Coronavirus Today: Freedom from the Delta variant
Good evening. I’m Karen Kaplan, and it’s Friday, July 2. Here’s what’s happening with the coronavirus in California and beyond.
This Fourth of July weekend we’ll be celebrating our freedom — from England 245 years ago and from the state’s COVID-19 restrictions that were lifted just last month. Californians can gather guilt-free with members of other households, enjoy the air conditioning inside their favorite restaurants, and fill the stands at Angel Stadium.
But in Los Angeles County, the atmosphere will be a little less festive.
Health officials know the coronavirus won’t be taking a holiday. And with the highly transmissible Delta variant on the loose, they’re not taking any chances.
They’ve already asked Angelenos to go back to wearing face masks indoors even if they’re fully vaccinated against COVID-19. That puts California’s most populous county at odds with state health officials as well as with experts at the U.S. Centers for Disease Control and Prevention.
L.A. County Public Health Director Barbara Ferrer and her colleagues aren’t just messing with us to stay in the spotlight. There are reasons to step up our vigilance, including:
• New coronavirus cases are rising. A total of 422 new cases were reported in L.A. County on Wednesday, June 30. That’s more than double the 210 new cases on June 15, the day California’s economy reopened.
• Over the seven-day period that ended Wednesday, the county averaged about 298 new cases per day. That’s an 85% increase over the seven-day period that ended June 24.
• County hospitals were treating 280 patients for COVID-19 on Wednesday. That’s up 31% since June 19, when 213 people were hospitalized with the disease.
• The proportion of coronavirus tests that turn out to be positive was 1.2% on Wednesday. The test positivity rate was less than half that on June 15 — just 0.5%.
To be sure, all of these numbers are far below their January peaks. But if it’s all the same with you, I’d rather not pretend the worst days of that devastating surge are an acceptable baseline.
At the risk of sounding like a broken record, the easiest way to protect ourselves against the Delta variant — along with all other coronavirus strains — is to get vaccinated.
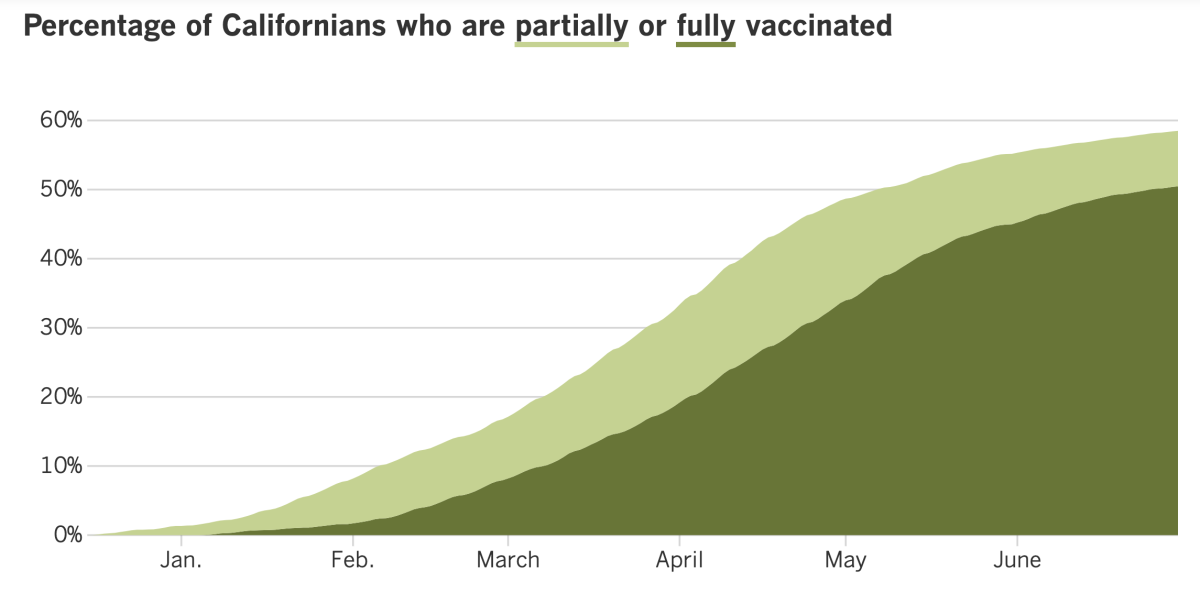
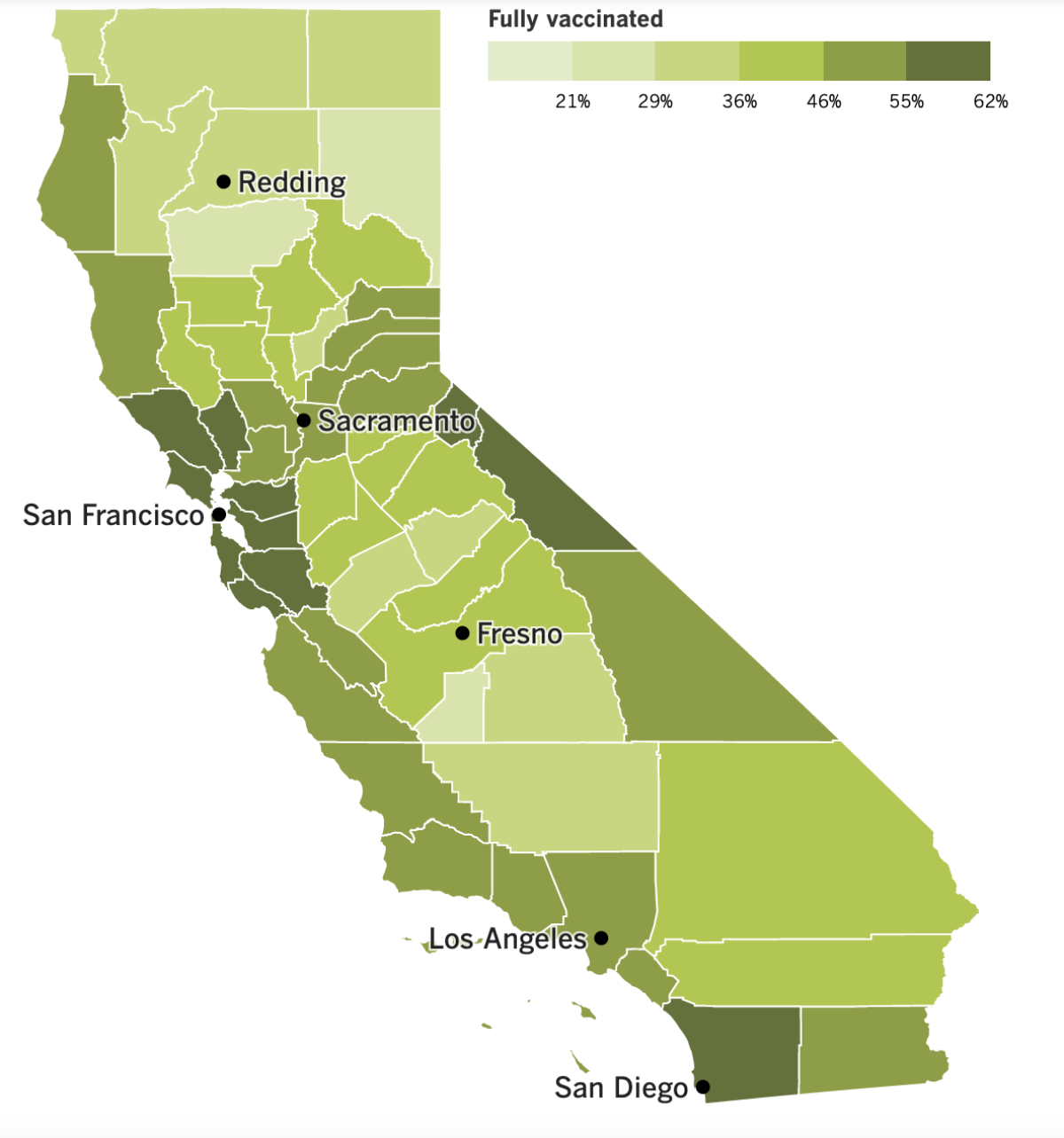
Only 50.7% of Los Angeles County residents are fully vaccinated (as are 50.5% of all Californians). That leaves plenty of of folks who are still vulnerable.
