Coronavirus Today: If COVID-19 won’t boost public health funding, what will?
Good evening. I’m Kiera Feldman, and it’s Thursday, May 20. Here’s what’s happening with the coronavirus in California and beyond.
It’s hard to imagine a situation that would highlight the value of public health agencies more than a global pandemic. At all levels of government, public health workers have been instrumental in mapping out the extent of the coronavirus crisis and formulating a strategy for overcoming it.
So how does California Gov. Gavin Newsom express his appreciation for this hard work? By denying a request from local public health leaders to include $200 million for them in his new proposed state budget.
That’s the charge from healthcare advocates who say Newsom’s budget would return the state to a dangerous, years-long pattern of underfunding local public health agencies despite the glaring inadequacies exposed by the COVID-19 pandemic, my colleague Melody Gutierrez writes.
“No one realizes that we’re necessary or we exist until something like COVID happens,” said Dr. Flojaune Cofer, senior director of policy for Public Health Advocates. “We need to make a consistent investment in our infrastructure and in prevention, because that’s how prevention works. You can’t wait until you’re in the midst of a crisis to prevent, you have to have the dollars in advance.”
Local health departments have grown used to doing more with less. Budget cuts made during the Great Recession in 2008 have remained in place, even as the state’s population has grown. Between 2006 and 2020, California’s health departments saw their funding reduced by $138.5 million, according to the County Health Executives Assn. of California.
That has resulted in lab closures, staffing shortages and the elimination of programs that reduce chronic diseases — including some that make people more susceptible to COVID-19.
“The biggest lesson of COVID-19 is that waiting until a crisis to invest in public health costs lives,” said Elsa Jimenez, health director at the Monterey County Health Department. “We can’t repeat the same mistakes California made before COVID-19.”
Newsom’s budget plan calls for a $3-million study to determine how much public health programs need so that the money can be included next year. (In the meantime, he said his budget earmarks $300 million for public hospitals and cash for expanding the Medi-Cal system for low-income Californians.)
Advocates said they see no reason to wait. The state has seen a massive tax revenue windfall, resulting in $38 billion in discretionary cash.
During the pandemic, city and county public health leaders had to abandon fundamental public health functions — such as contact tracing, communicable disease testing and enforcement of public health orders — because they did not have enough staffing or resources, according to Kaiser Health News.
With an additional $200 million a year, public health leaders said they could hire more nurses and epidemiologists, pay for new public health laboratories, and rebuild obsolete data systems that failed during the pandemic and cost lives.
“We identified all these needs before COVID,” said state Sen. Richard Pan (D-Sacramento), a pediatrician who is chair of the Senate Health Committee. “And yet we didn’t step up, so now is the time to step up.”
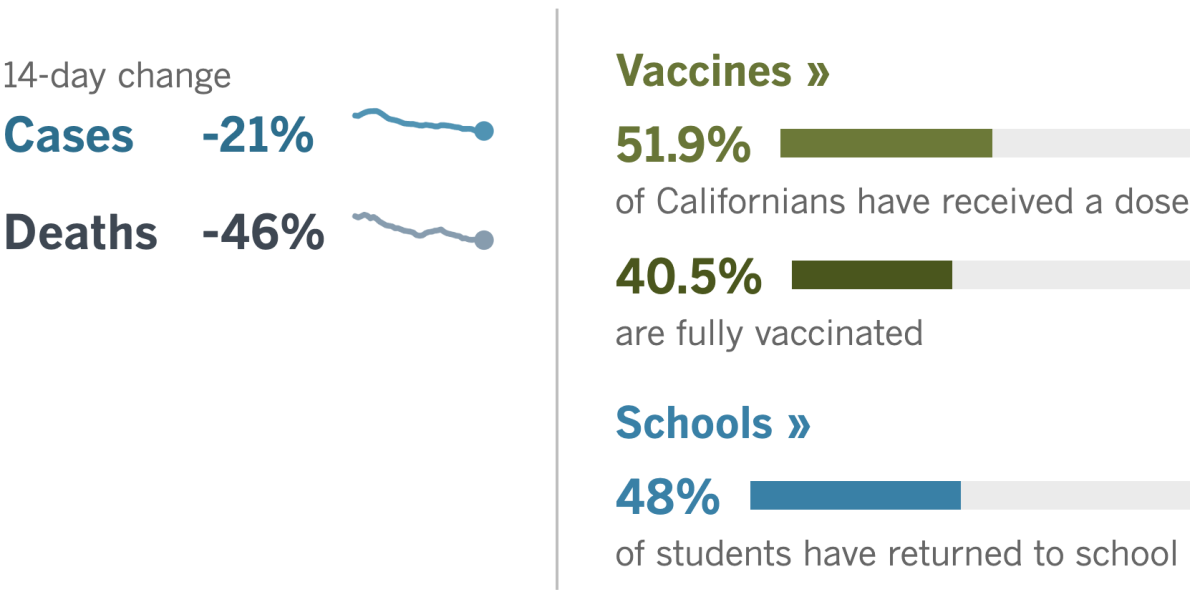
By the numbers
California cases, deaths and vaccinations as of 5:20 p.m. Thursday:

Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Across California
If you were waiting with bated breath for California to decide on new rules around masking for fully vaccinated workers, I have some bad news for you: They are staying the same for now.
