Coronavirus Today: Where did California go wrong?
Good evening. I’m Amina Khan, and it’s Wednesday, Nov. 18. Here’s what’s happening with the coronavirus in California and beyond.
As recently as last month, California seemed to be beating the odds. Health experts attributed much of its success to its imposing a stay-at-home order relatively early. Now, the Golden State is in the middle of the worst surge it’s seen since the start of the pandemic.
Where did we go wrong? That question is surely on the minds of many Californians facing a new round of rules and restrictions. The answer is simple, according to my colleague Rong-Gong Lin II.
“We actually do know how to fight the virus,” he writes. “We just got tired of doing it.”
He lays out how a combination of psychological fatigue and economic pressures brought us to this humbling point in the pandemic — and how it might fuel a third wave of cases that could set new records for mortality.
Back in the spring, the state’s swift response flattened the curve as intended, but it also triggered a reaction that has left us more vulnerable. The stay-at-home order devastated the economy and drew pressure from business owners to reopen. And attitudes toward social distancing guidelines began to change.
“California shows how a collective shrug, a lack of discipline and a yearning to quickly ‘get back to normal’ can also result in a new season of death,” Lin writes.
Relaxed rules for restaurants and bars, plus a burst of social activity in late spring and early summer, wound up sabotaging efforts to reopen schools in the fall as the death toll mounted.
Resentment toward the pandemic restrictions led some to defiantly hold parties and gather together without masks. Even Gov. Gavin Newsom succumbed to temptation and attended a birthday dinner with people from other households at an exclusive Napa Valley restaurant. The governor later apologized for making that choice.
Now, with Thanksgiving, Christmas and other winter holidays tempting many to travel, officials fear that California is setting itself up for a deadly winter.
“Traditional social gatherings held amid the world’s worst pandemic in a century will lead to a season of heartbreak, overwhelmed hospitals and busy morgues as the weeks tick closer to Christmas,” Lin writes.
That’s why health officials are begging Californians to sit this holiday season out.
“Please choose to be part of the solution because it’s going to take all of us to avoid increased heartbreak,” Barbara Ferrer, the Los Angeles County director of public health, said recently. “We’re actually recommending this Thanksgiving be a stay-at-home Thanksgiving.”
By the numbers
California cases and deaths as of 3:02 p.m. PST Wednesday:

Track the latest numbers and how they break down in California with our graphics.
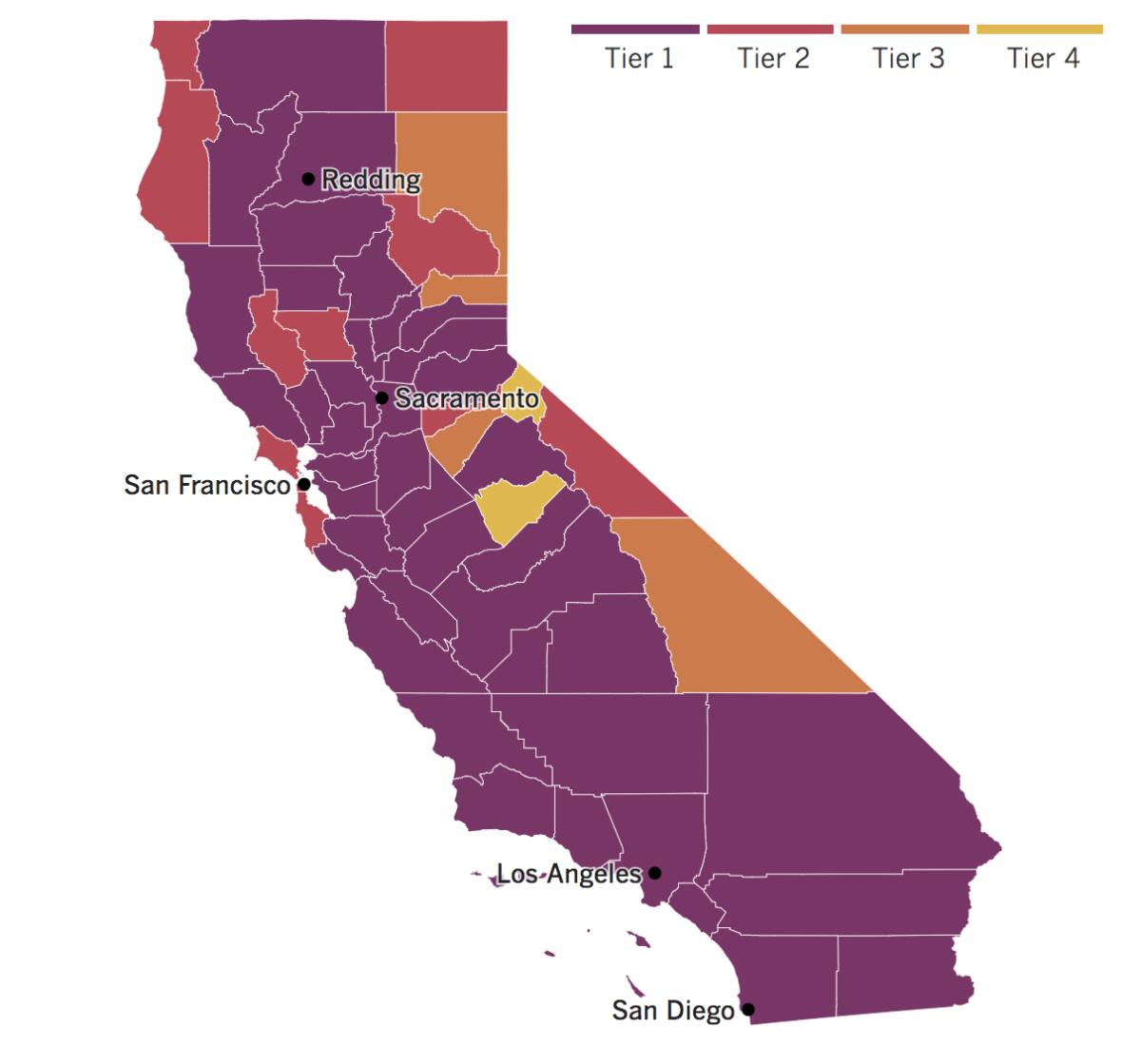
See the current status of California’s reopening, county by county, with our tracker.

Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Across California
Residents and officials in Orange County are not happy about the dramatic rollback of reopenings Newsom ordered this week in his bid to stem the statewide surge in new infections. Nor are they happy now to find themselves among the 94% of Californians living in counties in the strictest, purple tier of the state’s four-tier reopening road map.
Board of Supervisors Chairwoman Michelle Steel, a Republican who was recently elected to Congress, called Newsom’s decision to downgrade Orange County a “unilateral move” that was “troubling and harmful” to Orange County businesses that were forced to limit or suspend their operations.
“Instead of combatting COVID-19 in a thoughtful manner, this one-size-fits-all approach threatens the livelihoods of our residents,” Steel said.
In San Diego, more than 100 elected officials, business owners and residents rallied near the city’s waterfront to demand the county let restaurants, churches and other small businesses reopen. Few of the protesters wore masks, and some waved U.S. flags and posters with slogans like “Save San Diego.”
At the event, county Supervisor Jim Desmond told the crowd it was unfair to punish businesses that follow sanitation protocols, saying the rise in new cases isn’t their fault. “This is not a choice between opening up businesses or saving lives,” Desmond said. “We can do both.”
Los Angeles County, meanwhile, could face a new stay-at-home order if coronavirus cases and hospitalizations continue to surge over the next few weeks. And starting Friday, authorities will order restaurants to close at 10 p.m. and cap the number of people allowed at outdoor gatherings at 15 people, from no more than three households.
The county has been hit particularly hard by the latest wave in the outbreak. The average number of daily cases has tripled in the last month, from more than 900 cases per day to more than 2,800, according to a Times analysis. Hospitalizations have surged nearly 60% in the last month, and the test positivity rate has shot from 3.8% to 5.3% in just the last week.
“This is a different kind of moment, a new level of danger,” Los Angeles Mayor Eric Garcetti said. “If we don’t make these decisions now, there really is only one outcome: We will almost certainly have to shut things down again. And more people will get sick and die.”
While public health leaders are urging Californians to stay away from public gatherings, some of the state’s political leaders are having a hard time following their own government’s guidance. In addition to Newsom’s now-notorious meal at the French Laundry, several members of the state Legislature have been lambasted for taking a trip to Hawaii while mingling with interest groups who may have picked up some of the tab for the event.
These revelations have turned into cannon fodder for those who reject social distancing guidelines. Orange County residents who showed up at Tuesday’s weekly Board of Supervisors meeting lashed out at what they called the hypocrisy of “King Gavin,” whose claim that the birthday dinner was an outdoor event appeared at odds with photos from it.
COVID-19 “magnifies the bad optics” of Newsom’s decision — particularly when people are sacrificing so much, said Kevin Eckery, a public affairs strategist. Nonetheless, the public is likely to accept the governor’s apology and move on.
“We like it when people in authority admit they made mistakes,” he said.
No word yet on whether the same sentiment will hold for the delegation in Hawaii, some of whom remain unwilling to come forward.
Resources
— For general safety, wash your hands for at least 20 seconds (here’s a super-fun how-to video). Stop touching your face, and keep your phone clean. Practice social distancing, maintaining a six-foot radius of personal space in public. And wear a mask if you leave home. Here’s how to do it right.
— Watch for symptoms including fever, cough, shortness of breath, chills, repeated shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. If you’re worried you might be infected, call your doctor or urgent care clinic before going there.
— Need a COVID-19 test? Here’s how to receive a free test if you’re in L.A. County. And here’s a map of testing sites across California.
