Coronavirus Today: A glimmer of hope
Good evening. I’m Amina Khan, and it’s Monday, Nov. 9. Here’s what’s happening with the coronavirus in California and beyond.
In his first address to the nation since declaring victory this weekend, President-elect Joe Biden delivered a clear message to Americans on Monday: “Please, I implore you: Wear a mask.”
Biden’s call for the country to step up and mask up fell short of a call for a nationwide mandate — something that may be beyond the federal government’s authority — but it marked a sharp turn from the rhetoric of President Trump, who has repeatedly disparaged face coverings as a means of preventing the coronavirus’s spread.
“It doesn’t matter your party, your point of view,” Biden said in his speech. “We can save tens of thousands of lives if everyone would just wear a mask for the next few months.”
That would be quite an about-face for masks, which have become a political symbol as much as a preventive health accessory. Democrats largely have adopted and supported mask-wearing and other protective measures meant to impede community spread of the virus, while many Republicans have resisted mask mandates as affronts to personal freedom. But Biden said it was time to stop looking at masks through a partisan lens.
“A mask is not a political statement, but it is a good way to start pulling the country together,” Biden said in his remarks Monday. “I want to be very clear: The goal of mask wearing is not to make your life less comfortable or to take something away from you. It’s to give something back to all of us. A normal life.”
Biden also announced a 13-member advisory board to guide his transition team’s COVID-19 planning. The board will be led by three prominent advisors: Dr. David Kessler, a former commissioner of the Food and Drug Administration; Dr. Vivek Murthy, a former U.S. surgeon general; and Dr. Marcella Nunez-Smith of Yale University, whose research is focused on promoting health equity for marginalized communities. Many board members played significant roles in the last two Democratic administrations.
Dr. Ashish Jha, dean of the Brown University School of Public Health, praised Biden’s task force, calling it the “A-team.” “There is a light at the end of the tunnel,” he said on Twitter.
Biden’s announcement came just hours after pharmaceutical giant Pfizer announced that early data on the COVID-19 vaccine candidate it’s developing with German partner BioNTech suggest that the vaccine is 90% effective — a sign that the company is on track to file an emergency-use application with U.S. regulators.
Keep in mind, this doesn’t mean you’ll be running to your local drugstore or doctor’s office to get the shot any time soon (although you should be getting a flu shot as soon as you can to avoid clogging up hospitals in the “twindemic,” editorial writer Mariel Garza reminds us). The 90% efficacy figure comes from an interim analysis by an independent data monitoring board that looked at 94 infections in a study that enrolled nearly 44,000 people. Pfizer doesn’t plan to stop the study until it records 164 infections among the volunteers — a number the FDA agrees is enough to tell how well the vaccine is working.
Authorities have said it’s unlikely that any vaccine will arrive much before year’s end at the earliest, and that the limited initial supplies will be distributed to those who most need it, such as first responders who face a high risk of on-the-job exposure.
Still, good news is good news. Dr. Anthony Fauci, the government’s top infectious-disease expert, called the vaccine candidate’s effectiveness “just extraordinary,” adding: “Not very many people expected it would be as high as that.”
So, there you are: a glimmer of hope in the fight against this virus. Goodness knows we need it.