A state workplace safety board met on Thursday and postponed their vote on a proposal that would have allowed workers to return to their jobs without social distancing or face masks so long as everyone in the workplace is vaccinated.
The move came after the deputy chief of the California Division of Occupational Safety and Health, known as Cal/OSHA, asked the seven-member board to hold off on voting so that the agency could come up with a new proposal and present it at the next meeting on June 3.
In delaying the vote, a few board members expressed reservations about lifting mask restrictions too soon — even though the U.S. Centers for Disease Control and Prevention has already relaxed its recommendations.
“I don’t think it’s the time to roll back protections. I think the CDC guidance on May 13 was a bit premature,” board member Barbara Burgel said. “It shifts the responsibility to individual employees to try and sort out, ‘How are we going to know if our co-workers are vaccinated? How do we know if vaccinated individuals have symptoms?’”
Other members of the board wanted to make sure the state didn’t bungle the reopening.
“Our message should be: We’re getting to the end of this. Hopefully we’re getting to a place where we can open things up,” said board chair David Thomas. “We just don’t want to get — for lack of a better word — we don’t want to get stupid.”
For now, workers must continue to wear masks and practice physical distancing both indoors and outside. Workers can remove masks when alone or when eating or drinking, but in those cases, they must be physically distant from others.
Even as the pandemic recedes in California, the workplace is likely to remain fraught territory. Companies are obligated by law to provide safe workplaces, and labor lawyers are predicting a surge in lawsuits and complaints to oversight agencies like Cal/OSHA.
Can you refuse to be vaccinated and still keep your job? Can you sue if the guy in the cubicle next to you won’t wear a mask? There are no clear answers.
Dozens of lawsuits were filed last year by blue-collar warehouse and meatpacking employees who could not work from home. Now suits from white-collar office workers are starting to make their way through the courts too.
Workers may find themselves going up against the limits of the law.
“We’ve not had anything like this pandemic in a hundred years,” said UC Berkeley law professor Catherine Fisk. “And employment laws were developed fairly recently when infectious diseases were not a major threat, other than the annual flu.”
In other news, California’s eviction protections are expiring at the end of June, and cash to help renters has gone unspent.
Months ago, the state approved $2.6 billion to help tenants pay rent amid hardships caused by the COVID-19 pandemic. But few people applied for the rental assistance because of confusion and bureaucratic red tape, advocates say.
Newsom last week proposed doubling the amount available for rent relief to $5.2 billion, but the state doesn’t have any concrete plans on the table yet.
A U.S. Census survey in December found that more than 1.9 million adult Californians living in rental homes reported being behind on their rent. Housing advocates say California needs to do a better job of helping them get the assistance they need.
“We stand on the precipice of an eviction cliff, and unless the state protections are extended and this program is simplified, our communities will be thrown off the edge and destroyed,” said Elena Popp, executive director of the nonprofit Eviction Defense Network.
