Coronavirus Today: California cracks down — again
Good evening. I’m Amina Khan, and it’s Thursday, Dec. 3. Here’s what’s happening with the coronavirus in California and beyond.
Get ready, California. Residents will face sharp new limits on community outings and in-person shopping under a new statewide order aimed at preventing the state’s hospitals — and especially their intensive care units — from being overwhelmed with COVID-19 patients.
The rules, announced Thursday by Gov. Gavin Newsom, place restrictions on a range of activities in regions facing shortages in critical care resources — and they could potentially last through the holiday season.
The rules take effect Saturday, and despite initial indications that 11 counties in Southern California and 12 in the San Joaquin Valley could be required to implement the new restrictions immediately, state health officials later provided a list showing no regions currently at the threshold for closure — meaning no more than 85% of their intensive care unit beds are filled.
“The bottom line is, if we don’t act now, our hospital system will be overwhelmed,” Newsom said. “If we don’t act now, we’ll continue to see our death rate climb, more lives lost.”
Among the new rules: Hair and nail salons, playgrounds and family entertainment centers must close. Overnight stays at campgrounds are on hold. Restaurants can offer only takeout service, and retail businesses may operate at only 20% of indoor customer capacity at a time. Store officials will be required to ensure that no eating or drinking takes place inside.
After 21 days, any reopenings will be based on four-week projections of a region’s ICU capacity. This means the broad restrictions could stretch into January in some parts of California, given the strain on the state’s healthcare systems.
Keep in mind, California has averaged nearly 15,000 new coronavirus cases a day over the last week — a figure that has tripled over the last month. COVID-19 hospitalizations have also tripled over the same period. And over the last week, an average of 67 Californians have died of COVID-19 each day, a 60% increase from mid-November.
Some epidemiologists say state officials pretty much had to impose a strict shutdown; the alternative would have been to allow one of the worst public health disasters in the state’s modern history. Indeed, California’s death toll of close to 20,000 could double by the end of winter.
The initial coronavirus wave “has now become a viral tsunami,” said Dr. Robert Kim-Farley, a medical epidemiologist and infectious-disease expert at the UCLA Fielding School of Public Health. “The virus is now everywhere, and so, therefore, the restriction of activities needs to also be applied everywhere to be able to return to where we were — on a decreasing trend.”
By the numbers
California cases and deaths as of 4:11 p.m. PST Thursday:
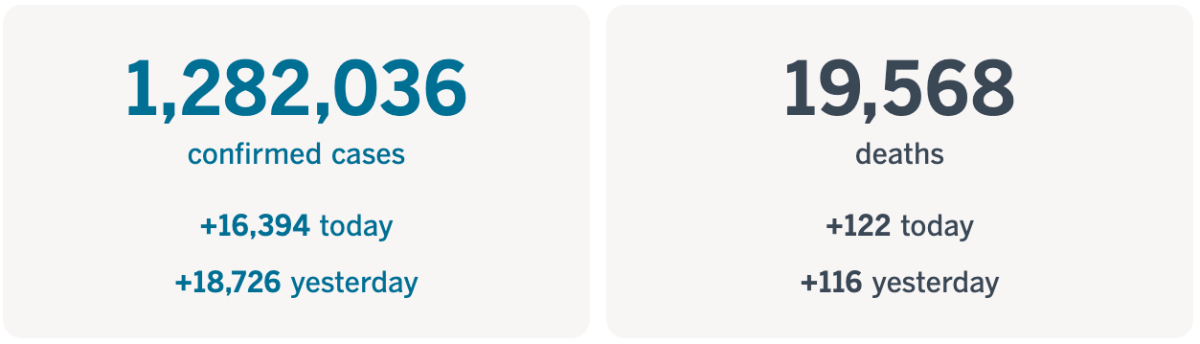
Track the latest numbers and how they break down in California with our graphics.
Across California
A new survey by the Los Angeles Unified School District is asking parents to make a major decision: Will you send your child back to school when campuses reopen?
It’s a particularly stressful time to be asking this question, with cases surging across the state. But the survey, which must be returned by Sunday, should provide the first set of comprehensive data on how parents of the district’s roughly 465,000 students are feeling about school safety and whether it’s a priority to reopen school campuses, my colleague Howard Blume writes.
Embedded in the survey are some of the same quandaries that health experts, educators and political leaders are wrestling with: How safe are schools? What are the risks? What’s best for my child?
The problem is that many unknowns and trade-offs factor into the return-to-school equation. It’s becoming increasingly apparent that distance-only learning may be harmful to many students who don’t have fast and reliable internet access, or the necessary technological tools, or parents who can assist them because they’re able to work from home, or even just a quiet space to study. Problems like these can exacerbate preexisting achievement gaps.
At the same time, returning to campus comes with its own set of dangers.
