Coronavirus Today: With the Delta variant’s rise, masks are back
Good evening. I’m Karen Kaplan, and it’s Tuesday, June 29. Here’s what’s happening with the coronavirus in California and beyond.
Last week we told you that if anything looked likely to roll back our newfound pandemic freedoms, it was the Delta variant. Sure enough, it is.
On Monday, the Los Angeles County Department of Public Health advised all residents to wear masks while they’re in public indoor spaces — even if they’re fully vaccinated against COVID-19.
It may seem like a mixed message. After all, the county reminded people that “fully vaccinated people appear to be well protected from infections with Delta variants.” And as far as scientists can tell, that appears to be true.
But no vaccine is perfect. The county has confirmed at least 10 coronavirus infections involving the Delta variant among people who were fully vaccinated. None required hospital care, most likely thanks to the immune-system boost they got from the vaccine.
The Delta variant, which was first identified in India, has also been found in three county residents who were partially vaccinated and 110 who were unvaccinated. These are the people health officials are most worried about.
Scientists estimate that Delta is 60% more transmissible than the Alpha variant from the United Kingdom, which in turn is 50% more transmissible than the original coronavirus strain. That means Delta spreads more than twice as readily as the version of the virus that sparked the global pandemic.
Among coronavirus samples sequenced in the U.S. in the two-week period that ended June 5 (the most recent reporting period available), 10% were Delta, according to the Centers for Disease Control and Prevention. In the prior two weeks, this variant accounted for just 2.9% of samples sequenced.
In addition, by June 5, Delta made up nearly 35% of samples analyzed in Iowa, Kansas, Missouri and Nebraska, and 25% of those in Colorado, Utah, Montana, Wyoming and the Dakotas.
In California, Delta accounts for 14.5% of coronavirus samples that have been sequenced so far in June, making it the third-most common variant in the state. With that in mind, asking everyone to wear masks in supermarkets, movie theaters, offices, retail stores and other indoor venues sounds like a way to be safe instead of sorry.

“Until we better understand how and to who the Delta variant is spreading, everyone should focus on maximum protection with minimum interruption to routine as all businesses operate without other restrictions, like physical distancing and capacity limits,” L.A. County officials explained in a statement.
L.A.’s advice aligns with that of the World Health Organization, which advises people to “wear a mask, especially in crowded, closed and poorly ventilated settings,” even after they’ve been vaccinated. The CDC, on the other hand, still says people who’ve been fully vaccinated don’t need to wear masks or worry about social distancing.
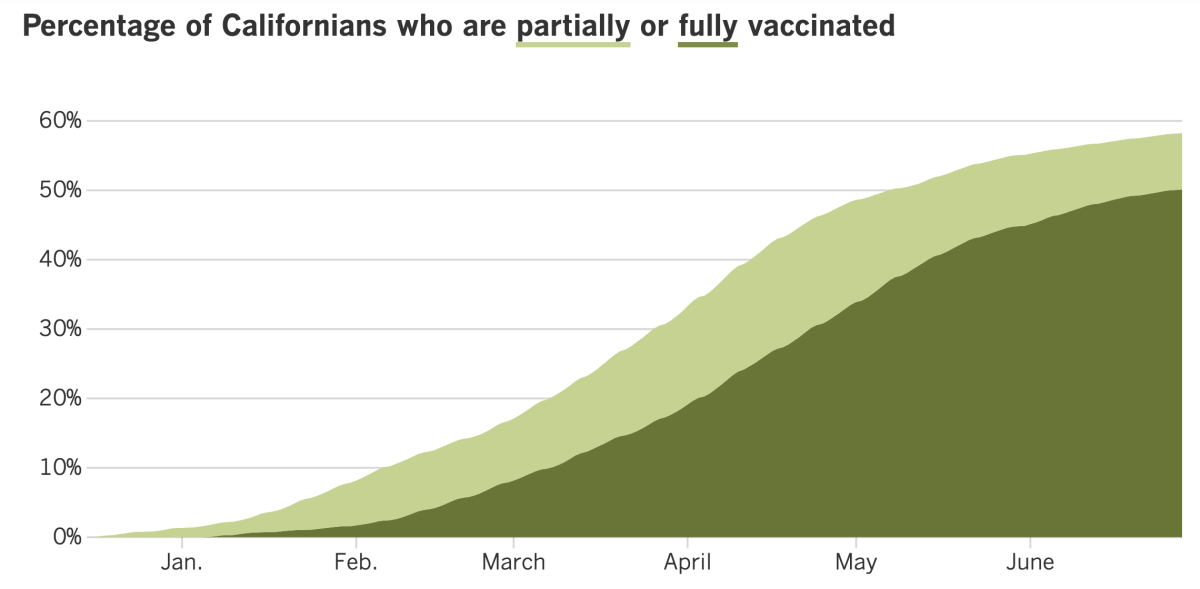
It’s unclear if Delta will prompt officials here to reinstate other safety measures for those who are vaccinated. Even if coronavirus spread accelerates, California’s vaccine coverage is high enough to prevent another devastating surge.