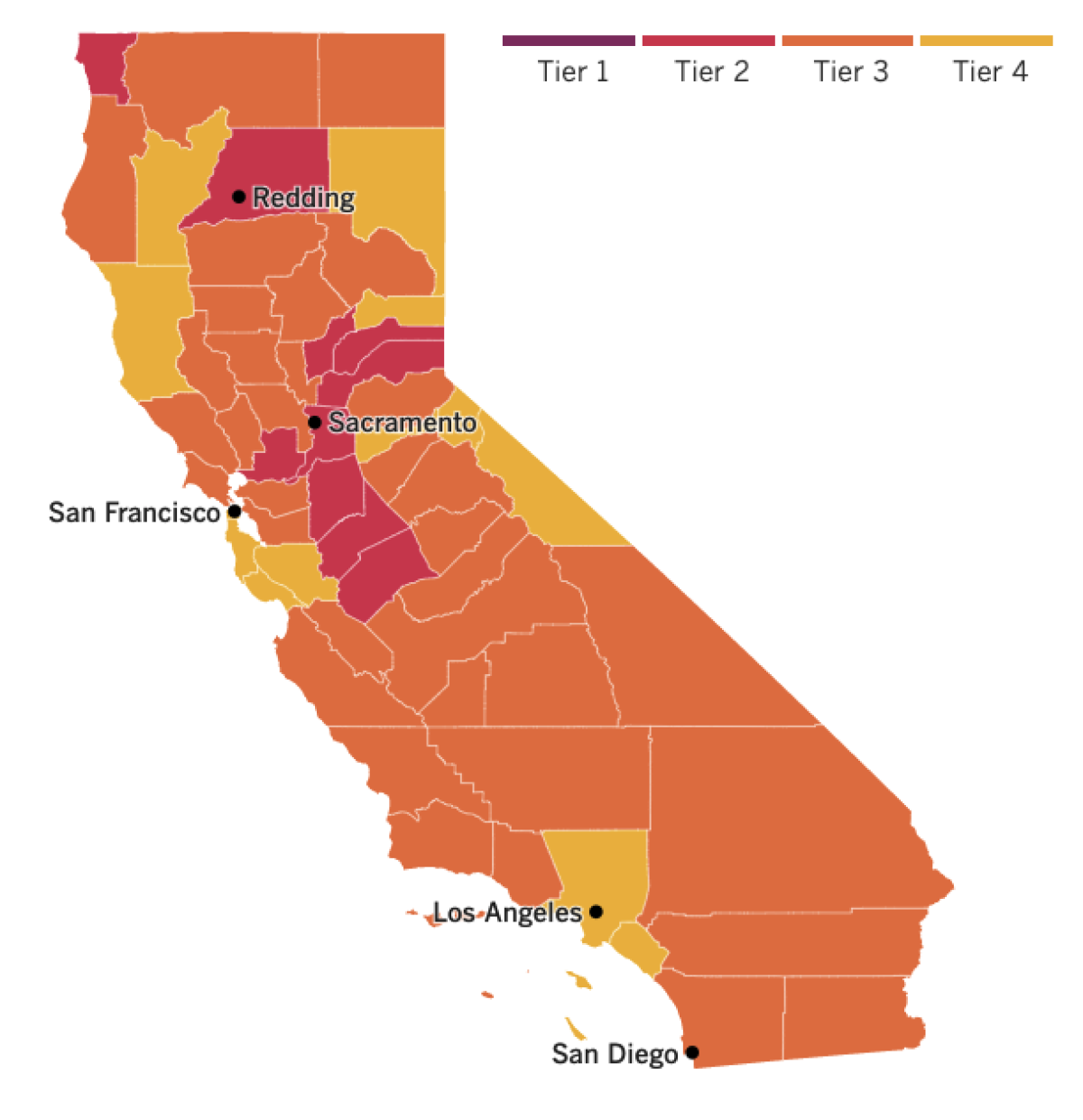

See the latest on California’s coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
The head of the World Trade Organization said Thursday that vaccine production must be diversified in order to contain the COVID-19 pandemic.
