Coronavirus could become leading cause of death in L.A. County
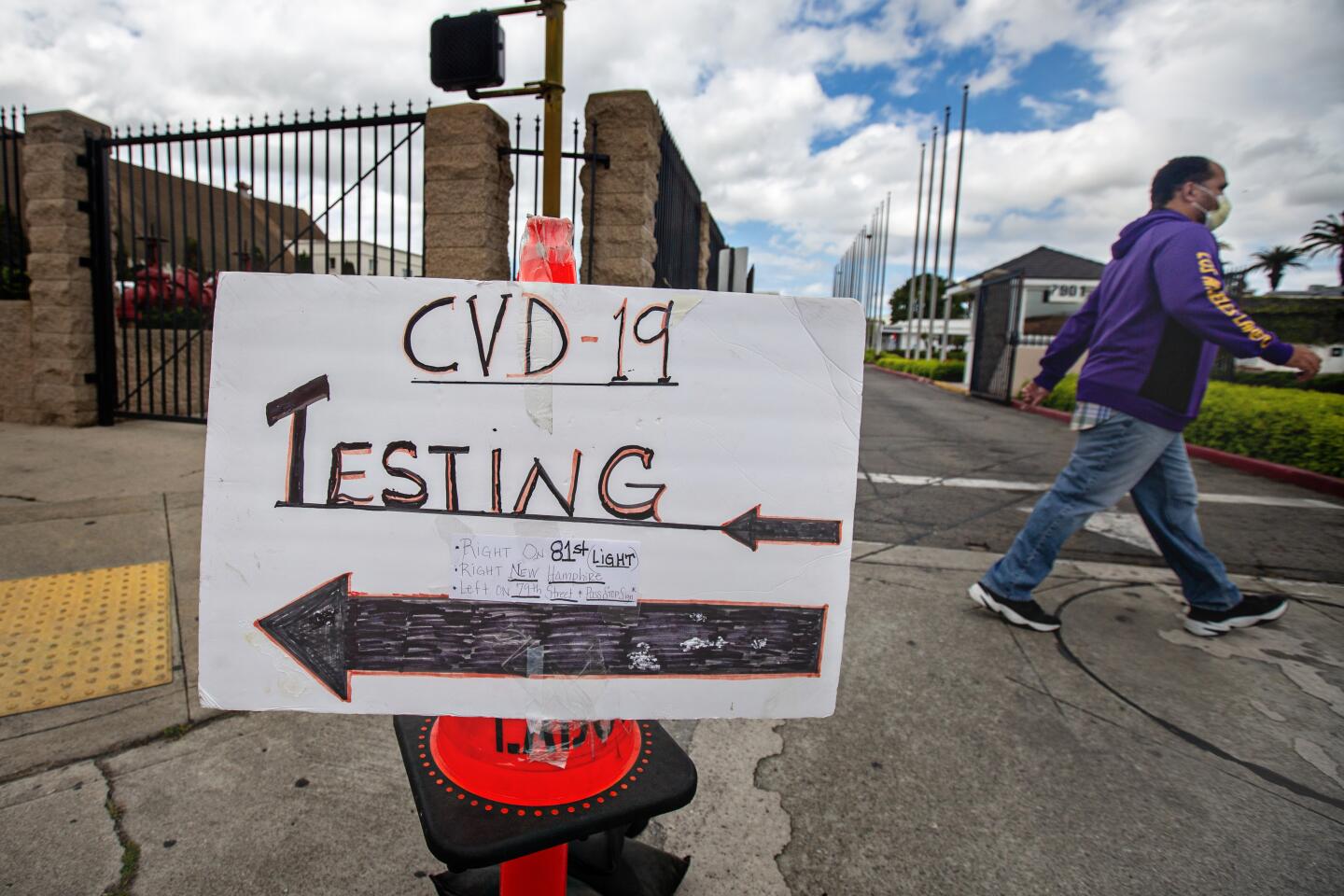
A new report says that perhaps 4% of Los Angeles County residents have been infected with the coronavirus at some point. The research offers both hopeful and sobering news for the county, which has been hit hard by the coronavirus.
It suggests social distancing has slowed the outbreak and that COVID-19 might be less fatal than originally believed. But it is still a killer. More than 600 have lost their lives to the coronavirus, accounting for about half the coronavirus deaths in California — even though L.A. County has only about a quarter of the state’s population.
