Coronavirus Today: CDC changes its mind on masks (again)

Good evening. I’m Karen Kaplan, and it’s Tuesday, July 27. Here’s what’s happening with the coronavirus in California and beyond.
For the record:
9:57 a.m. July 28, 2021An earlier version of this newsletter misstated the CDC’s definitions for levels of coronavirus transmission in a community. The threshold for “substantial” transmission is more than 50 new cases per week per 100,000 people, not 50 new cases per day, and “high” transmission is more than 100 new cases per week per 100,000 people, not 300 new cases.
Remember how excited you were when the Centers for Disease Control and Prevention said that fully vaccinated people could ditch their pesky face masks in most situations. Well ...
Thanks to the thriving Delta variant and the millions of Americans who haven’t seen fit to get vaccinated, the CDC changed its official mask advice yet again Tuesday and urged people to wear masks in indoor public places even if they’ve been immunized.
The new guidance applies to parts of the country where the virus is spreading dangerously. In CDC-speak, that means counties where transmission rates are “substantial” (more than 50 new cases per week per 100,000 residents) or “high” (more than 100 new cases per 100,000 people).
Los Angeles County is one of those places with high transmission rates, but since we already have an indoor mask mandate, the guidance won’t have much effect. With roughly two-thirds of the nation’s counties subject to the new guidance, however, changes are likely elsewhere.
California health officials are reviewing the new CDC advice but have not yet decided whether to adjust the state’s rules. Almost all Californians live in a county with substantial or high transmission rates. That includes the entire southern third of the state, except for San Luis Obispo County.
Gov. Gavin Newsom has been asked repeatedly about the possibility of a new statewide mask recommendation or mandate in recent weeks. His typical response is to say neither will be necessary if more Californians get vaccinated. But if that doesn’t happen, the CDC action may provide him some political cover to take a more aggressive approach.

The new federal attitude toward masks comes just 10 weeks after the CDC told the country it was safe for fully vaccinated Americans to stop covering their faces in most indoor settings. New data about so-called breakthrough infections involving the Delta variant prompted the agency to update its advice.
Data collected since January indicate that viral loads in some vaccinated people with asymptomatic Delta infections “are quite similar” to those of infected people who have not been vaccinated, said Dr. Rochelle Walensky, director of the CDC. Viral loads are considered a reliable proxy for a person’s ability to transmit the virus.
Medical and public health experts who have seen the emerging evidence “universally said this required action,” Walensky said, and she reluctantly agreed.
“I know this is not a welcome piece of news,” Walensky said. “Not only are people tired, they’re frustrated.”
White House Press Secretary Jen Psaki defended the CDC for altering its mask guidance “based on evolving data.”
“That’s what they should be doing,” she said.
This is hardly the first time the CDC has changed its mind about masks. If you think really hard, you might remember way back to February 2020, when the U.S. surgeon general fired up his Twitter account and urged Americans to “STOP BUYING MASKS!”
For a part-entertaining, part-infuriating walk down memory lane, be sure to check out our timeline of the CDC’s ever-changing advice on face masks.
By the numbers
California cases, deaths and vaccinations as of 7:20 p.m. on Tuesday:
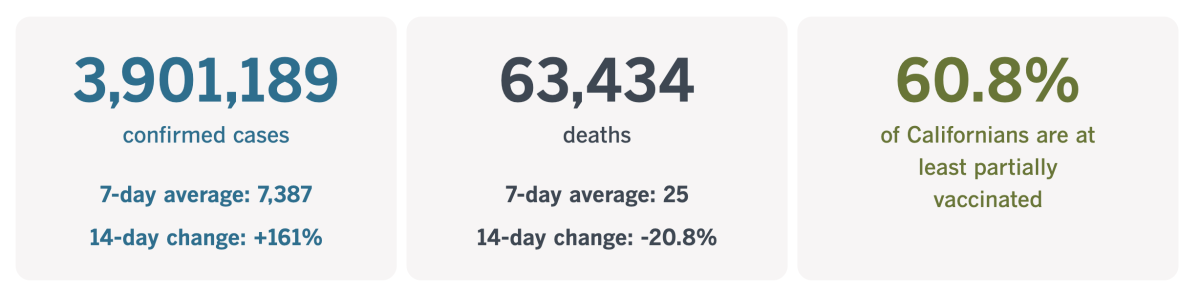
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
What FDA approval means for vaccine hesitancy
If the COVID-19 vaccines are so great, why hasn’t the U.S. Food and Drug Administration formally approved them yet?