“Given that we have large numbers of unvaccinated people in Los Angeles County — 4 million in total, including 1.3 million children not yet eligible to be vaccinated — another wave could become a very real possibility,” Ferrer said.
By the numbers
California cases, deaths and vaccinations as of 3:35 p.m. Friday:
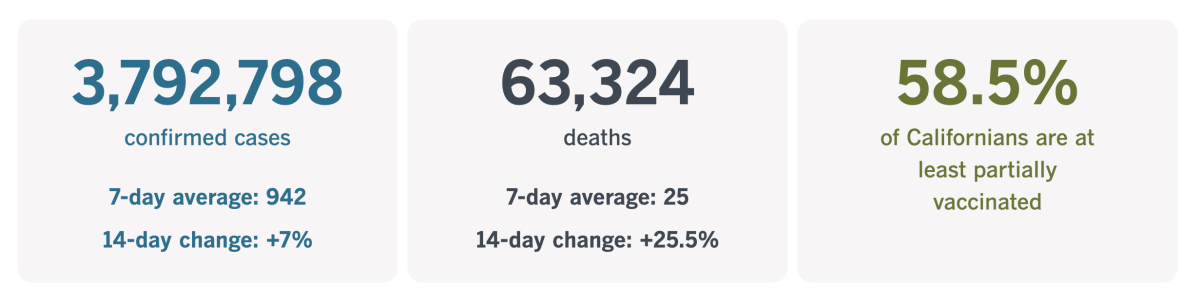
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Actual safety vs. hygiene theater
Take a look at the expression on this girl’s face:

This is 8-year-old Zadie Williams, and she’s getting her temperature taken upon arrival at her summer school class at Hooper Avenue School in Los Angeles.
Temperature checks have become de rigueur during the pandemic — at schools, at the gym, at the Los Angeles County Museum of Art. But we’ve known for a while that this is an unreliable way to identify people with active coronavirus infections.
Way back in October, a detailed survey of nearly 4,000 COVID-19 survivors found that only 7.7% of them had a fever in the first 10 days of their illness. Considering that roughly 40% of people with coronavirus infections are completely asymptomatic, that means fewer than 5% of infected people could be identified by a temperature check — and more than 95% of them could not.
Another study focused solely on kids who caught the coronavirus found that at least 81% of them never came down with a fever as a result of their infections.
Zadie may not be up on all the science, but that “I’m so over this” look in her eyes is exactly what you’d expect from someone who thinks the thermometer is being deployed more for show than for actual safety.
Displays like this have come to be known as “hygiene theater.” Derek Thompson, a staff writer at the Atlantic, noticed it last summer. He wondered why so many businesses were bragging about all the surfaces they were sanitizing when scientists had determined that the coronavirus spread mainly through the air. It was reminiscent of the over-the-top security measures instituted at airports after 9/11.
“COVID-19 has reawakened America’s spirit of misdirected anxiety, inspiring businesses and families to obsess over risk-reduction rituals that make us feel safer but don’t actually do much to reduce risk — even as more dangerous activities are still allowed,” Thompson wrote.
Dr. Panagis Galiatsatos, a pulmonary and critical care specialist at the Johns Hopkins School of Medicine, has the same reaction about the temperature screenings at his daughter’s summer camp.
“The temperature check is by far the bane of my existence,” Galiatsatos told my colleague Amina Khan. “Temperature checks establish body temperature, not if you have a fever.”
And as we’ve established, even that is hardly the same as establishing whether someone is infected with the coronavirus.