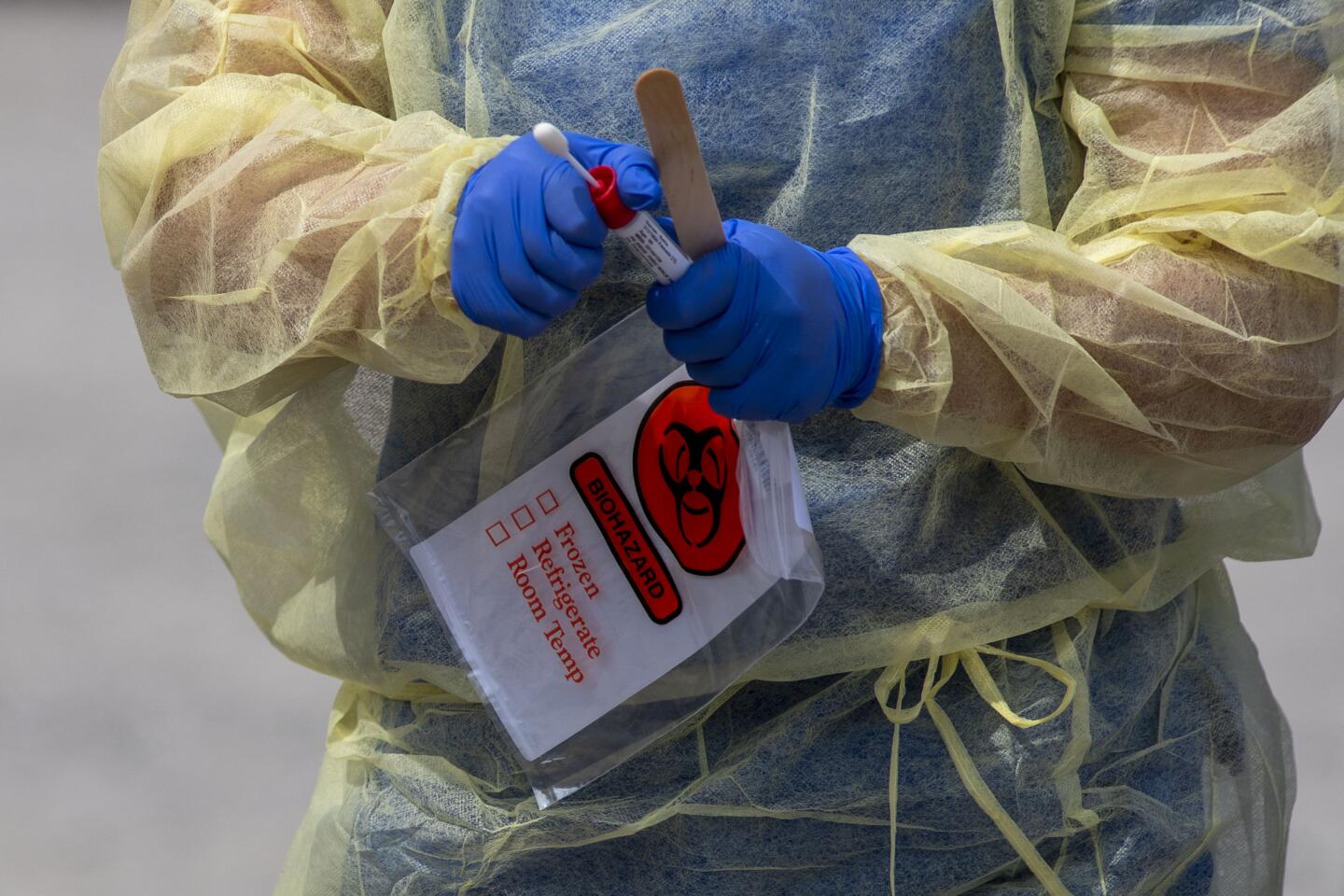
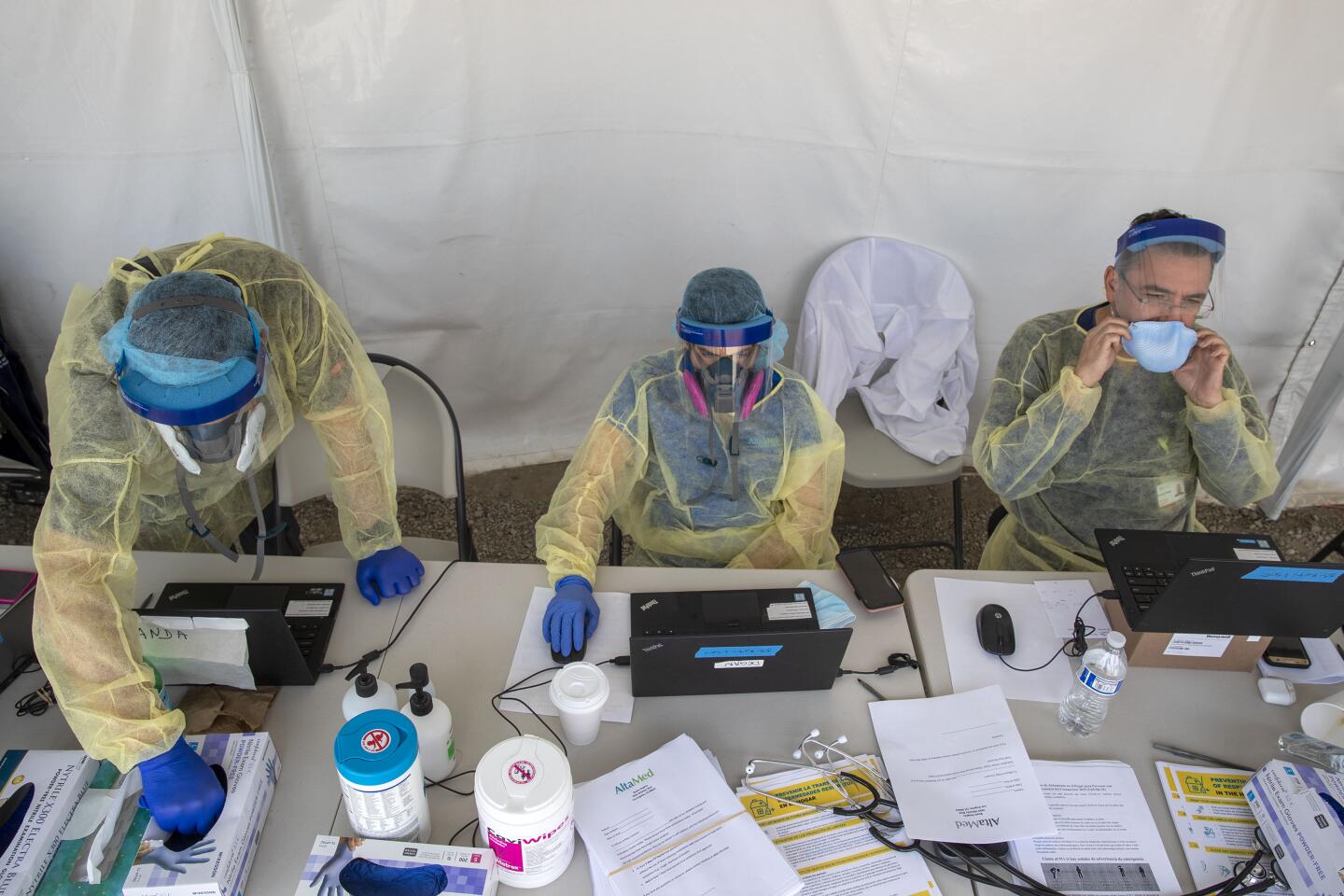
The results come from the first large-scale study tracking the spread of the virus in the county, which is California’s most populous and has the state’s highest numbers of cases and deaths. Researchers identified a pool of 863 adults reflecting the county’s demographics for the study, conducted by USC and the county Department of Public Health.
They found that 2.8% to 5.6% of adults have antibodies to the virus in their blood, an indication of past exposure. Without any adjustments for a margin of error, the raw percentage of people testing positive for past exposure to the coronavirus in L.A. County was about 4.1%.
Three Angelenos describe getting the highly coveted blood test for coronavirus antibodies.
What are the implications of this report?