It’s a question that’s coming up more and more as people notice that while President Biden and his top health officials are urging people to get vaccinated, the FDA’s official fact sheets warn patients that the shots are still considered experimental.
“The Pfizer-BioNTech COVID-19 Vaccine is an unapproved vaccine that may prevent COVID-19,” one of the warnings states. “There is no FDA-approved vaccine to prevent COVID-19.”
This caution isn’t limited to the Pfizer-BioNTech product. There are identical warnings for the Moderna and Johnson & Johnson shots too.
Dr. Jerome Adams, the former U.S. surgeon general, raised the issue on Twitter a few weeks ago. Adams, a vocal advocate for the vaccines, argues that many people who remain on the fence about the vaccines would embrace them if they received the FDA’s official stamp of approval. Formal approval would also give employers, colleges and other institutions clear legal authority to institute vaccine mandates, he argues.
There’s little doubt that the vaccines currently authorized for emergency use will wind up getting formal approval eventually. More than 342 million doses have been administered in the United States, and tons of real-world data show that they’re safe and effective, even against the highly transmissible Delta variant.
Those may seem like arguments to pull the trigger on formal approval. But they work even better as reasons to go ahead and get vaccinated now while the FDA continues to evaluate the vaccines according to its usual rules.
“The FDA has established a procedure for fully authorizing drugs that has served it well in the past,” my colleague Michael Hiltzik argues in a recent column. “Tinkering with that procedure can only lead to a bad outcome.”

Just think back to last fall, when there were worries that the Trump administration would pressure the FDA to green-light a COVID-19 vaccine before its vetting process was complete. In an effort to bolster public confidence, the heads of nine pharmaceutical companies jointly pledged not to cut any corners on their end.
Political meddling was a bad idea then, and it’s a bad idea now. If consumers — especially vaccine holdouts — suspect the FDA approved the vaccines for reasons based on anything other than science, any effort to rush the approval process will backfire.
In addition, courts have been upholding the legitimacy of COVID-19 vaccine mandates even though the shots are merely authorized for emergency use. A federal judge in Houston rejected a challenge from employees of Houston Methodist Medical Center who said the hospital’s vaccine mandate was reminiscent of the Holocaust. And a federal judge in South Bend, Ind., upheld the University of Indiana’s requirement that students and employees get vaccinated if they want to study or work on campus.
What’s more, Hiltzik makes a strong case that the remaining vaccine holdouts won’t be swayed by a switch from emergency use authorization to approval. Polls consistently find that some people simply don’t believe COVID-19 is a true threat or are skeptical of vaccines in general. For this crowd, nothing the FDA does will make a difference.
Other unvaccinated adults said they’re waiting to see how their friends or family members fare after getting their shots. And some people apparently weren’t aware that the vaccines are available for free. For groups like these, the lack of FDA approval is not the thing that’s holding them back.
“The best thing the agency can do to ensure that the public sees that the vaccines are safe and effective is to put them through the same approval process that has made the U.S. drug market one of the safest in the world,” Hiltzik writes. “Little can be gained by changing the rules, and far too much can be lost.”
Ready to join the 163 million Americans who are fully vaccinated? You can find the shot you need at Vaccines.gov.
