Coronavirus Today: When grown kids move back in
Good evening. I’m Russ Mitchell, and it’s Wednesday, June 9. Here’s what’s happening with the coronavirus in California and beyond.
For the record:
12:09 p.m. June 10, 2021An earlier version of this newsletter stated that an article by Times intern Madalyn Amato on what to do if you’ve lost your COVID vaccination card was published in April. Amato’s article was published last week.
After more than a year of fear, pain, illness and death, about 600,000 Americans have died of COVID-19. Countless others struggled with social isolation as people masked up, kept physically distant and spent most of their time at home, many of them alone.
But tragedy often draws people closer together. That’s certainly been the case with COVID-19.
The fact that so many adult kids have moved back in with their parents during the pandemic is not news. Last July, 52% of Americans ages 18 to 29 lived with a parent — the highest level recorded in at least a century, according to the Pew Research Center. Many were trying for the first time a kind of intergenerational living far more common in other countries.
The Times’ Soumya Karlamangla got close to some of the families behind those numbers and learned that their experiences turned out to be deeper and more fulfilling than they might have expected.
The Anderson family leads off her story. Melissa, now 29, last summer moved from Los Angeles to rural Gridley, north of Sacramento, to live with her parents. She had never spent much time alone with them, as the third of four daughters. But over several months, the three formed a bond that resembles a friendship among peers more than a parent-child relationship.
Nearly every evening after dinner, Melissa and her mother, Mary, would walk a mile on a road outside their home amid walnut groves. They talked about dating, religion, money, family relationships, life goals — conversations far deeper than they’d had in the past. “I would like to be her friend if she wasn’t my daughter,” said Mary, 58.
Melissa knew she wanted ultimately to move back to Southern California, so she asked her parents to make sure she moved out by this summer, fearing she wouldn’t leave otherwise. “So we’ve just been faking how excited we are about her move back to L.A.,” Mary said. Melissa last month put down a deposit on a new apartment in L.A. and began packing.
But the move is bittersweet. “I would never say the pandemic has been a blessing. I don’t believe that. I think it’s been horrible and caused a lot of pain and trauma for a lot of people,” Melissa said. “But it has put things in perspective, and taught me, anyway, the kind of life I want to be living after this.”

By the numbers
California cases, deaths and vaccinations as of 7:44 p.m. Wednesday:

Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Across California
Maybe you’re already walking around without a mask. I’ve been going barefaced outside on trails and on the street when there aren’t too many people around. As soon as I get close to anyone, though, or go inside anywhere but my own home, I put mine on. I’m fully vaccinated — but I’m extra cautious, and it’s seemed the sociable thing to do.
But when California reopens Tuesday, anyone who’s been vaccinated can go without masks just about (but not quite) anywhere, state officials confirmed Wednesday. Tell me you’re not looking forward to that! (You’ll find the exceptions below.)
Those who haven’t been vaccinated will still be required to mask up in public indoor settings, such as retail stores, movie theaters and restaurants when not eating or drinking.
The change squares with guidelines the federal Centers for Disease Control and Prevention put out nearly a month ago. Dr. Mark Ghaly, California’s health secretary, said the state’s updated guidance “follows the science as we know it today.”
How the rules will be enforced is … interesting. Ghaly said businesses can implement some kind of vaccine verification routine, depend on the honor system or require everyone to wear a mask — but they can’t prevent people from wearing masks when they want to.
Workplaces, meantime, will be subject to standards set by the state Occupational Safety and Health Standards Board.
So where will vaccinated people still have to mask up? Exceptions to the face liberation announcement will apply to anyone at transit hubs or aboard public transportation; in healthcare settings and long-term care facilities; indoors at K-12 schools, child-care facilities or other youth settings; in homeless shelters, emergency shelters and cooling centers; and in correctional facilities and detention centers.
Ditching masks is just one more small reason to aim for herd immunity. L.A. isn’t expected to reach it until late summer. But San Francisco, which had imposed some of the most restrictive lockdown measures in the country and scored the second-highest rate of vaccinations in the state, appears to be nearing that community health goal.
“I think San Francisco is pretty close,” said UC San Francisco epidemiologist Dr. George Rutherford, who believes north of 75% of a population probably needs to be immune, either through vaccination or from surviving a previous infection, before herd immunity is achieved. “I think we’re in really good shape here, here meaning the city [of San Francisco]. Other places, we’re plenty close.”
Once herd immunity is achieved, new coronavirus cases introduced among unvaccinated people, such as through travelers, are unlikely to spread beyond a small outbreak or to start growing exponentially throughout a community. That means that even people without immunity to a disease are indirectly protected.