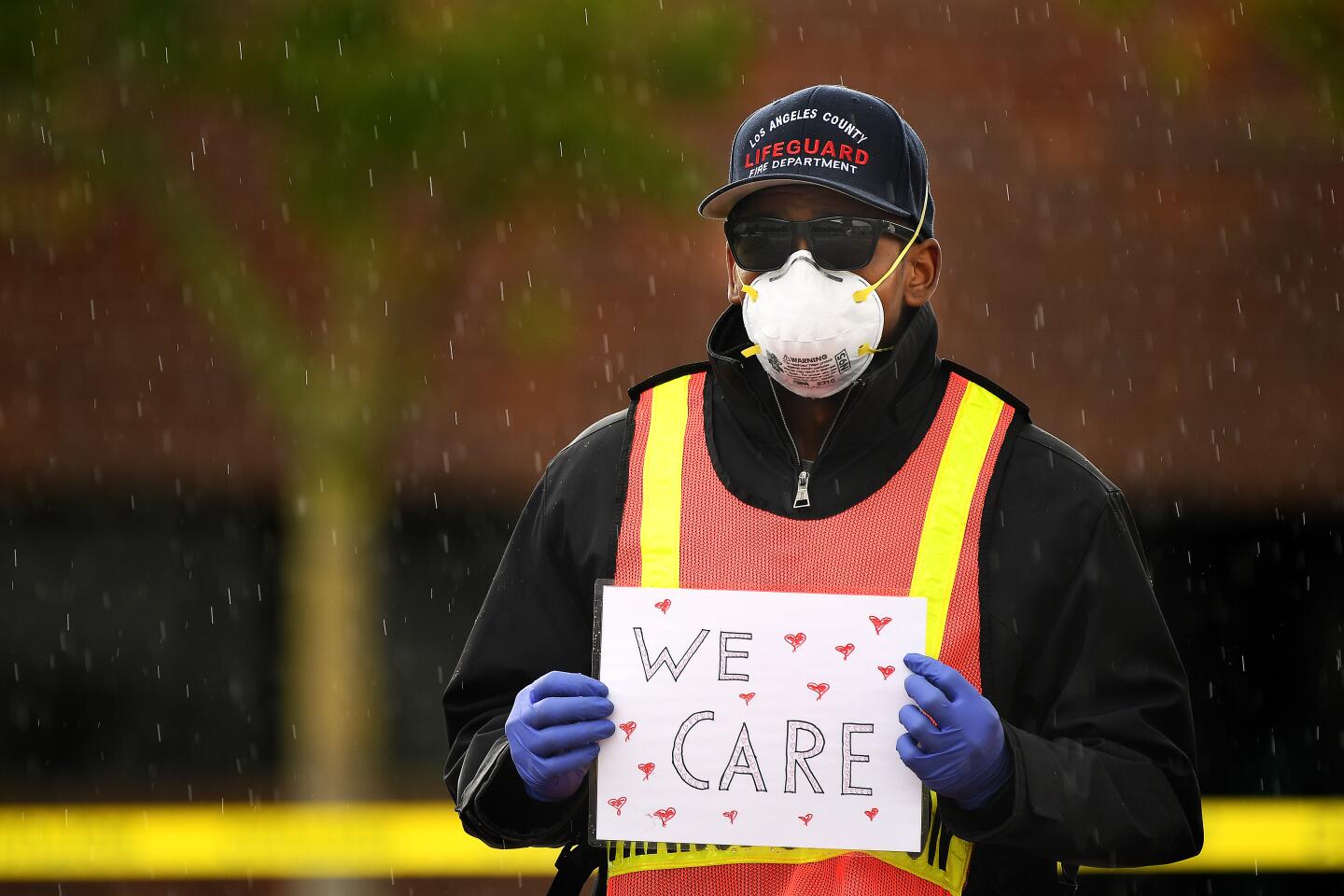
It could mean that L.A. County has done a great job of slowing the spread of the coronavirus, said Barbara Ferrer, director of the L.A. County Department of Public Health. The virus’ escalation came while the county pursued stay-at-home orders that have prevented hospitals from being overwhelmed with too many critically ill patients.
In other words, it means that roughly 221,000 to 442,000 adults have recovered from infection as of early April, at a time when the county had officially reported fewer than 8,000 COVID-19 cases.
An early morning text. A lawyer-filled meeting on a Sunday afternoon. Emotional journal entries. And, ultimately, action.
What do the numbers suggest about the case fatality rate of the virus?
It suggests that for those infected with the virus in L.A. County, 0.1% to 0.2% died, Ferrer said. That would put it similar to the case fatality rate for the seasonal flu, which is 0.1%.
Study leader Neeraj Sood, a professor at USC‘s Price School for Public Policy, cautioned that Ferrer’s calculation was a preliminary estimate.
“This is kind of like a back-of-the-envelope calculation that Dr. Ferrer did,” Sood said.
It’s also a percentage specific only to Los Angeles County. Italy and New York might have different case fatality rates.
“There could be underlying differences in the health of the population,” Sood said. Also, the case fatality rate can change in the course of an epidemic. When hospitals start to be stretched beyond capacity, and there’s a shortage of doctors or medical equipment, the case fatality rate can suddenly change and get worse.