California’s vaccination progress
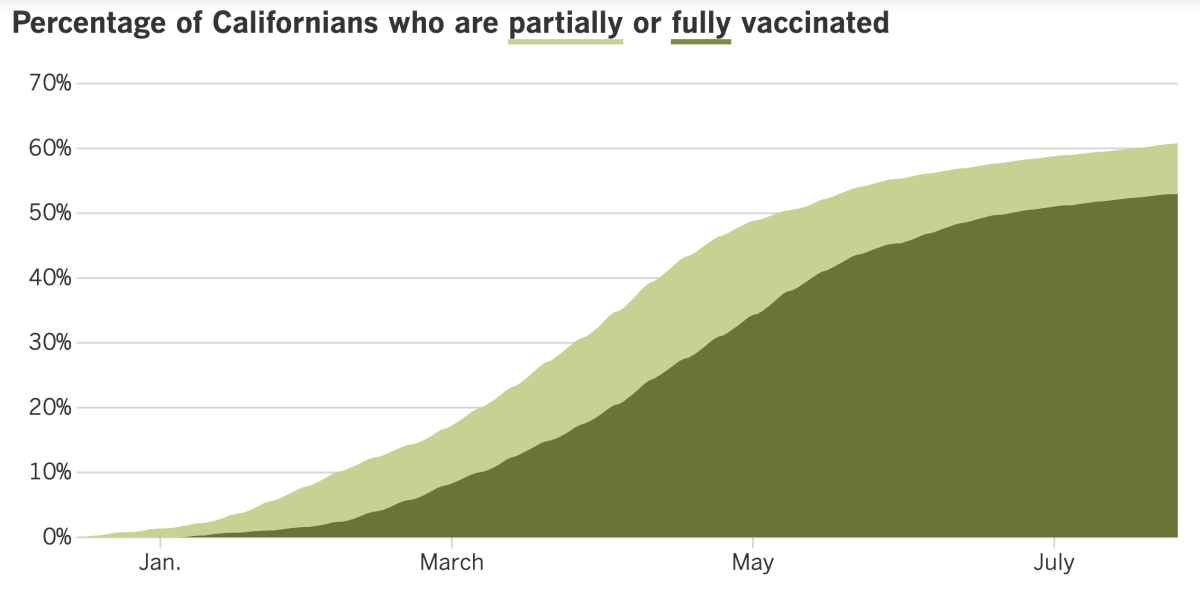
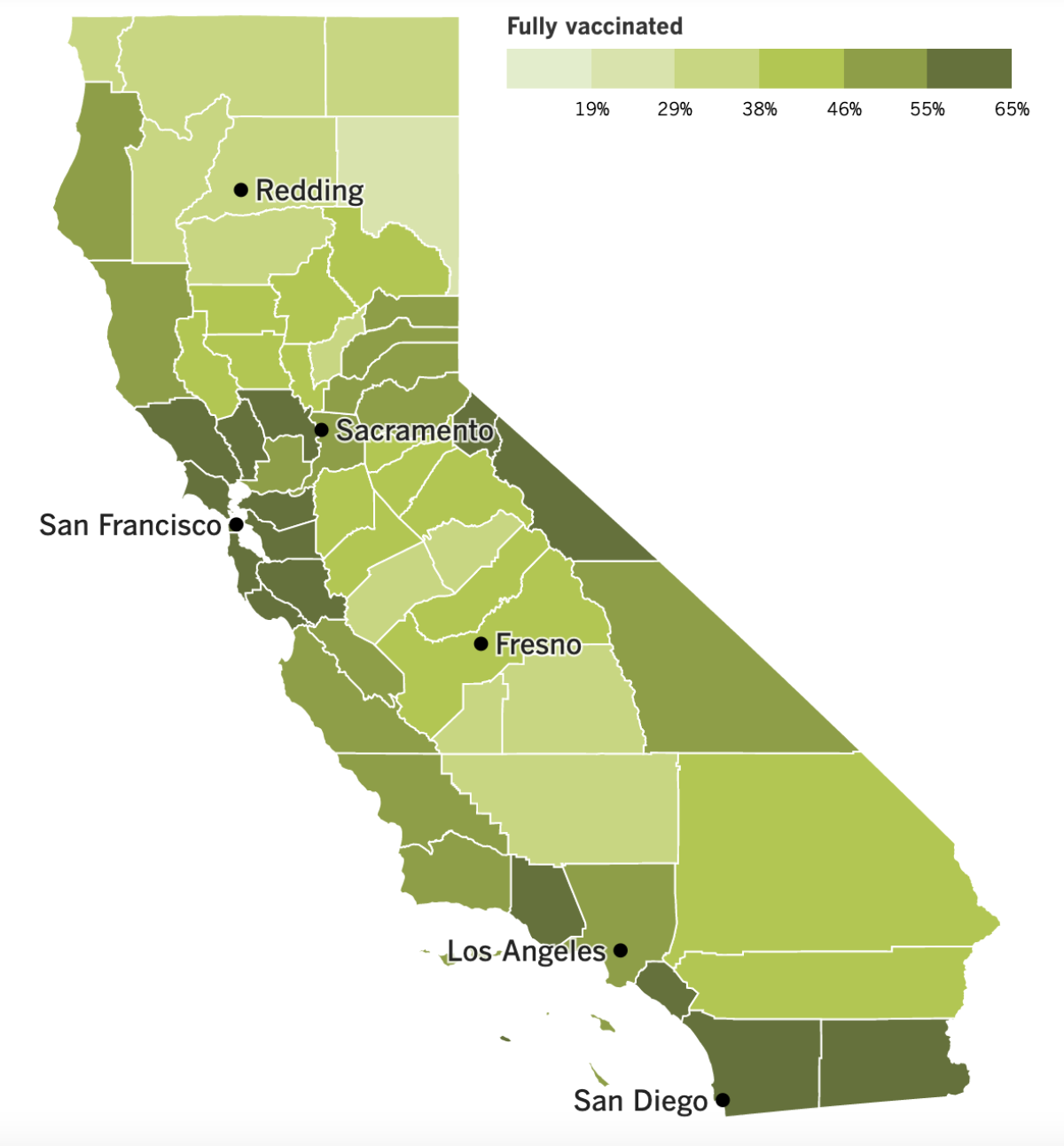
See the latest on California’s vaccination progress with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
In other news ...
California is ramping up the pressure on state workers to get vaccinated against COVID-19, announcing Monday that they’ll soon be required to show proof of their inoculation. Those who decline to get vaccinated, or who won’t offer documentation of their shots, will have to submit to coronavirus testing at least once a week.
The new policy is not a vaccine mandate, but it is an important change because it means the state will no longer let its 246,000 employees vouch for themselves about their vaccination status. The rule goes into effect Aug. 2.
Workers in California healthcare facilities — both public and and private — will be subject to similar requirements starting Aug. 9. The new policy will also apply to people with jobs in jails, homeless shelters, senior living homes and other congregate settings.
Unvaccinated employees in high-risk settings, including acute care facilities and nursing homes, will be tested for coronavirus infections at least twice a week.
“Too many people have chosen to live with this virus,” Newsom said. “We’re at a point in this epidemic, this pandemic, where choice — individuals’ choice not to get vaccinated — is now impacting the rest of us in a profound and devastating and deadly way.”
With that in mind, the state is encouraging all employers to follow its lead. The California State University system is going a step further.
On Tuesday, officials with the nation’s largest four-year public university system said it would require students, faculty and staff to be vaccinated before returning to any of the 23 campuses for the fall semester. The University of California announced a vaccine mandate for its campuses about two weeks ago.
In both cases, people can seek an exemption for medical or religious reasons. Those who receive them will have to be tested frequently to keep coronavirus outbreaks from flaring up.
Joseph I. Castro, the chancellor of the Cal State system, had previously said that he wouldn’t implement a vaccine requirement until the shots had received full FDA approval. With the Delta variant spreading rapidly and the FDA not saying when formal approval will come, Cal State opted to move ahead now.