(Contrast that with South Africa, where less than 1% of the population is vaccinated. The Delta variant is fueling a third wave of infections there that’s on track to top the previous two, prompting President Cyril Ramaphosa to impose a sweeping set of new restrictions that includes a ban on indoor and outdoor gatherings, earlier curfews for nonessential businesses and the suspension of leisure travel in and out of the country’s most populous province.)
But the more a virus spreads, the more chances it has to mutate. And the more it mutates, the more chances it gets to acquire a genetic change that reduces the efficacy of vaccines or medicines.
“It’s quite simple: More transmission, more variants. Less transmission, less variants,” WHO Director-General Tedros Adhanom Ghebreyesus said Friday. “That makes it even more urgent that we use all the tools at our disposal to prevent transmission.”
Including masks.
By the numbers
California cases, deaths and vaccinations as of 4:24 p.m. Tuesday:
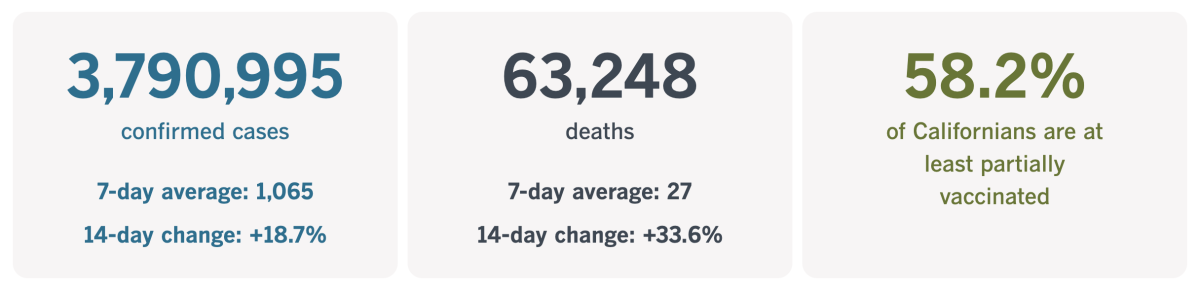
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
The limits of vaccine lotteries
Public officials desperate to boost COVID-19 immunization rates surely thought they’d hit the jackpot when they rolled out vaccine lotteries. After all, few things motivate Americans more than cold, hard cash.
Ohio Gov. Mike DeWine was the first to dangle federal pandemic relief funds in front of vaccine-hesitant citizens, hoping the prospect of a $1-million payout would persuade them to roll up their sleeves.
“I know that some may say, ‘DeWine, you’re crazy! This million-dollar drawing idea of yours is a waste of money,’” the governor said. But in his view, the bigger waste would be “a life lost to COVID-19” — especially when the vaccines to prevent the disease are readily available.
The idea appealed to other governors, who copied the idea in their states. California’s version, Vax for the Win, offered 10 grand prizes of $1.5 million each and a variety of other rewards. Everyone who received at least one dose of COVID-19 vaccine is eligible to win.
But six weeks after DeWine unveiled his Vax-a-Million program in mid-May, it’s becoming clear that it’ll take more than cash — even huge amounts of it — to entice the remaining holdouts to get shots.