“I am worried that once children return to school they might bring the virus home, and those at higher risk, such as the adults and the older folks, might contract the virus,” said Yesica Aguirre, whose eighth-grade son attends Bell Gardens Middle School.
Meanwhile, many parents have also been up in arms since L.A. County closed outdoor public playgrounds this week in its effort to slow the surge in cases.
My colleague Hailey Branson-Potts spoke to Zachary Beckman, whose 2-year-old, Sydney, defied the yellow caution tape around Anderson Park in Redondo Beach and flopped over a swing. Just a few feet away, three adults played on a tennis court that was allowed to remain open. None wore a mask.
For many parents, the official dictates have added up to a confusing and frustrating mix of dos and don’ts.
“Parents are really taking the brunt of all this,” Beckman said. “I understand the need for safety, but the inconsistencies and lack of logic is very frustrating.”
Here’s some good news for food service workers: Los Angeles will offer a one-time $800 stipend to employees who work at restaurants, breweries, food stands and other related businesses, Mayor Eric Garcetti said Wednesday.
The Secure Emergency Relief for Vulnerable Employees, or SERVE, initiative will offer the financial aid to 4,000 workers using money from the nonprofit Mayor’s Fund for Los Angeles, Garcetti said. Some 4 out of 10 employees in the food service industry have lost their jobs this year, he added.
Eligible residents must be 18 or older and have earned no more than $58,450 in 2019. Applications open Monday, and the link to apply will be available on the SERVE initiative website.
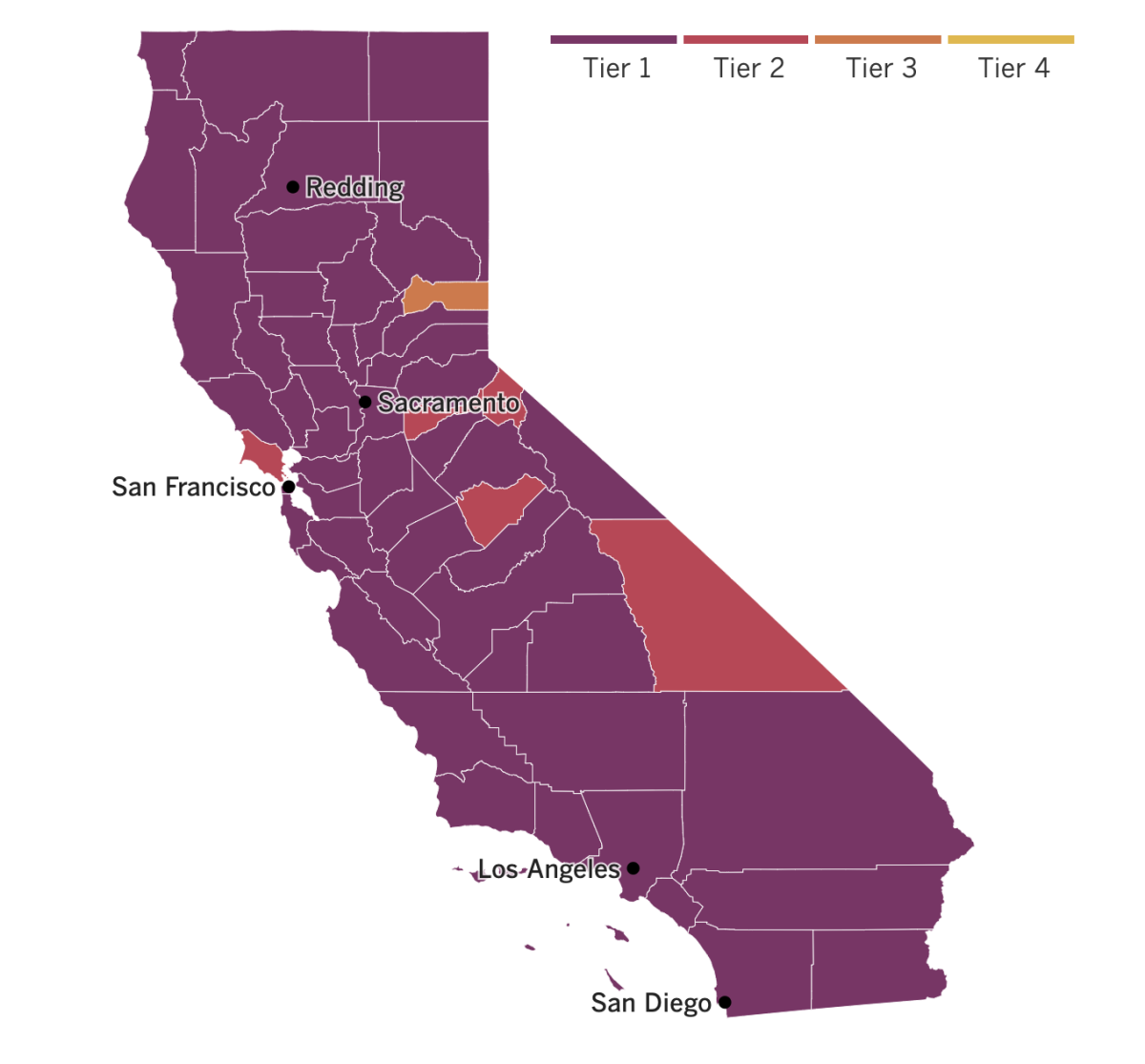

See the current status of California’s reopening, county by county, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
The United States recorded 3,157 daily COVID-19 deaths Wednesday. That single-day total, which beats the previous record set in the spring by more than 20%, is also greater than the number of people killed in the Sept. 11 attacks.