Unlike in most other developed countries, drug companies in the United States are allowed to charge whatever they want for prescription medicine, often basing price on the “benefit” to patients.
Does this mean the coronavirus is only as bad as the flu?
No. As can be seen, Ferrer said, the coronavirus is extraordinarily devastating and can cause more death in a much shorter amount of time, compared with the seasonal flu.
The case fatality rate is not the only thing important when considering the catastrophic impact of a pandemic. Also important: the number of people who get infected.
“If the number of people who get infected is, say, three times of that as the flu, even if the fatality rate is the same, you’re going to get thrice as many deaths,” Sood said.
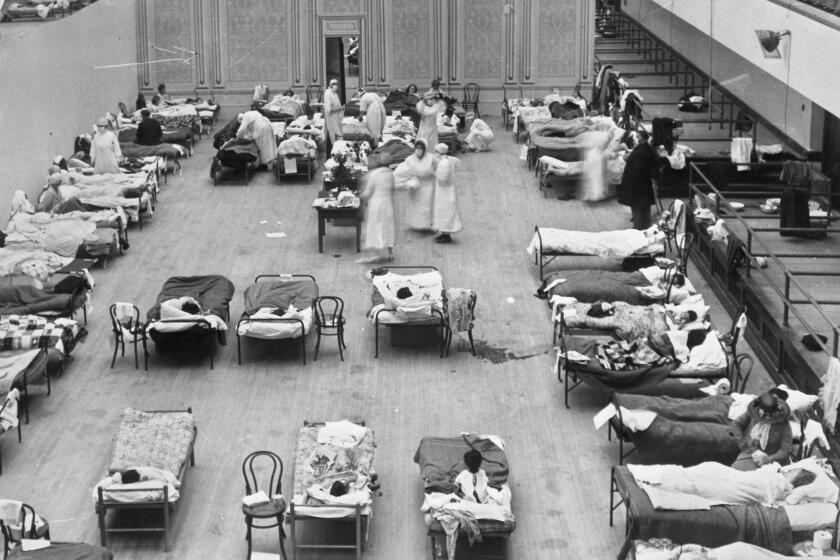
Also, seasonal flu deaths might be spread out over six to eight months. But for COVID-19, the same number of deaths might be concentrated in the span of one or two months, “which could overwhelm the healthcare system. And that in turn might change the fatality rate,” Sood said.
From the Plague of Justinian and the Black Death to polio and AIDS, pandemics have violently reshaped civilization since humans first settled into towns thousands of years ago. No one can know exactly how the COVID-19 pandemic will ultimately change the world. But stress cracks are already showing.
How would the coronavirus compare to other leading causes of death?
The coronavirus may very well become the leading cause of death in L.A. County.
Dr. Paul Simon, chief science officer at the L.A. County Department of Public Health and co-lead on the study, said that, on average, there are 165 deaths daily in Los Angeles County from all causes, with the leading cause coronary heart disease, which claims 35 to 40 lives daily.
“We’re now seeing about 50 deaths a day from COVID,” Simon said. “If this mortality were to continue for the whole year — we hope it doesn’t, but if it did — COVID would be the leading cause of death in Los Angeles County. So we’re still very concerned about mortality.”
Newsom said that while areas across the state have been affected differently by the pandemic, the “virus knows no jurisdiction, knows no boundaries” and could easily spread into neighboring counties if they ease restrictions prematurely.
What are the study’s implications on how soon the stay-at-home order can be lifted?
A second round of the study will be done as a follow-up in two to three weeks, which will be important to see how the virus continues to spread through the county. That study may help determine whether L.A. County remains on track to possibly loosen the stay-at-home order some time in May.
“I think if the prevalence stays relatively stable, that’s reassuring,” Simon said. “If we see a big bump up in prevalence, I think that will be more cause of concern.”
Researchers hope to repeat the study at regular intervals over the course of the summer. Officials will also be looking at multiple sources of data to determine when it’s safe to relax certain physical distancing orders, Simon said.
The study authors did not release an underlying technical report that detailed their methodology.
