Coronavirus Today: ‘Why have people like me been forgotten?’
Good evening. I’m Amina Khan, and it’s Monday, Jan. 11. Here’s what’s happening with the coronavirus in California and beyond.
As healthcare workers line up to receive their shots in California, many are being asked to provide proof that they’re in this high-priority group. But some healthcare workers say they haven’t gotten access to the shot and are being left behind because they’re independent practitioners who don’t work directly for a hospital or health system.
One of those workers is Tania McCracken, a midwife in the Inland Empire who spends hours inside the homes of pregnant women, helping to deliver newborns. It’s hands-on work that involves a lot of close contact — and thus, a higher risk for catching the coronavirus. And yet McCracken and many other state-licensed midwives have not yet been able to get their shots. So far, the health systems that were given some of the first supplies of vaccine have focused on inoculating their own staffs.
Midwives aren’t the only health workers being left behind, my colleague Melody Petersen writes. Dozens of physicians, nurses, physical therapists and others who are not directly employed by hospitals posted pleas on a website that had sought public comment on a state vaccine advisory committee’s efforts to distribute the shots. Many pointed out that their jobs don’t allow them to stay the recommended minimum of six feet away from others.
“Why have people like me been forgotten?” Erin Newman, a self-employed audiologist in Orange County, wrote to the committee. Newman said she spends 45 minutes with each of her patients as she evaluates their hearing, often sitting just inches away. In theory, she should fall squarely in the vaccine priority group. But the local medical system she reached out to told her its doses were for its own staff.
The challenges of getting the vaccine to this overlooked group of health workers may be a harbinger of greater difficulties to come. Self-employed Californians in other industries could face similar problems getting their shots, even if they qualify for access.
After health workers and nursing home residents, priority will expand to workers in education, child care, emergency services, and food and agriculture, as well as Californians age 75 and up. Next in line are workers in transportation and critical manufacturing, along with people who are 65 to 74 years old. After that come workers in industries such as utilities, defense, energy, communications and financial services.
Already, some self-employed workers in these next-in-line industries are worried they’ll be pushed to the back of the queue simply because they don’t have a corporate badge that serves as proof of their work.
“I am a self-employed teacher, and my wife is a childcare provider,” Lee Young wrote to the committee. “We both work with children, but we own our own business. … We need your help to ensure that we are not left behind.”
By the numbers
California cases, deaths and vaccinations as of 7:03 p.m. PST Monday:

Track the latest numbers and how they break down in California with our graphics.
Across California
California passed another tragic milestone this weekend, logging its 30,000th death from COVID-19 — and then some. Since the most recent surge began washing over the state in November, deaths have been piling up more and more quickly. California was counting about 40 deaths a day on Nov. 3, around 70 deaths per day by Thanksgiving and about 220 deaths per day by Christmas. By Sunday night, California was logging an average of 481 deaths per day over the previous week.
To understand the severity of the surge, consider this: It took about six months for California to record its 10,000th death (on Aug. 6), four more months to record its 20,000th death (on Dec. 8) and just about one additional month to record its 30,000th death on Jan. 10, according to a Times analysis. Five of the highest single-day death tallies for California have been logged in the last week alone.
The post-Christmas surge continues to ravage Los Angeles County, where the daily average number of new infections on Thursday, Friday and Saturday was about 18,000 — far above the average of 14,000 logged over the previous week. On Saturday, the county recorded its 12,000th COVID-19 death and its 900,000th coronavirus infection.
“This very clearly is the latest surge from the winter holidays and New Year’s — no question about it,” Dr. Paul Simon, the L.A. County Department of Public Health’s chief science officer, said Friday. “It had gradually started earlier in the week, but [definitely is] here in the last day or two.”
The surge is devastating local hospitals, which are running low on much-needed supplies, space and staff. Emergency medical technicians are struggling to offload patients, who may be sitting in an ambulance waiting for a bed for up to 17 hours. And the worst is likely yet to come, as doctors, nurses and other workers brace for the impact of another influx of COVID-19 patients infected during the recent holidays.
“It’s a war zone,” said a doctor at an L.A. County public hospital. “The way most people leave is by dying.”