What’s more, the number of Americans hospitalized with COVID-19 passed 100,000 for the first time — it has more than doubled over the last month — and new cases now exceed 200,000 per day, figures released Thursday show.
These bleak trends reflect a deepening crisis in the U.S., with potentially worse to come when the toll from Thanksgiving becomes apparent. Millions of Americans ignored warnings to stay home and celebrate the holiday with members of their household and no one else.
“The reality is December and January and February are going to be rough times,” said Dr. Robert Redfield, head of the U.S. Centers for Disease Control and Prevention. “I actually believe they are going to be the most difficult time in the public health history of this nation.”
The forthcoming COVID-19 vaccines should help turn things around eventually, but only if Americans trust them enough to take them. Three former occupants of the Oval Office hope to do their part by rolling up their sleeves and persuading the public that if the vaccines are good enough for them, they’re good enough for anyone. Former Presidents Obama, George W. Bush and Clinton said they’d be willing to get a COVID-19 vaccine publicly once one becomes available.
“I promise you that when it’s been made for people who are less at risk, I will be taking it,” Obama said during a radio interview, adding, “I may end up taking it on TV or having it filmed, just so that people know that I trust this science.”
Clinton would “definitely” be willing to get a vaccine as soon as one is available to him, a spokesman said.
And Bush’s chief of staff, Freddy Ford, said that the former president asked him to meet with Dr. Anthony Fauci, the nation’s top infectious-disease expert, and Dr. Deborah Birx, the White House coronavirus response coordinator, to tell them that “when the time is right, he wants to do what he can to help encourage his fellow citizens to get vaccinated.” And he would “gladly do so on camera,” Ford added.
All three presidents said they would wait for their proper turn in line, allowing for those who need the vaccine most to get it first.
In Russia, President Vladimir Putin has ordered a “large-scale” COVID-19 immunization campaign to start by late next week. Doctors and teachers will be the first in the queue to get a domestically developed vaccine that has not yet made it through advanced clinical trials to ensure its safety and effectiveness.
The move came Wednesday, hours after Britain became the first country in the West to authorize the use of a COVID-19 vaccine — the one developed by Pfizer and Germany’s BioNTech — and the first to do so after Phase III clinical trials.
Russia has promoted its space-race-named Sputnik V as the world’s “first registered COVID-19 vaccine” after giving the inoculation regulatory approval in early August. But the authorization drew criticism from experts at the time because the shots had been tested only on several dozen people. According to Putin, one of his daughters was among those early recipients.
Your questions answered
Today’s question comes from readers who want to know: Who will be the first to get the vaccine in the U.S.?
My colleague Thomas Curwen has put together a handy primer on what we know so far about the vaccines that are soon to be available in the United States.
The CDC’s Advisory Committee on Immunization Practices met this week to vote on who should be at the front of the line to receive the first shots of a COVID-19 vaccine. Their recommendation: Focus on front-line healthcare workers as well as residents of long-term care facilities, such as nursing homes and assisted-living facilities. More groups will be eligible as more vaccine becomes available.
These recommendations are not binding on the state officials who will make the final decisions about vaccine distribution. But the guidance does “carry great importance for public health and medical officials,” said Dr. Kelly Moore, associate director of the Immunization Action Coalition, a nonprofit that provides information about vaccines and their distribution.
The committee’s decision is meant to help states as they prepare to receive and distribute COVID-19 vaccines, a process expected to begin this month. And states may have to make more detailed decisions, such as whether to put emergency room doctors and nurses ahead of other healthcare workers if vaccine supplies run low.
The committee will meet again to vote on specific vaccines once they have passed muster with the Food and Drug Administration.
And it will also decide at a later date who will come next in the vaccination queue. Among the candidates: teachers, police, firefighters and other essential workers such as those in food production and transportation; elderly people and those with underlying medical conditions.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them.
Resources
Practice social distancing using these tips, and wear a mask. Here’s how to do it right.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