“The whole concern about COVID has been its asymptomatic spread,” Galiatsatos said. “Using temperature checks to prevent that is like trying to catch a golf ball using a volleyball net. You’re giving people a false sense of security.”
The problem is that when we feel any kind of security in the midst of this pandemic, the last thing we want to do is give it up.
“Unwinding these protocols is turning out to be a little more emotional than the science,” Dr. Lindsey Leininger, a public health scientist at Dartmouth, said on the Donlon Report.
She gets it. She even says we should cut ourselves some slack if we do take comfort in these rituals. But that doesn’t mean we can afford to keep pointing thermometers at people while ignoring the real threats.
“Sometimes it distracts from what truly matters,” she said. “Get vaccinated, wear a mask and clean the indoor air. I cannot stress ‘clean the indoor air’ enough.”
California’s vaccination progress
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
In other news ...
The Delta variant has now been identified in at least 96 countries, according to the World Health Organization. That figure stands as a harsh reminder of the unrelenting nature of a virus: To stay alive, it adapts and mutates.
Governments around the world are scrambling to contain it — even Israel, the country with the highest COVID-19 vaccination rate on the planet.
Some 85% of Israeli adults have gotten their COVID-19 shots, prompting the country to reopen its businesses, schools and other venues. But on Thursday, the number of new coronavirus infections hit 307, the highest daily level in nearly three months. And the country’s health ministry expects it to keep on rising.
Now health officials are racing to vaccinate children; they administered more shots to kids this week than in any previous week. The country also revived a requirement that face masks be worn indoors. Other measures under consideration are tighter travel restrictions at Israel’s main airport and a resumption of its “Green Pass” system, which gives vaccinated residents access to certain venues and activities while keeping those who are unvaccinated out.
India has confirmed 400,000 deaths from COVID-19, with half of them occurring in just the last two months as the Delta variant overwhelmed the already-strained health system. Officials believe the true toll in India is much higher, and that COVID-19 deaths there might have topped 1 million.
In Russia, a surge in new infections prompted health authorities to roll out COVID-19 booster shots for people who were immunized more than six months ago.
“I’m pleading with you not to miss a chance to get additional protection from the virus, which is particularly important amid the spread of a more aggressive delta variant,” Moscow Mayor Sergei Sobyanin wrote on his blog.
Russian health authorities said the Delta variant was responsible for the bulk of recent new infections in Moscow and some other regions. The government’s coronavirus task force has reported more than 20,000 new infections each day since last Thursday — more than double the average in early June. There were 23,543 new cases on Thursday and 672 deaths, the highest daily death toll since the pandemic began.
Governments in Africa would love to deploy vaccines against the Delta variant, but that’s not an option for them.
Strive Masiyiwa, the African Union’s special envoy tasked with procuring COVID-19 vaccines for the continent, blamed the United Nations-backed initiative called COVAX for failing to deliver shots to low- and middle-income countries and for keeping mum about key donors who hadn’t followed through with their funding pledges.
“The situation could be very different had we known back in December that ‘Listen, this help is not coming, do for yourselves,’” Masiyiwa said.
He saved the worst of his ire for Europe, lamenting that “not one dose, not one vial, has left a European factory for Africa” despite a crushing surge of infections there.
The WHO stepped into some controversial vaccine waters this week, saying that if a COVID-19 vaccine was good enough to pass muster with them, it ought to be good enough for any country that’s opening its borders to inoculated travelers.
The comments were aimed in part at the European Union, which has said it would consider would-be visitors vaccinated only if the shots they got were licensed by the European Medicines Agency. That list does not include two Chinese vaccines made by Sinovac and Sinopharm, both of which got a green light from the WHO.
The EU drug regulator is considering licensing China’s Sinovac vaccine, but there is no timeline on a decision. It also does not recognize versions of the AstraZeneca vaccine that were made in India, effectively barring travel for people in developing countries who received doses via the U.N.-backed initiative known as COVAX.