California already boasts low COVID-19 hospitalization rates, with roughly 1,000 COVID-19 patients in hospitals, down from about 22,000 in January. That’s a rate of about 2.6 Californians hospitalized with COVID-19 for every 100,000 residents, down from a peak of 56 per 100,000 residents.
The latest number is significant. Dr. Monica Gandhi, a UC San Francisco infectious-disease specialist, suggested in April that a good milestone for when restrictions like masking and social distancing can ease is when hospitalization numbers fall below 5 for every 100,000 residents. During the peak of the flu season, hospitalization rates for the flu on average top out at about 20 to 40 per 100,000 residents.
“We will see on June 15 if we stay at low cases — I actually have no doubt that we will,” Gandhi told The Times.
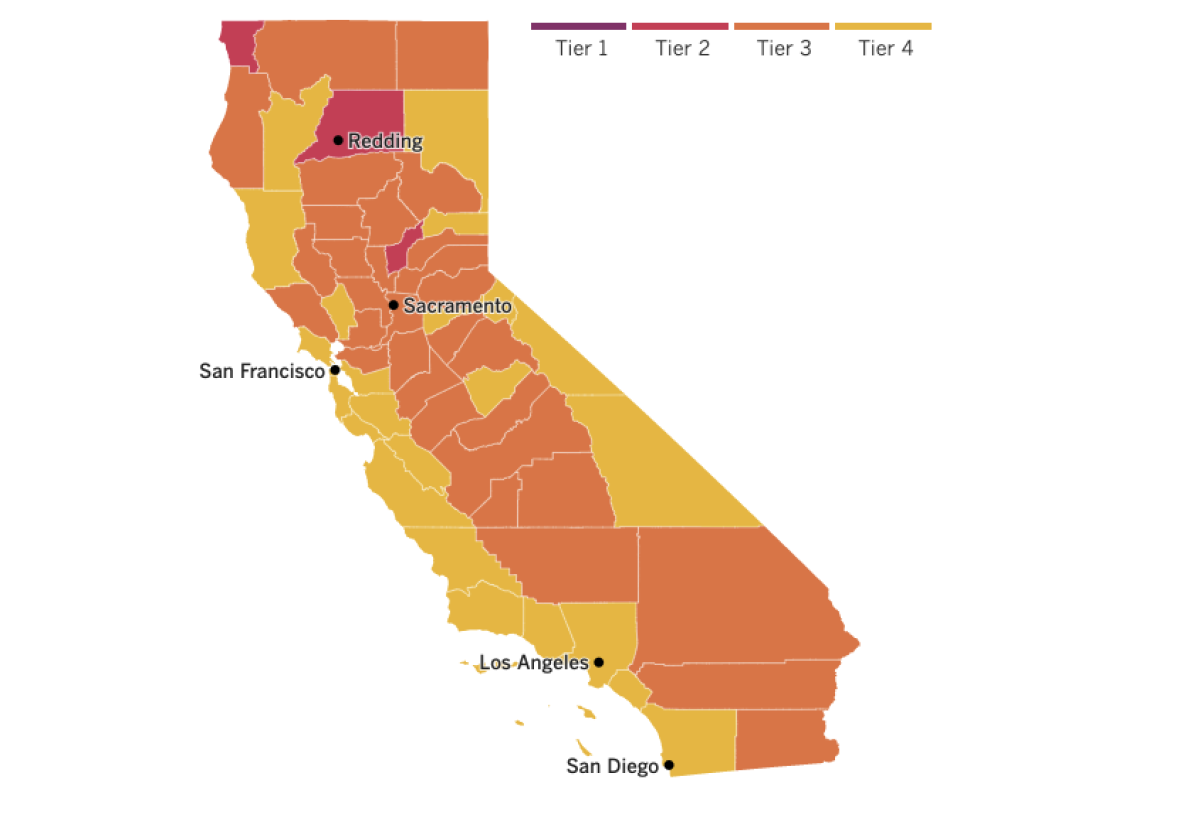

See the latest on California’s coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
As if COVID-19 were not bad enough, the U.S. saw steep rises in death rates for heart disease and diabetes, along with other common killers, in 2020. A big reason, health experts believe: People stayed away from hospitals, even when serious symptoms struck, for fear of catching the coronavirus. The year marked the biggest jump in heart attack and diabetes death rates in at least 20 years.