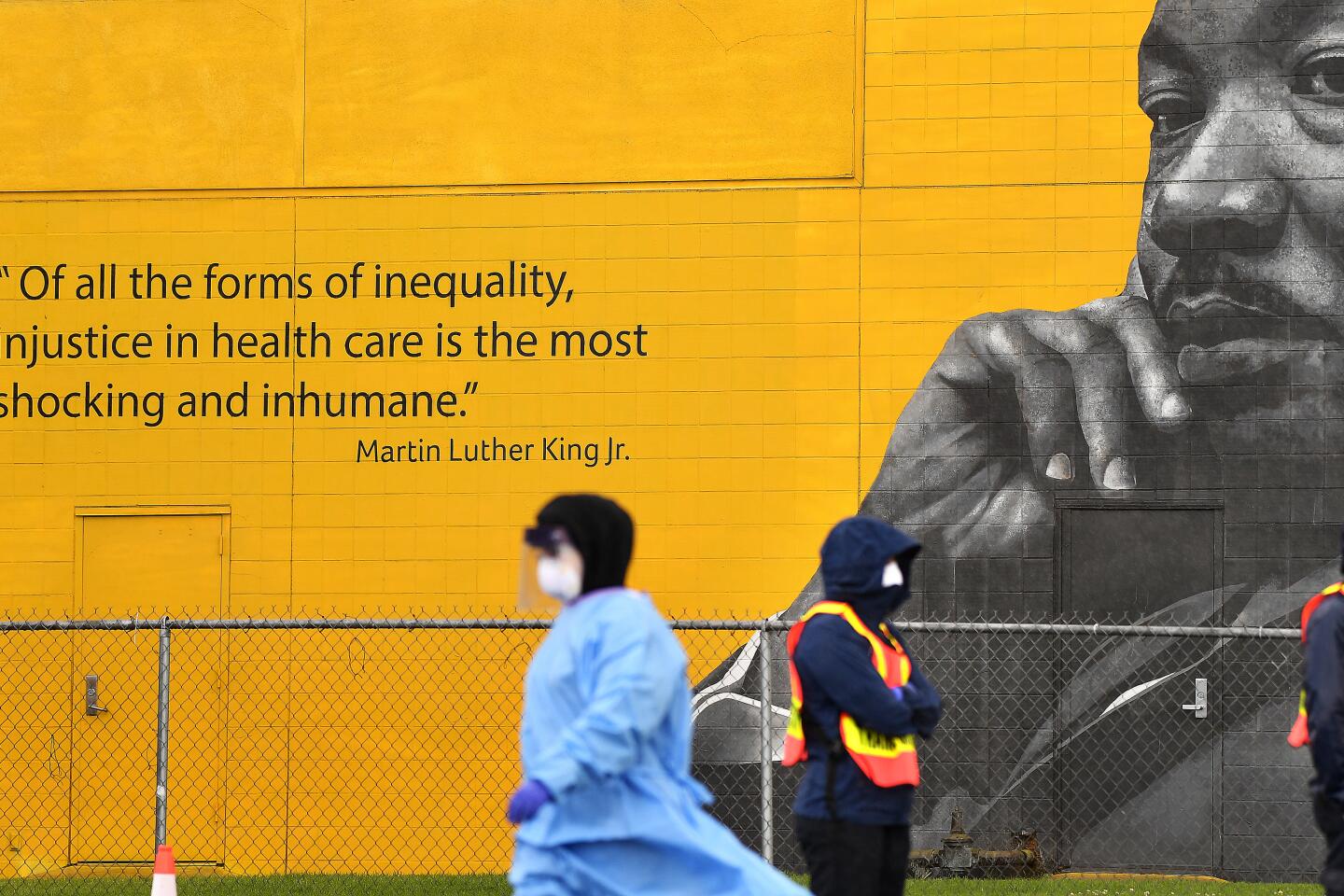
Coronavirus: L.A. releases first racial breakdown of fatalities; African Americans have higher death rate
What are racial and gender breakdowns?
Preliminary data found that men were more likely to be infected than women in L.A. County. Seven percent of blacks in the study tested positive, compared with 6% of white participants, 4% of Asian Americans and 2.5% of Latinos.
“There seem to be some differences by gender, and by race/ethnicity, but we really need to dig deeper into that to figure out,” Sood said. “Is it something about where you live? Is it something about you taking public transportation? Is it something about your biology or some genetic predisposition?”
What does the latest hospitalization data show?
Although there’s been a surge of public optimism that coronavirus cases are not headed toward worst-case scenarios, California has yet to see a sustained decline in the number of people hospitalized or in intensive care for the coronavirus.
The number of people confirmed to have the coronavirus in California and in intensive care has remained between 1,100 and 1,200 from April 6 through Sunday.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.