The problem right now is in many ways as simple as it is devastating: Patients are being admitted to hospitals faster than they’re being discharged. This has placed an onerous burden on discharge planners, who are desperately trying to free up beds in hospitals drowning in COVID-19 patients. My colleague Brittny Mejia describes their daily work as a jigsaw puzzle, trying to figure out where to make patients fit.
“If there is another place for them to go we need to let that patient go to that other bed … because there’s somebody else who’s dying right now and they need a bed,” said Suzette Shields, a clinical social work supervisor at Harbor-UCLA Medical Center.
The rising death toll means funeral homes and private mortuaries are having to turn families away, and hospital morgues are being overwhelmed. The California Governor’s Office of Emergency Services has been preparing to dispatch 88 refrigerated trailers around the state to supplement morgue space.
“This is a mass casualty, a mass fatality event that our county is experiencing,” said Dr. Rais Vohra, Fresno County’s interim health officer.
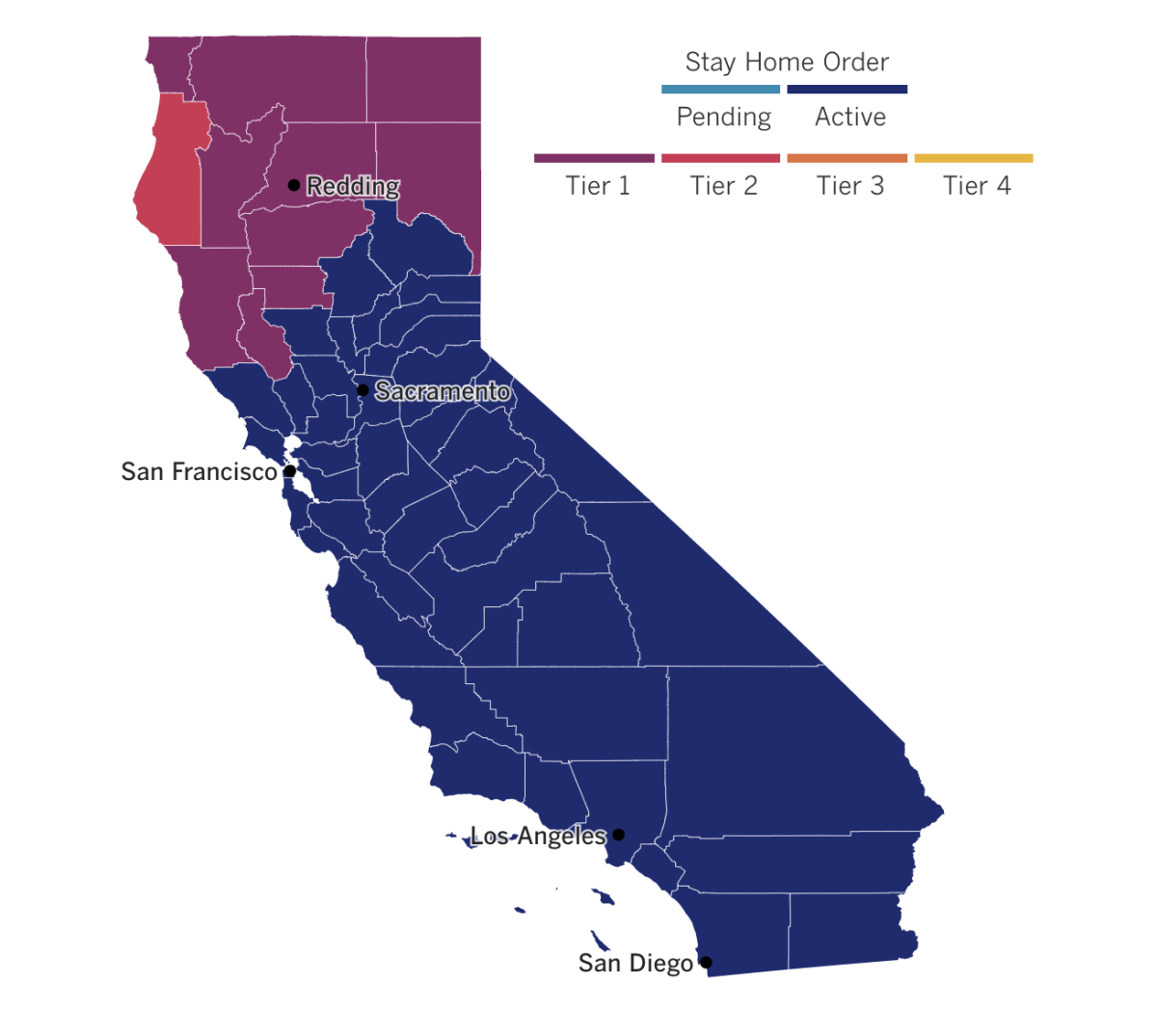
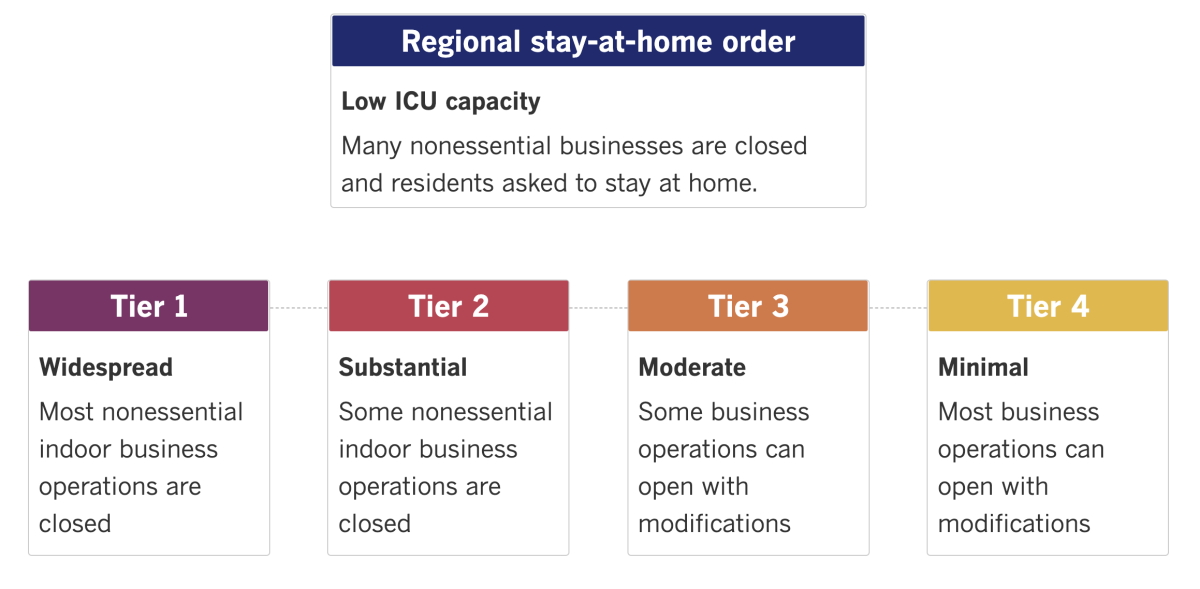
See the latest on California’s coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
In Washington, Rep. Bonnie Watson Coleman (D-N.J.) said Monday she has tested positive for COVID-19 and believes she contracted the coronavirus while she and other lawmakers were forced to shelter in place last week as a violent mob loyal to President Trump attacked the Capitol.
Watson was among dozens of lawmakers whisked to a secure, undisclosed location when the pro-Trump insurrectionists broke through barricades, invaded offices and ransacked the building. A statement from her office pointed out that “a number of members within the space ignored instructions to wear masks.” So far, her symptoms are “mild,” according to the statement.
The news comes a day after Capitol attending physician Dr. Brian Moynihan notified lawmakers that they may have been exposed to an infected individual while sheltering in place. He urged them to get tested.
“Many members of the House community were in protective isolation in the large room — some for several hours,” Moynihan wrote. During that time, “individuals may have been exposed to another occupant with coronavirus infection.” The infected person was not identified.
