, this time they’d get the sequence from Delta.
The Food and Drug Administration has said that new versions of existing vaccines made to target variants would not have to repeat all of the same testing their predecessors were subject to. They could get a nod from regulators after being tested in a few hundred people over the course of two or three months — provided the streamlined trial demonstrated that the modified vaccine was more effective against the variant than the original vaccine.
Pfizer and Moderna are testing vaccines that have been modified for Delta, but neither has asked the FDA to authorize their use. And scientists say there’s little need to do so, since the original vaccines are still doing their job of reducing people’s risk of becoming seriously ill with COVID-19.
In addition, their booster shot tests have shown that a third dose using the original vaccine recipe stimulates the immune system to make more coronavirus-fighting antibodies that are perfectly capable of fending off the Delta variant.
Changing the vaccine production process is a big deal, and it should only be done “when it’s really necessary,” said FDA vaccine chief Dr. Peter Marks.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
Resources
Need a vaccine? Keep in mind that supplies are limited, and getting one can be a challenge. Sign up for email updates, check your eligibility and, if you’re eligible, make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