By the numbers
California cases and deaths as of 7:04 p.m. PST Monday:
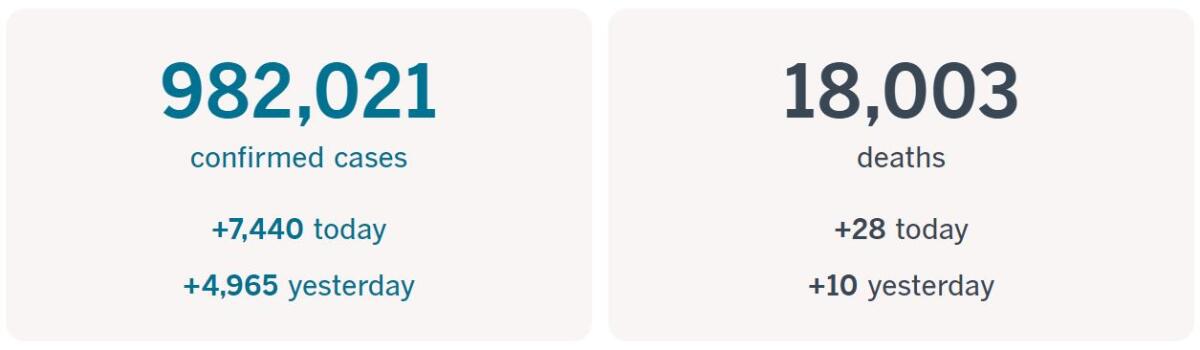
Track the latest numbers and how they break down in California with our graphics.
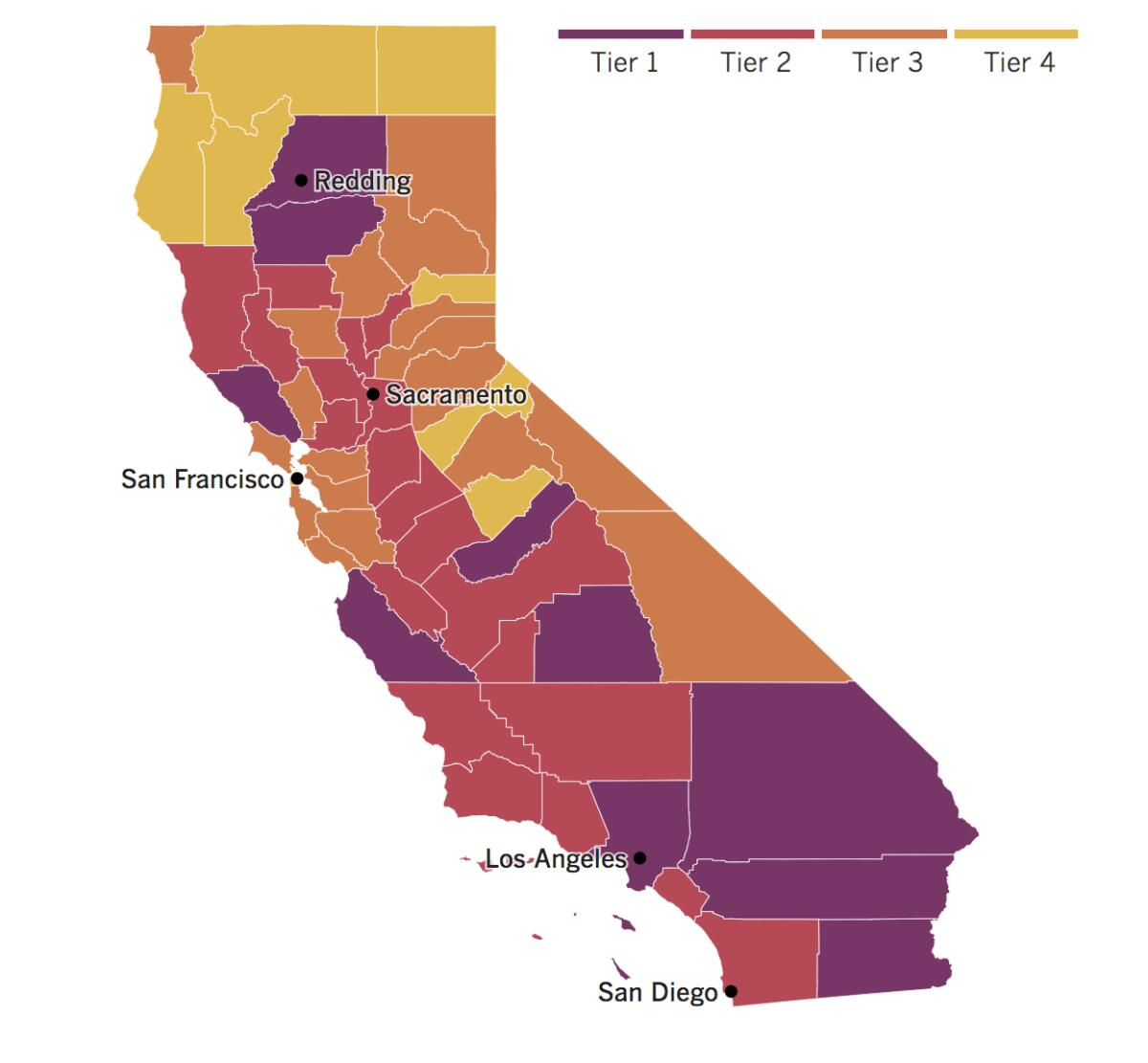
See the current status of California’s reopening, county by county, with our tracker.

Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Across California
For weeks, Los Angeles County health officials have reported ominous spikes in coronavirus cases that they’ve blamed on social gatherings. There were get-togethers with friends where people let their guard down. There were playoff watch parties for the Lakers and Dodgers, and celebrations when they won their championships. There were Halloween festivities.
Now days with more than 2,000 new cases have become commonplace, and county Public Health Director Barbara Ferrer said it’s time to face facts: We’re in the midst of a surge. “This isn’t a blip any longer. This isn’t, ‘Oh, you know, we had one bad weekend. And, you know, we’re now getting back under control,’ ” she said Monday. “This is now a surge in our cases. And if it continues, it will be quite alarming to go into our coldest months seeing this level of increase in cases.”
The increase in cases still isn’t as steep as it was in July, but L.A. County residents should redouble their efforts to prevent the virus from spreading further, she said. That includes refraining from joining crowds in the street to rejoice over the outcome of the 2020 presidential election — something that happened in Los Angeles and around the country.
“Let us remember that no matter how we feel, we all have an obligation to protect each other from COVID-19,” Ferrer said. “Gathering with people outside of your household, especially in settings where people are shouting, chanting or singing and not distancing, can easily lead to increased cases of COVID-19. This will slow down our recovery and can result in more illness and deaths.”
Officials on Sunday announced more than 2,200 new COVID-19 cases, marking the fourth consecutive day with more than 2,000 confirmed infections. The county reported at least 1,413 new cases on Monday, but Ferrer said numbers typically come in lower at the start of the week because of reporting lags over the weekend.
Still, California has a fighting chance to prevent a full-fledged third wave as the winter season closes in. Although the state’s slow-moving reopening strategy has made many residents impatient, health experts say it has kept California’s hospitals from being overwhelmed with COVID-19 patients.
“We are fortunate in the sense that we have a much more muted uptick that’s beginning to occur,” said Dr. Robert Kim-Farley, an epidemiologist and infectious diseases expert at the UCLA Fielding School of Public Health. “And I think it’s because we are still adhering, for the most part, to this tiered approach of gradual opening of the economy and schools.”
That’s going to require a lot of good social-distancing behavior on the part of Californians, even as holiday gatherings might tempt us into risky situations. (Check out the reader question in this newsletter for some tips for politely declining invites to family holiday dinners if you’re looking for the right words.)
Dr. Mark Ghaly, who heads the California Health and Human Services Agency, said the state has benefited from high compliance with a mandatory mask order, which he called “one of the most valuable tools at play to reduce transmission.” By contrast, some of the states seeing the worst per capita case rates have residents who largely are not wearing masks.
UC San Diego is trying to make in-person schooling a less risky enterprise for its students by erecting four large outdoor tents near the center of campus. At 80 feet by 60 feet, the outdoor classrooms will be able to accommodate up to 50 students, a fraction of the capacity of indoor lecture halls, where 200-student classes are held — but they will feature WiFi, podcasting equipment, microphones and LCD display screens. Thanks to a combination of social distancing and the breeze, this setup should provide students a place to study and attend lectures while reducing the risk of transmission.