Just look at Ohio. By the time its program wrapped last week, only 47% of residents had received at least one dose of COVID-19 vaccine. In other words, more than half of Ohioans have no vaccine protection.
The story is the same in other states.
West Virginia Gov. Jim Justice hoped a lottery would induce at least two-thirds of eligible residents — those age 12 and up — to get the shots by the time the state’s mask mandate was lifted June 20. When the big day came, only 61.5% of eligible residents had been at least partially vaccinated.
Colorado Gov. Jared Polis announced weekly drawings of $1 million. Yet 589,000 fewer doses of COVID-19 vaccine were administered in the month after Colorado Comeback Cash was unveiled than in the month before.
The results in California have been mixed, according to a Los Angeles Times data analysis. In the early weeks of Vax for the Win, the average number of vaccine doses administered throughout the state each day increased 33%, from 121,000 to about 161,000.

Nationwide, the average daily number of vaccinations increased by just 14% during the same period, and only five states — Montana, Utah, Georgia, South Carolina and New Hampshire — saw larger percentage increases in those same weeks.
The most recent seven-day period my colleagues analyzed averaged 132,000 vaccine doses per day. That’s a decline from the peak and well below the 400,000 daily doses the state was averaging in early April. But it’s still higher than in the pre-lottery days.
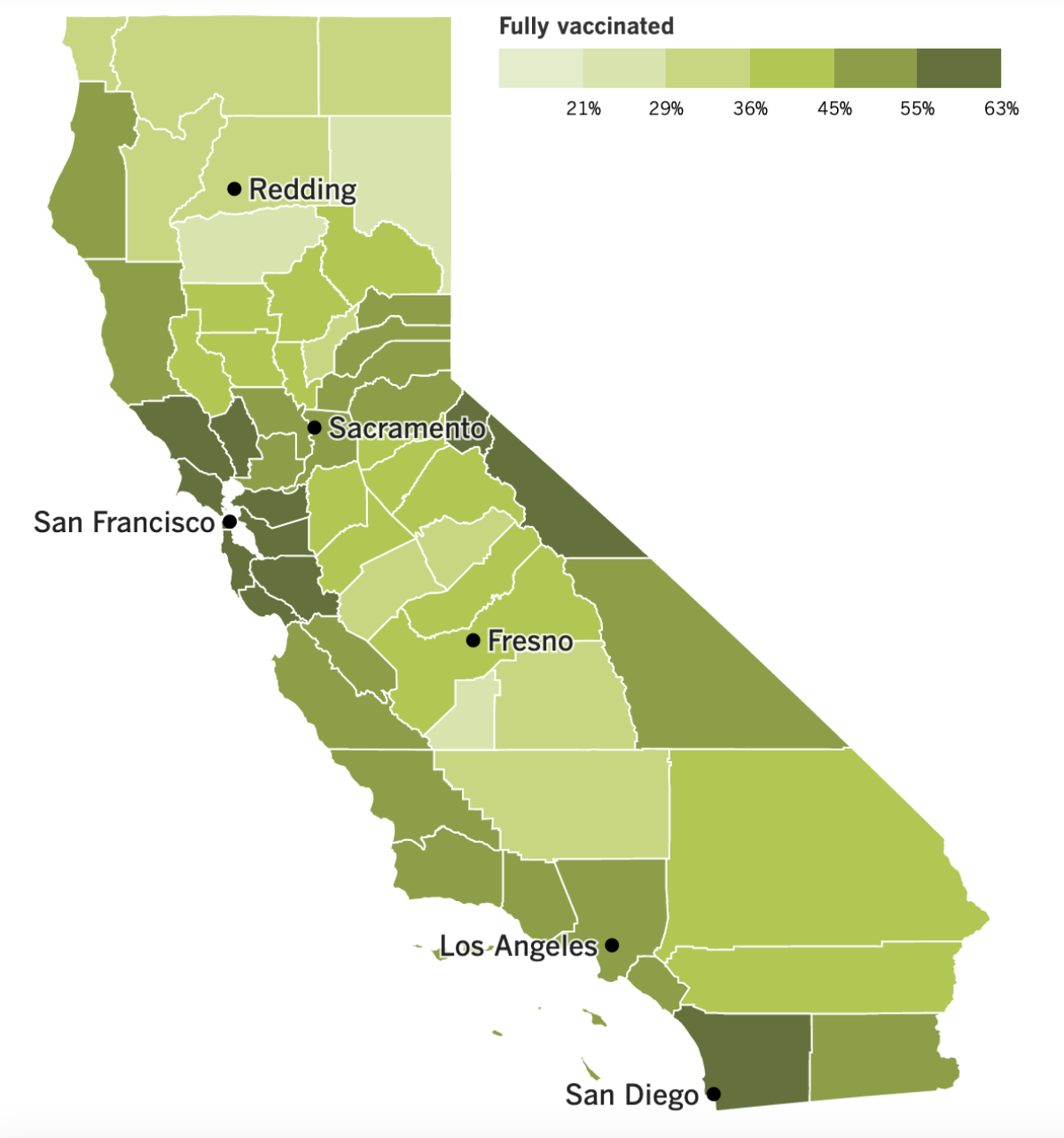
Immunizations have stalled out in some of California’s Black and Latino neighborhoods that were hit hardest by the coronavirus, as well as in rural communities that were hostile to vaccines even before the pandemic. Health officials still think they can make inroads, but other experts say it will be a struggle thanks to the state’s inconsistent messaging and an outreach campaign that asks private companies to do much of the heavy lifting.
A better approach, these critics say, is to have local public health departments work with community clinics, nonprofits and other trusted organizations to dispel anti-vax myths and talk through people’s hesitancy about vaccines. This kind of outreach is time-consuming and expensive — but if we want to get to herd immunity, it’s unavoidable.
Just ask Carnella Marks, a Black resident of Oroville whose personal experience with doctors, combined with the country’s racist history, have left her skeptical about official assurances that the new vaccines are safe. She had thought seriously about getting the single-dose Johnson & Johnson vaccine, but then the government suspended its use over concerns about rare blood clots.