“When hospitalization rates for COVID would go up, we would see dramatic declines in patients presenting to the emergency room with heart attacks, stroke or heart failure,” said Dr. Donald Lloyd-Jones, a Northwestern University researcher who is president-elect of the American Heart Assn.
Another possible reason death rates went up, he said, is that many people stopped taking care of themselves during the crisis, with some gaining weight or cutting back on their medications. Experts said the stress of the crisis, job losses and the lockdown-related disappearance of exercise options were also factors.
That said, the death rate from the nation’s No. 2 killer, cancer, continued to decline, down about 2% in 2020 — similar to drops in recent years. But COVID-19 still may figure in: Lloyd-Jones theorizes that COVID-19 intervened and became the primary cause of death for patients weakened by cancer.
In Haiti, COVID-19 itself remains a major killer. The few Haitian hospitals treating cases of the disease have been so swamped in recent days that they report turning away patients, while plans to open another hospital to treat the infected have been delayed.
Official numbers for the nation of 11 million people show just 2,271 cases and 62 deaths over the last month. But experts say the numbers don’t yet account for a sudden spike in new cases, the largest in Haiti since the virus first hit.
Furthering the spread: Haiti hasn’t received a single vaccine, though officials say they expect to get 130,000 AstraZeneca doses this month. Even when vaccines arrive, experts worry many people may decline it — some for fear of venturing through crime-wracked neighborhoods to reach a clinic.
One woman mentioned such dangers as one reason why she avoided getting tested. Like many Haitians, she turned to a home remedy — in her case, a tea made with parsley, garlic, lime, thyme and cloves.
Also at the back of the pack when it comes to vaccines are countries in Africa. In South Africa, only 0.8% of the population is fully vaccinated, according to figures from Johns Hopkins University; in Nigeria, only 0.1% is, in a country of more than 200 million people. There are at least five other countries on the continent where not a single dose has been delivered, according to the Africa Centers for Disease Control and Prevention.
“It is extremely concerning and at times frustrating,” said Africa CDC Director Dr. John Nkengasong, a Cameroonian virologist who is trying to ensure that some of the world’s poorest nations get a fair share of vaccines in a marketplace where they can’t possibly compete.
He called on wealthy nations to get vaccines to Africa to avert a “moral catastrophe.”
A new initiative from the Biden administration should help. It will buy 500 million doses of Pfizer’s COVID-19 vaccine to donate to the COVAX partnership serving impoverished nations, signaling a massive new investment in the worldwide inoculation campaign, my colleagues in Washington report. The plan is expected to be announced Thursday.
Your questions answered
Today’s question comes from readers who want to know: What happens if I lose my vaccination card?
You get your COVID-19 vaccination. You’re given a card that includes your name, birthday, which vaccine you got and when.
Then you lose your card. A lot of people do, anyway. I lost mine.
It’s a common enough problem that Times intern Madalyn Amato tackled it in a how-to article back last week, and we brought you some tips back in April. But having dealt with this myself, I thought I’d share my own experience, too.
That experience was instruction enough that when my high-school-age daughter became eligible and got her first injection, we made sure to take a picture of the card and keep it on her phone.
So what happens if you lose your card? If you live in L.A. County, there are at least two options, Amato writes:
1) A company called Healthvana works with the L.A. County Department of Public Health to store a digitized version of your COVID-19 vaccination record. You can access it from any internet-connected device. If you have an iPhone, you can download the record into Apple Wallet.
Typically, Healthvana sends an email or text message to shot-getters, with instructions. Instructions, along with advice on how to avoid falling prey to a scam message, can be found at the county public health website.
Note that this digital record does not necessarily qualify as a “vaccine passport.” It’s also not considered a valid legal form of identification.
It could take several weeks to receive your Healthvana message. If you don’t get it within a month of your shot, contact Healthvana through its website.
2) Digital vaccination records are also kept by the state-run California Immunization Registry, or CAIR. Your record should appear within two to three weeks of your shot. Then you need to send a health information release form, and wait up to 14 days. You can’t get a replacement of your physical card, but CAIR can send you a physical copy of your records.
I chose a third option. I lost the card for my first shot. I called my healthcare provider, Kaiser Permanente, and they said just come in for your second shot, we have your record.
After I was fully vaxxed, they gave me a new card. I immediately snapped a photo and kept the real thing in an envelope where I knew I could find it — on the far left side of my freshly organized sock drawer.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
Resources
Need a vaccine? Sign up for email updates, and make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Need more vaccine help? Talk to your healthcare provider. Call the state’s COVID-19 hotline at (833) 422-4255. And consult our county-by-county guides to getting vaccinated.
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