It’s all part of “Return to Learn,” UCSD’s attempt to allow a relatively small number of students to live on campus and take some courses in person. Campus officials say they may start using the tents this fall, but regular use for lectures won’t start until the winter quarter begins in January. (They’re designed to withstand significant rain and wind.)
UCSD’s enrollment has jumped by 840 during the pandemic, an increase in sharp contrast to other universities around the nation. Since Oct. 1, 72 students and university staff have tested positive for the coronavirus — a relatively small number for a school with 40,473 students.
Resources
— For general safety, wash your hands for at least 20 seconds (here’s a super-fun how-to video). Stop touching your face, and keep your phone clean. Practice social distancing, maintaining a six-foot radius of personal space in public. And wear a mask if you leave home. Here’s how to do it right.
— Watch for symptoms including fever, cough, shortness of breath, chills, repeated shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. If you’re worried you might be infected, call your doctor or urgent care clinic before going there.
— Need a COVID-19 test? Here’s how to receive a free test if you’re in L.A. County. And here’s a map of testing sites across California.
— Here’s how to care for someone with COVID-19, from monitoring their symptoms to preventing the virus’ spread.
— If your job has been affected by the pandemic, here’s how to file for unemployment.
— Here are some free resources for restaurant workers and entertainment industry professionals having trouble making ends meet.
— Advice for helping kids navigate pandemic life includes being honest about uncertainties, acknowledging their feelings and sticking to a routine. Here’s guidance from the CDC.
— In need of mental health services? Here are resources for coping during the crisis from the CDC and the L.A. County Department of Mental Health. L.A. County residents can also call (800) 854-7771 or text “LA” to 741741.
— For domestic violence victims, the pandemic can pose a “worst-case scenario,” advocates say. If you or someone you know is experiencing such abuse, call the National Domestic Violence Hotline at (800) 799-SAFE (7233) or L.A. County’s hotline at (800) 978-3600. Here are more ways to get help.
Around the nation and the world
As President-elect Biden laid out his plans for confronting the pandemic once he takes office Jan. 20, the Trump administration has seen more key staffers become infected with the virus. Housing and Urban Development Secretary Ben Carson has tested positive for the coronavirus, officials said Monday; he is the first member of Trump’s Cabinet to do so.
Late last week, senior administration officials confirmed that White House Chief of Staff Mark Meadows had tested positive, though they offered no details on when he contracted the virus or what his condition was. Meadows had traveled with Trump in the run-up to election day and last appeared in public Wednesday morning — without a mask — as Trump falsely declared victory while the votes were still being counted.
Meadows and Carson are among the 10 million Americans who have contracted the virus since the pandemic began. One million new infections were recorded in the last 10 days, a drastic uptick as the country faces its third major surge.
By Monday morning, total deaths had surpassed 237,000. The Centers for Disease Control and Prevention said it expected that figure to grow by about 20,000 over the next two weeks. “We’re seeing the equivalent of two 747s crashing per day, killing everybody onboard,” said Dr. Carlos del Rio, a global health epidemiologist at Emory University, expressing concern that the public had not grasped the scale of devastation.
“You’d imagine, at some point, someone would say, ‘What’s going on with planes?’” he said. “There would be outrage. And I’m not seeing the outrage.”
Not all areas of the country are being hit the same way at the same time. The Dakotas are among the states with the lowest population density, but they’re suffering from the nation’s worst fatality rate per capita over the last 30 days. North Dakota reported 309 COVID-19 deaths in the last 30 days, causing its rate to shoot up to 41 deaths per 100,000 people, data from Johns Hopkins shows. South Dakota has reported 252 deaths in the last 30 days, and a death rate of about 29 people per 100,000 during that time.
Experts worry that deaths will continue their upward climb in the northern Plains and Upper Midwest, given that people have been slow to wear masks and adopt other mitigation measures. In the name of limited government, both states’ Republican governors have denigrated government orders to help halt the outbreaks.