A vaccine lottery isn’t going to persuade her to put her trust in a system that hasn’t earned it.
“I don’t care what kind of money the governor is shelling out to get me to take the vaccine,” Marks told Kaiser Health News. She wants to know more about the safety of the vaccines, but “nobody’s knocking on my door to talk to me or answer my questions.”
California’s vaccination progress
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
In other news ...
Fellow Californians, have you received your digital COVID-19 vaccination record? If you have, you might have noticed an apparent glitch: The QR code you got from the state doesn’t seem to retrieve any information.
But don’t fret. That’s a feature, not a bug, according to the California Department of Public Health.
That pixel-y square may look like a regular QR code, but it’s actually a Smart Health Card, my colleague Luke Money reports. To provide extra security, it can be properly scanned only by a compatible device or app. This way, there’s no risk that your name, date of birth or vaccination status can be found out by anyone who happens to have a QR code reader (that is, anyone with a smartphone).
Speaking of vaccines, San Francisco has become the first major city and county in California to implement a COVID-19 vaccine mandate for its employees.
Exemptions are available for those who need to skip the shots for medical or religious reasons, but other employees could lose their jobs if they refuse to get the shots once they receive formal approval from the Food and Drug Administration. (So far, the COVID-19 vaccines have been rolled out under an emergency use authorization.)
The vaccine mandate extends to all 35,000 city government employees, including police, firefighters, custodians and City Hall clerks. Front-line workers in hospitals, nursing homes and jails were already required to get vaccinated.
At this point, Los Angeles County isn’t planning to follow in San Francisco’s footsteps, Public Health Director Barbara Ferrer said.
Good news for California renters: Newsom signed a bill Monday that extends eviction protections for tenants who pay at least 25% of their rent. Low-income tenants can have all of their past-due rent paid up by the state as part of a $5.2-billion rent relief program that helps not only renters but also their landlords.
Newsom called it “the largest and most comprehensive COVID rental protection and rent relief program of any state in the nation.”
Under the deal made with the Legislature, tenants and landlords can apply right away for the new funds. Payments can cover past-due rent going back to April 2020 and through Sept. 30, when the new eviction protections expire.