WTO Director-General Ngozi Okonjo-Iweala said the world has the capacity to manufacture about 5 billion vaccine doses overall but that as the virus has spread “we require twice and three times that.”
Vaccine production is 80% concentrated in 10 European, North American and South Asian nations, Okonjo-Iweala said.
“It’s not normal that Africa, with 1.3 billion people, has 0.17% of the manufacturing capacity of the world,” she said, adding that Latin America has about 2% of global production capacity. “This has to change.”
In Japan, officials on Thursday gave preliminary approval to the COVID-19 vaccines developed by Moderna and AstraZeneca. Formal approval is expected Friday after a broader vaccine policy panel signs off, officials said.
So far, the Pfizer-BioNTech vaccine is the only one available there.
Only 4% of the population has received a dose of COVID-19 vaccine, but Japan is working to boost that figure in advance of the Tokyo Olympics.
Recent polls have found that more than 80% of Japanese residents are opposed to hosting the Olympics this summer. Political leaders hope that picking up the pace of vaccinations will tamp down public concerns about the safety of the Games.
Here in the U.S., the problem is not supply but demand, and health experts are worried about big gaps they’re seeing in vaccine rates nationwide.
While Massachusetts has nearly hit its goal of administering 4 million doses, clinics in Alabama are shutting down because interest in the shots has plunged.
For the past month, every American adult who has wanted a shot could get one. Under these circumstances, the geographic patterns that have emerged are hard to ignore.
The highest vaccination rates are concentrated in the Northeast, while the lowest ones are mostly in the South. Vaccine disparities are also seen between rural and urban areas.
Dr. Eric Topol, head of the Scripps Research Translational Institute, said the gaps in COVID-19 vaccination could be traced to “anti-science” attitudes among Republican leaders who were skeptical about the value of masks. Getting more people vaccinated will take continued education, incentives and “head-on” confrontation of misinformation, he said.
Closing the gaps is vital to controlling a disease that has killed 588,000 people in the U.S., health experts say. Nationwide, COVID-19 vaccines have helped drive U.S. cases down to their lowest level since last June and reduced deaths to about 570 a day, a level not seen since last July.
“Low vaccination rates will leave room for the virus to circulate, reemerge and possibly form new variants,” said Tara Kirk Sell, a senior scholar at the Johns Hopkins Center for Health Security. “High vaccination rates are critical to keeping the disease under control, especially when we get back to the fall and winter.”
Your questions answered
Today’s question comes from readers who want to know: How will stores know if customers and employees are vaccinated?
This will become a really important issue in California come June 15, when the state is planning to adopt the CDC’s recommendations and allow people who are fully vaccinated to go unmasked indoors.
The state is still hammering out the logistics of how this policy will be enforced in businesses, according to Dr. Mark Ghaly, California’s Health and Human Services secretary.
“There’s different ways to implement it,” Ghaly said this week. The goal is to develop a plan “with a high degree of integrity with continued focus on protecting the public.”
Here in L.A., officials have hinted that it’ll be an honor system kind of thing.
“There is no way to determine onsite whether another person is vaccinated or not,” said County Public Health Director Barbara Ferrer.
That may sound disturbing to some, but Ferrer seemed unfazed.
“We have come this far by taking care of each other, and to end this pandemic, we’ll need to remain willing to follow sensible safety modifications that make it possible to reduce cases and outbreaks while we increase the number of residents that are fully vaccinated,” she said.
And actually, there is a way to determine a person’s vaccination status at the entrance of a store: a “vaccine passport” system. This would allow people who are fully vaccinated to provide proof of their status, perhaps with a certificate on their smartphones.
Theoretically, if California adopted a statewide vaccine passport program, L.A. County would have to implement it. But, so far, state officials haven’t said that they have any plans to go this route.
There is public support for vaccine passports, though. A recent poll found that a majority of Californians support requiring proof of COVID-19 vaccination or negative test results at workplaces, entertainment venues and elsewhere.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
Resources
Need a vaccine? Sign up for email updates, and make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Need more vaccine help? Talk to your healthcare provider. Call the state’s COVID-19 hotline at (833) 422-4255. And consult our county-by-county guides to getting vaccinated.
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