The decision was unanimous among the presidents of all 23 universities, Castro said. Students generally embraced the plan as well, said Isaac Alferos, president of the Cal State Student Assn.
Some Los Angeles politicians would like to see a similar mandate for city workers. Councilman Mark Ridley-Thomas said he would introduce a motion Wednesday that would direct city staffers to come up with a policy to make that happen.
The pandemic “is not retreating,” Ridley-Thomas said, “and the best defense to date are the vaccinations. So why wouldn’t we do all that we can to avoid the calamity that we were confronted with no more than five months ago?”
L.A. County Supervisor Kathryn Barger is behind the idea as well, saying Tuesday that “we need to begin the process of preparing to require all county employees to be vaccinated.... We are preaching, and I think we need to practice in terms of moving forward with our county workforce.”
Vaccine mandates have already been announced in San Francisco, Pasadena and New York. And on Monday, the Department of Veterans Affairs joined that list.
The VA became the first major federal agency to require vaccination of healthcare workers. The mandate will apply to physicians, dentists, podiatrists, optometrists, registered nurses, physician assistants and others who work in departmental facilities or provide direct care to veterans.
Nearly all doctors are vaccinated, but uptake hasn’t been as vigorous among other categories of health workers. For instance, only about 60% of nursing home staffers are vaccinated, according to data from Medicare. The VA’s announcement came as the American Medical Assn., the American Academy of Nursing, the American Public Health Assn. nearly 60 other organizations called on health facilities to require COVID-19 vaccines for their workers.
“We stand with the growing number of experts and institutions that support the requirement for universal vaccination of health workers,” the medical and healthcare organizations said in a statement.
And finally, a new study estimates that more than half the country’s coronavirus cases were not counted in the official tally up through early March of this year.
Experts acknowledge that infections, illnesses and deaths are undercounted, for a variety of reasons. Sometimes it’s due to problems like inadequate testing or poor record-keeping. Other times, political leaders want to suppress the truth about the extent of the pandemic’s toll.
The study used data from two random testing surveys conducted in Indiana and Ohio to calibrate their estimates of the undercount. Their conclusion: Only 1 out of every 2.3 infections in the U.S. had been confirmed via testing. Based on that, they determined that nearly 20% of the population — roughly 65 million people — had been infected by early March.
“This suggests that the United States was far from reaching herd immunity and that it was unlikely to do so from infections alone,” the study authors wrote in the Proceedings of the National Academy of Sciences.
That’s a sobering message, said Jennifer Nuzzo, an epidemiologist at the Johns Hopkins Center for Health Security. who was not involved in the study: “We still have a long way to go, and a whole lot more people could get sick and die before it’s done.”
Your questions answered
Today’s question comes from readers who want to know: Do I need to get vaccinated if I’ve already had COVID-19?
If you’ve had COVID-19 and recovered, your immune system made antibodies that will offer you protection against a future coronavirus infection. But experts agree that you should get vaccinated anyway.
For one thing, the vaccines induce a stronger immune response than a natural infection, especially if your COVID-19 symptoms were mild, said Mercedes Carnethon, an epidemiologist at Northwestern University Feinberg School of Medicine.
“We get a more robust and consistent response from the vaccine,” Carnethon told my colleague Amina Khan. That makes it a better bet “for immunity over a long period of time.”
Also, if you had a coronavirus infection much earlier in the pandemic, the antibodies your immune system made might not offer enough protection against the variants that are dominant now. But multiple studies suggest the vaccines offer good protection against Delta and the other variants circulating today, Carnethon said.
Finally, scientists have found that just one dose of vaccine can give a COVID-19 survivor a huge immune system boost.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
Resources
Need a vaccine? Sign up for email updates, and make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Need more vaccine help? Talk to your healthcare provider. Call the state’s COVID-19 hotline at (833) 422-4255. And consult our county-by-county guides to getting vaccinated.
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