— Here’s how to care for someone with COVID-19, from monitoring their symptoms to preventing the virus’ spread.
— If your job has been affected by the pandemic, here’s how to file for unemployment.
— Here are some free resources for restaurant workers and entertainment industry professionals having trouble making ends meet.
— Advice for helping kids navigate pandemic life includes being honest about uncertainties, acknowledging their feelings and sticking to a routine. Here’s guidance from the CDC.
— In need of mental health services? Here are resources for coping during the crisis from the CDC and the L.A. County Department of Mental Health. L.A. County residents can also call (800) 854-7771 or text “LA” to 741741.
— For domestic violence victims, the pandemic can pose a “worst-case scenario,” advocates say. If you or someone you know is experiencing such abuse, call the National Domestic Violence Hotline at 1-800-799-SAFE (7233) or L.A. County’s hotline at 1-800-978-3600. Here are more ways to get help.
Around the nation and the world
As the death toll in the U.S. passed 250,000, conditions inside American hospitals are fast deteriorating. Overrun hospitals are now being forced to turn chapels, cafeterias, waiting rooms, hallways and even a parking garage into patient treatment areas. Staff members are calling other medical centers in search of open beds for the nearly 77,000 people requiring treatment across the country.
Front-line workers are suffering from exhaustion and frustration, and for good reason. The number of people hospitalized with COVID-19 in the U.S. has doubled in the last month, with new records set every day this week. Newly confirmed daily infections have risen by more than 80% over the last two weeks, to about 160,000 — the highest levels on record. Cases are rising in all 50 states, and deaths are averaging more than 1,155 a day, higher than they’ve been in months.
“We are depressed, disheartened and tired to the bone,” said Alison Johnson, director of critical care at a Tennessee hospital. Some days, she said, she drives to and from work in tears.
The situation looks a little different across the Atlantic. Though Europe made up close to half of the world’s 4 million new coronavirus cases last week, infections there dropped nearly 10% compared with the week before. That’s thanks in part to strict — though often unpopular — government lockdown measures, according to the World Health Organization.
Still, the tally of COVID-19 deaths rose “substantially” in Europe over the last week, to more than 29,000, the U.N. agency said. (COVID-19 deaths are typically a lagging indicator of the virus’ spread.) Britain has become the region’s first nation to record more than 50,000 deaths.
Meanwhile, the WHO reported that the Americas saw a 41% increase in new cases, which means that a higher weekly death toll could soon be coming. The only region that saw a drop in both cases and deaths was South Asia.
There’s a little more good news on the vaccine front: Pfizer said Wednesday that new test results show its experimental COVID-19 vaccine is 95% effective, has no serious side effects and protects older people who are most at risk of dying of the disease — providing the last bit of data needed for the company to seek the Food and Drug Administration‘s authorization for emergency use.
The announcement comes days after competitor Moderna said its COVID-19 vaccine candidate appears to be 95% effective, based on an interim analysis of its late-stage study.
On Tuesday, the FDA granted emergency use authorization to a rapid coronavirus test that can be performed and developed entirely at home, the only such test out of nearly 300 authorized to date. Users will have to use a swab to collect a nasal sample, then swirl it in a vial that plugs into a portable device that gives a readout. The 30-minute test kit will require a prescription, which is likely to limit its initial use.
Your questions answered
Today’s question comes from a reader who wants to know: What’s the evidence that masks help reduce transmission?
This question comes from someone who says he regularly wears a mask but wants to know a little more about the scientific basis for doing so. So let’s turn to the federal Centers for Disease Control and Prevention, which recently updated its guidance on masks with new evidence on the subject.
To be clear, the CDC says you should wear a mask — that has not changed. But previously, the agency said the reason to do so was to protect other people from your germs. Mask-wearing is caring, the theory went. But new research shows that a mask also offers protection to the person who wears it.
“Now we’re saying here’s another reason” to do it, said Dr. John Brooks, chief medical officer for the CDC’s COVID-19 emergency response.
Federal health authorities cited a Japanese-led study that used mannequin heads and artificial respirators to mimic the spread of coronavirus particles through the air in order to test how well masks blocked transmission.
The results confirmed previous research that masks are most effective when worn by an infected person who might spread the virus by coughing, sneezing or talking. Indeed, masks block about 60% of the virus that comes out of an infected person, the study found.
But on top of that, the scientists also determined that if an uninfected person were standing near an unmasked infected person, the amount of virus inhaled by the uninfected person would fall by 37% if they wore a mask. When both people wore masks, transmission dropped by a whopping 70%.
Our reporters covering the coronavirus outbreak want to hear from you. Email us your questions, and we’ll do our best to answer them. You can find more answers in our Frequently Asked Questions roundup and in our reopening tracker.
For the most up-to-date coronavirus coverage from The Times over the weekend, visit our homepage and our Health section, sign up for our breaking news alerts, and follow us on Twitter and on Instagram.