Some lawmakers and staff were furious after video surfaced of Republican lawmakers not wearing masks in the room. Among the maskless: newly elected Georgia Rep. Marjory Taylor Greene, a presidential ally aligned with a pro-Trump conspiracy theorist group.
Across the pond, Queen Elizabeth II and her husband, Prince Philip, have received their COVID-19 jabs. Buckingham Palace officials said Saturday that the 94-year-old monarch and Philip, 99, joined the 1.5 million people in Britain who have been given their first dose of vaccine. The shots were administered at Windsor Castle, where the royal couple have been spending their time during lockdown.
Officials said they took the unusual step of commenting on the queen’s health in order to prevent inaccuracies and further speculation. The queen “decided that she would let it be known she has had the vaccination,” a palace statement said.
Meanwhile, the new variant of the coronavirus that has emerged in the United Kingdom has made its way around the globe, and mounting evidence is confirming what some scientists had suspected: that it is a super-spreader capable of turbocharging the pandemic while pushing other less transmissible strains of the virus to the sidelines.
Two groups of researchers have concluded that the new strain’s rapid growth across Britain can’t be dismissed as a fluke. They used genetic data to time-stamp its spread in three distinct regions of England and found similar patterns of growth in all of them. Another type of genetic screening provided a separate signal that the strain was consistently able to outspread its competitors. And mathematical models also showed that the way the variant spread in different regions was too similar to be a coincidence — it had to be that the virus itself was more transmissible.
On the bright side, lest we forget, this particular strain is not thought to be any more virulent than its predecessors — that is, it won’t make folks sicker and it won’t raise their risk of death. It also appears to be just as susceptible to the COVID-19 vaccines.
In Ethiopia, the United Nations is worried about “massive community transmission” in the troubled Tigray region, whose population of 6 million has been made vulnerable by a military conflict that displaced residents and interrupted coronavirus surveillance and control work for more than a month, according to a new U.N. report.
The U.N. describes a “dire humanitarian situation” in the region, with food scarcity leaving 4.5 million people in need of emergency food assistance. To make matters worse, “only five out of 40 hospitals in Tigray are physically accessible,” the report said. Most of the remainder have had supplies and equipment stolen, and many are reportedly destroyed, it went on.
Ethiopia has one of the highest coronavirus caseloads in Africa, with more than 127,000 confirmed infections. Although its daily case rate has fallen in recent weeks, officials have not said whether those numbers include data from the Tigray region.
Your questions answered
Today’s question comes from readers who want to know: How many U.S. states have the coronavirus strain from the United Kingdom?
At least nine so far, and that number is sure to grow.
First, a little background: The coronavirus strain that’s making people anxious is known as B.1.1.7, and it has 17 specific genetic changes that set it apart from its predecessors. Scientists are still working out what each of those changes does, but it’s clear that when they’re combined, they boost the virus’s capacity to spread.
British researchers reported last week that their homegrown variant is about 56% more transmissible than typical coronavirus strains. (That figure could be anywhere between 40% and 70%, they said.) In real-world conditions, a single person infected with B.1.1.7 could seed an outbreak that extends to as many as 16 people over the course of a month. By contrast, a person infected with a typical strain of coronavirus would cause only three new cases over the same period.
When British scientists first warned of the new strain’s super-spreading potential, Prime Minister Boris Johnson implemented lockdown measures for much of England, and many countries — the U.S. included — imposed restrictions on travelers from the U.K. But B.1.1.7 had already jumped the border. It’s now in at least 49 countries, including the United States.
The U.S. doesn’t have a comprehensive screening system to keep an eye out for new and potentially dangerous coronavirus strains. Still, at least nine states have detected the U.K. strain so far. Colorado was the first to do so, on Dec. 29.
As of Friday, the Centers for Disease Control and Prevention were aware of 63 cases in eight states — California, Connecticut, Florida, Georgia, New York, Pennsylvania and Texas in addition to Colorado. But that list is already out of date: On Saturday, Minnesota’s Department of Health announced that five cases involving the U.K. variant had been detected there.
Given the strain’s super-spreading ability, scientists say it’s just a matter of time before it makes its way to more states.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them.
Resources
Practice social distancing using these tips, and wear a mask. Here’s how to do it right.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