Some 758,000 California households are behind on their rent, and the average amount owed is $4,700, according to research by PolicyLink and the USC Equity Research Institute.
National vaccine effort: The Biden administration is throwing new support into its campaign to get 70% of U.S. adults vaccinated by the Fourth of July. Officials are going after the “movable middle,” some 55 unvaccinated million adults — many of them under 30 — who are seen as persuadable.
The administration is sending A-list officials across the country to devise ads for niche markets and enlist the help of community organizers. It’s almost like a hard-fought political campaign, complete with data crunching to identify groups that can be won over.
“It’s door to door. It’s mobile clinics. We’re doing vaccinations at church, the PTA meeting, the barber shop, the grocery store,” said Health and Human Services Secretary Xavier Becerra.
You may be thinking that getting some Americans to roll up their sleeves is like pulling teeth. But my colleague Andrew Mendez reports that Americans are now clamoring for dental appointments after going more than a year without having their teeth cleaned.
In April 2020, patient volume at private dental practices plummeted to 7% of the pre-pandemic baseline, the American Dental Assn. says. As of this month, volume is up to 88%.
Dental hygienist Jeannette Diaz can attest to that. She sees about six patients each weekend and has to turn down an additional four. Appointments that used to last about an hour now take twice as long. It’s not just that she’s scraping off more than a year’s worth of tartar and plaque; it’s that patients are eager to talk about the pandemic and how it affected their lives.
“It can be emotionally exhausting and draining when you hear about what they are experiencing mentally and emotionally that leads them to … be unable to care for their oral hygiene,” Diaz said.
Finally, I’d like to thank the reader who pointed out a spelling error in Friday’s newsletter. I mentioned a blogger in China who was sentenced to six months in prison for posting stories about the suffering of Wuhan residents while the city was under lockdown. That blogger was in Hebei (not Heibei) province.
Your questions answered
Today’s question comes from readers who want to know: Why is Japan lagging so far behind on COVID-19 vaccinations?
After all, Japan is a wealthy nation with an advanced healthcare system and a thriving pharmaceutical industry. And the Tokyo Olympics, which begin in just 3½ weeks, provide a huge incentive for the country to gets its act together on immunizations.
Yet as of Tuesday, only 10.9% of the Japanese public was fully vaccinated, according to Our World in Data. That’s slightly below the worldwide average of 10.7% and nowhere close to the U.S., where 46.8% of residents are fully vaccinated.
A variety of factors account for the gap, starting with the fact that the country is wary of vaccines in general.
Accounts of side effects — even rare ones — prompt a lot of media attention. For instance, reports of side effects that seemed to be related to the HPV vaccine caused Japan to stop recommending it, even though it is widely used around the world to prevent cervical cancer. (Sure enough, the apparent “side effects” were later found to be unrelated to the HPV vaccine.)
In addition, Japan has no homegrown vaccine. The public’s skepticism toward vaccines makes them a risky investment for pharmaceutical companies. A few candidates are now in clinical trials, but even if they work out, approval is still months away. That means the country has had to rely on imports, which were in short supply until last month.
Plus, Japan is not entirely comfortable with vaccines made elsewhere. To boost confidence, the government requested vaccine makers to conduct additional tests in small numbers of Japanese people, even though large-scale clinical trials had already been conducted.
For instance, the Pfizer-BioNTech vaccine was vetted in about 44,000 volunteers from six countries (including about 2,000 people of Asian descent), but Japan asked for tests on 160 Japanese people. Critics say that delayed the vaccine rollout by several months without generating much useful data.
Once the vaccines were in the clear, the rollout was hampered by uncertainties related to supply and distribution, a confusing system for scheduling appointments and a shortage of medical workers able to administer the shots.
Pfizer and BioNTech have teamed up with the International Olympic Committee to donate doses to athletes who will be competing in Tokyo. Organizers expect 80% of athletes to be vaccinated by the time the Games begin.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
Resources
Need a vaccine? Sign up for email updates, and make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Need more vaccine help? Talk to your healthcare provider. Call the state’s COVID-19 hotline at (833) 422-4255. And consult our county-by-county guides to getting vaccinated.
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