Doctors in the region say they’re stunned that they are still struggling to persuade people to take precautions. “When I go out and I don’t see a significant number of people masking, that really worries me,” said Dr. Jawad Nazir, a clinical professor at the University of South Dakota School of Medicine. “This is not going away.”
In Utah, Gov. Gary Herbert declared a state of emergency and ordered a statewide mask mandate in an effort to stem a surge in hospitalizations. Residents are required to wear face coverings in public, at work and when they are within six feet of people who don’t live in their households. The order will remain in effect until Nov. 23.
Several of the largest counties in the state already require masks, but Herbert had avoided extending the rule to the entire state despite a two-month surge in cases. On Sunday, the Republican governor said the time to debate masks had passed and that his orders would not shut down the economy.
U.S. regulators have allowed emergency use of the first antibody drug to help the immune system fight COVID-19. The Food and Drug Administration on Monday cleared the experimental drug for people 12 and older with mild or moderate cases who do not require hospitalization. The one-time treatment is given through an IV. The therapy, from Eli Lilly, is still undergoing testing to establish its safety and effectiveness. It is similar to a treatment Trump received after contracting the virus last month.
Your questions answered
Today’s question comes from a reader who wants to know: How safe is it to stay in hotels and motels right now — particularly those where you have to walk through a shared hallway to get to your room?
This is a tricky question to answer, as there aren’t a whole lot of clear numbers to guide risk, experts say. Travelers seem to be erring on the side of caution by increasingly checking into open-corridor motels, according to a story by my colleague Roger Vincent. Perhaps they feel safer entering their rooms directly from the open air instead of passing through a closed corridor with shared, circulated air.
That said, I spoke to Dr. Natascha Tuznik, an infectious disease expert at UC Davis, for some insight into how to evaluate the risk.
“Hotels and motels do confer risk, as does any travel,” Tuznik said. But if you do have to stay somewhere, an Airbnb or VRBO rental might be better for a few reasons.
First, many hosts are following enhanced cleaning guidelines based on protocols from the CDC and the World Health Organization.
Second, with Airbnb or VRBO rentals, there is less stranger foot traffic to worry about, and you may be less likely to encounter crowded elevators or hallways.
Third, rental properties can typically be aired out better thanks to multiple windows and doors. And many hosts are leaving time — sometimes days — between guest occupancies, reducing the chances that you’ll pick up the virus from someone who was in the space before you. (Tuznik still recommends re-cleaning all high-touch surfaces and placing the TV remote in a resealable plastic bag, because they’re really just impossible to clean.)
That said, “environmental (surface) transmission accounts for a minority of cases, maybe 5% or so at most,” she added. “It really is the respiratory route that confers the greatest risk.”
While motels with outdoor corridors may indeed have potentially lower risk than closed-corridor motels, the risk inside the rooms remain the same, she said. That risk depends on the efficacy of the airflow and venting system in the room, and older buildings with older systems may not be as good as more up-to-date, state-of-the-art facilities, she added.
Tuznik offers these tips if you find yourself checking in somewhere overnight:
- Call ahead and ask what enhanced measures or protocols are being implemented. “If the answer is unknown or wishy-washy, I would see this as a red flag,” she said. “Businesses should want to be transparent.”
- Re-clean high touch surfaces, as mentioned.
- Forgo the maid service or cleaning service so fewer people enter your room.
- Don’t walk around barefoot — wear shoes or flip flops.
- Strip the comforter off the bed (it’s oftentimes not laundered, she says) as well as any decorative pillows.
- Put the remote in a clear plastic bag.
- Air out the room when you arrive, if possible.
Our reporters covering the coronavirus outbreak want to hear from you. Email us your questions, and we’ll do our best to answer them. You can find more answers in our Frequently Asked Questions roundup and in our reopening tracker.
For the most up-to-date coronavirus coverage from The Times over the weekend, visit our homepage and our Health section, sign up for our breaking news alerts, and follow us on Twitter and on Instagram.




