Op-Ed: I nearly died from COVID. Now I’m letting go of the fear

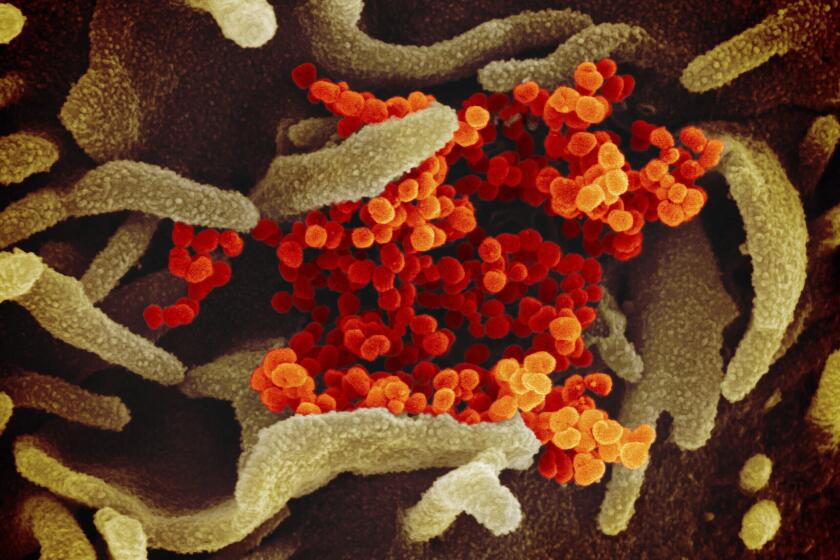
Two years ago, I was in a hospital bed on the 15th floor of NYU Langone hospital in Manhattan, dying of COVID-19. A previously healthy, 44-year-old runner, I found myself impossibly weak, unable to walk five feet from my bed to the bathroom without a nurse’s help. I could barely breathe, even with the highest levels of supplemental oxygen. Eventually I wound up in the ICU, where I was placed on a ventilator.
Trying to shake our nation into taking the threat seriously, I shared my coronavirus ordeal with the world. I tweeted about it from the hospital; talked about it on the “Today” show, “The Rachel Maddow Show,” and “Nightline”; and wrote for multiple publications about my time on the ventilator, my painfully slow recovery, and my six-figure hospital bills (which I thankfully did not have to pay). I hoped that my story led others to do everything humanly possible to prevent contagion.
Today, COVID-19 is far less dangerous than it was two years ago, and I wonder: By telling my harrowing story, did I contribute to a climate of fear that we now find difficult to dispel?
Op-Ed: As a doctor in a COVID unit, I’m running out of compassion for the unvaccinated. Get the shot
A doctor featured in a Times article published Sunday on the latest wave of COVID-19 speaks for herself in a searing letter to unvaccinated people.
Amazing vaccines have made illness much less severe. The currently dominant Omicron variant is relatively mild. Treatments, including antiviral pills, monoclonal antibodies and steroids, are much more effective than what was available to me. As a result, the death rate among hospitalized patients has plummeted. In April 2020, when I left the hospital, more than 23% of patients who went to the hospital for COVID wound up dying there. By September 2021, only 2.8% died in the hospital. Practically speaking, COVID today and COVID in the spring of 2020 are vastly different.
Meanwhile, two years of mitigation measures have taken a serious toll: increased deaths from non-COVID causes, record numbers of fatal drug overdoses, an economic crisis for our cities, and a mental-health crisis that has hit young people particularly hard. The pandemic’s effects have been especially harmful in education, with low-income and minority students suffering the most.
Two years ago, the president declared a state of emergency to deal with the emerging threat of COVID-19. Now is the right time for authorities to begin the necessary examination of our state and national response to the novel coronavirus.
So despite my own nightmarish experience, I’m glad to see that states, counties and school districts are modifying pandemic requirements. I’m glad to see that office leasing is on the rise again, and major corporations are bringing their workers back to the office. I’m glad to see that other nations are lifting contagion precautions and easing travel restrictions.
We should celebrate these developments — especially because even as they’re happening, COVID cases and deaths are down dramatically from their peaks in California, the United States and the world (with some notable exceptions, such as China).
The degree of protection against COVID strongly correlates with the strength of our long-lived T-cell response to the coronavirus’ proteins.
As states and countries start to move past the crisis stage of the pandemic, they can look to California’s “SMARTER” plan as a possible blueprint for addressing COVID as a more endemic phenomenon. The plan, an acronym for “shots, masks, awareness, readiness, testing, education and Rx,” acknowledges that while keeping the public safe is important, so is keeping businesses open and keeping students in school. At the same time, the approach contains contingency plans and metrics for when to implement them, in case COVID deaths start rising again — which can’t be ruled out, especially if a more dangerous new variant emerges.
With more than a thousand Americans still dying every day, the virus remains a serious threat. We need to get more people vaccinated and boosted. We need to protect the most vulnerable, including the elderly and the immunocompromised. We need to support healthcare workers suffering from burnout, depression and anxiety. We need to treat people enduring “long COVID,” as I did for more than a year. We need to remember and mourn the almost 1 million Americans, and more than 6 million people worldwide, who have lost their lives to this disease.
Here’s what we don’t need: more fear. Instead, let’s take a deep breath and move from a mindset of fear to a mindset of hope. After two long years, it’s hard to let go of being afraid, but let’s try. If we continue living in a perpetual state of anxiety and emergency, we are defeating only ourselves.
David Lat is the author of Original Jurisdiction, a newsletter about law and the legal profession.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.