“Any measure that only allows people protected by a subset of WHO-approved vaccines to benefit from the reopening of travel ... would effectively create a two-tier system,” the WHO said Thursday. “It would negatively impact the growth of economies that are already suffering the most.”
WHO officials are drawing up plans for the next phase of its probe into the origins of the COVID-19 pandemic, but a growing number number of scientists say the agency shouldn’t be the one to investigate.
Even some experts with strong ties to WHO say that political tensions between the U.S. and China make it impossible for an investigation by the agency to find credible answers. Instead, they’re calling for a broad, independent analysis like the one in the wake of the 1986 Chernobyl nuclear disaster.
The global health agency can’t compel China to cooperate with an investigation, and that’s a dealbreaker in some people’s eyes.
“We will never find the origins relying on the World Health Organization,” said Lawrence Gostin, director of the WHO Collaborating Center on Public Health Law and Human Rights at Georgetown University. “For a year and a half, they have been stonewalled by China, and it’s very clear they won’t get to the bottom of it.”
Your questions answered
Today’s question comes from readers who want to know: For children, how does the risk of a serious side effect from the COVID-19 vaccine compare with the health risks of getting COVID-19?
This question has been on parents’ minds since the U.S. Food and Drug Administration authorized the Pfizer-BioNTech vaccine for use in kids as young as 12 — and it became more pressing in light of reports that some teens developed a heart condition called myocarditis in the days after they got their shots.
Experts with the CDC’s Advisory Committee on Immunization Practices did the math and determined that for boys between the ages of 12 and 17, administering 1 million second doses of the vaccine would result in 56 to 69 cases of myocarditis — an inflammation of the heart muscle — over 120 days. But those shots would also prevent 5,700 cases of COVID-19, including 215 hospitalizations, 71 admissions to the ICU and two deaths.
For girls ages 12 to 17, 1 million second doses would be followed by eight to 10 cases of myocarditis over 120 days, while preventing 8,500 cases of COVID-19, including 183 hospitalizations, 38 ICU admissions and one death.
In other words, the risk that boys and girls will become seriously ill with COVID-19 if they don’t get vaccinated is greater than the risk that they’ll get myocarditis if they do get vaccinated.
If you need a little more perspective, consider that American children are routinely vaccinated for other diseases that are far less deadly than COVID-19. Researchers broke it down in the Journal Clinical Infectious Diseases:
Varicella (aka chicken pox) caused 50 pediatric deaths per year between 1970 and 1994, the year before the varicella vaccine was introduced in the U.S.
Rotavirus killed between 20 and 60 kids per year between 1999 and 2007; a vaccine to prevent the gastrointestinal disease was rolled out in the U.S. in 2006.
Rubella (a.k.a. German measles) resulted in 17 childhood deaths per year between 1966 and 1968, the before the U.S. got its first rubella vaccine. (It’s now combined with vaccines for measles and mumps.)
For the sake of comparison, COVID-19 has claimed the lives of at least 322 children as of May 27, 2021.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

This cutie is Ava Marie, the 8-year-old brand ambassador for the children’s clothing company Brooklynn & Blake.
Michelle Youngblood, the woman seen fitting the dress, launched Brooklyn & Blake in October. A pandemic might not seem like the most opportune time to start a new business, but Youngblood and thousands of other Black entrepreneurs are challenging that notion by turning adversity into opportunity.
My colleague Don Lee reports that 380 out of every 100,000 Black adults became new entrepreneurs during the 2020 pandemic — the highest that figure has been in the last 25 years. In fact, Black entrepreneurism last year ranked higher than for white-owned and Asian-owned companies.
Youngblood took the leap after she was laid off from her job at a health insurance company last summer and received enough severance pay to fulfill a lifelong dream. Don’t miss this inspiring story about one of the pandemic’s rare silver linings.
Resources
Need a vaccine? Sign up for email updates, and make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Need more vaccine help? Talk to your healthcare provider. Call the state’s COVID-19 hotline at (833) 422-4255. And consult our county-by-county guides to getting vaccinated.
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




