Hundreds of thousands in L.A. County may have been infected with coronavirus, study finds

Hundreds of thousands of Los Angeles County residents may have been infected with the coronavirus by early April, far outpacing the number of officially confirmed cases, according to a report released Monday.
The initial results from the first large-scale study tracking the spread of the coronavirus in the county found that 4.1% of adults have antibodies to the virus in their blood, an indication of past exposure.
That translates to roughly 221,000 to 442,000 adults who have recovered from an infection, once margin of error is taken into account, according to the researchers conducting the study. The county had reported fewer than 8,000 cases at that time.
The findings suggest the fatality rate may be much lower than previously thought. But although the virus may be more widespread, the infection rate still falls far short of herd immunity that, absent a vaccine, would be key to return to normal life.
“We are very early in the epidemic, and many more people in L.A. County could potentially be impacted,” said Neeraj Sood, the study’s leader and a professor at USC’s Sol Price School of Public Policy. “And as those number of infections arise, so will the number of deaths, the number of hospitalizations, and the number of ICU admissions.”
The early results from L.A. County come three days after Stanford researchers reported that the coronavirus appears to have circulated much more widely in Santa Clara County than previously thought.
Though the county had reported roughly 1,000 cases in early April, the Stanford researchers estimate the actual number was 48,000 to 81,000.
The findings bolster the sense that a significant portion of those carrying the virus could show no symptoms at all, and therefore be unknowingly infecting others. Dr. Deborah Birx, the coordinator of President Trump’s coronavirus task force, said during the White House briefing that the USC results underscore “concern about asymptomatic spread” because it is harder to trace.
“This has been the fundamental question to begin with,” she said, emphasizing the importance of treating the disease as “highly contagious.”
A new study by Stanford University, using antibody blood tests, estimates that the number of cases in Santa Clara County may be 50 to 85 times greater than what was previously known.
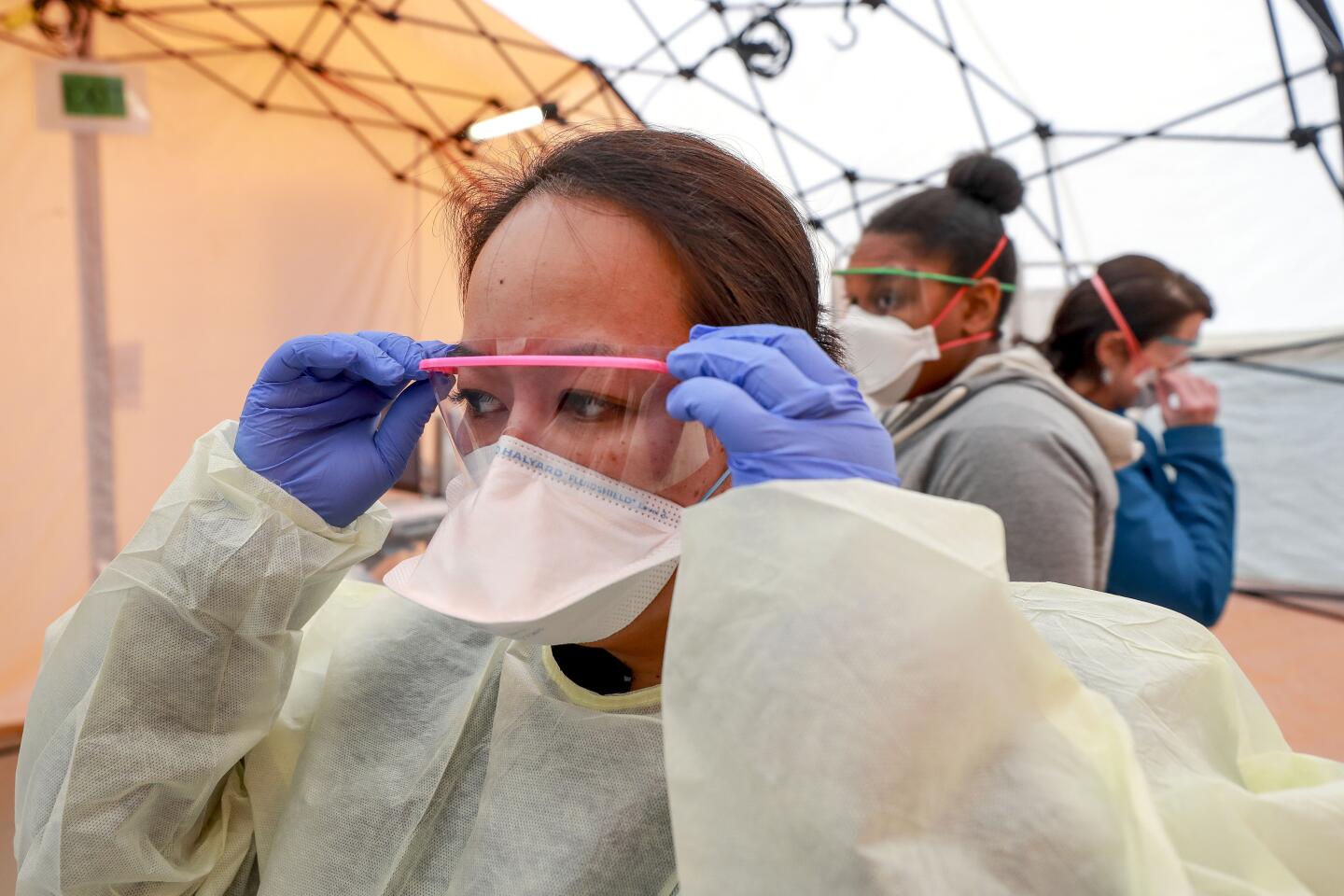
Antibody tests, also known as serology testing, have increasingly become a focal point in the response to coronavirus because they can potentially show the true extent of the virus’ reach and therefore can shed light on how close the population is to achieving herd immunity. That occurs when enough people have some degree of immunity to the virus that it becomes difficult for infections to spread.
“Any way you slice the data ... it’s clear that herd immunity in this situation does not apply. It’s still way below that level,” said Natalie Dean, a professor of biostatistics at the University of Florida.
Such tests can also provide a more accurate picture of how lethal the virus is.
The mortality rate is based on the number of confirmed infections; the higher the number of infections, the lower the fatality rate. Both studies estimated a mortality rate of 0.1% to 0.2%, which is closer to the death rate associated with the seasonal flu.
Researchers emphasized that these initial findings should not make people dismiss the risks of COVID-19.
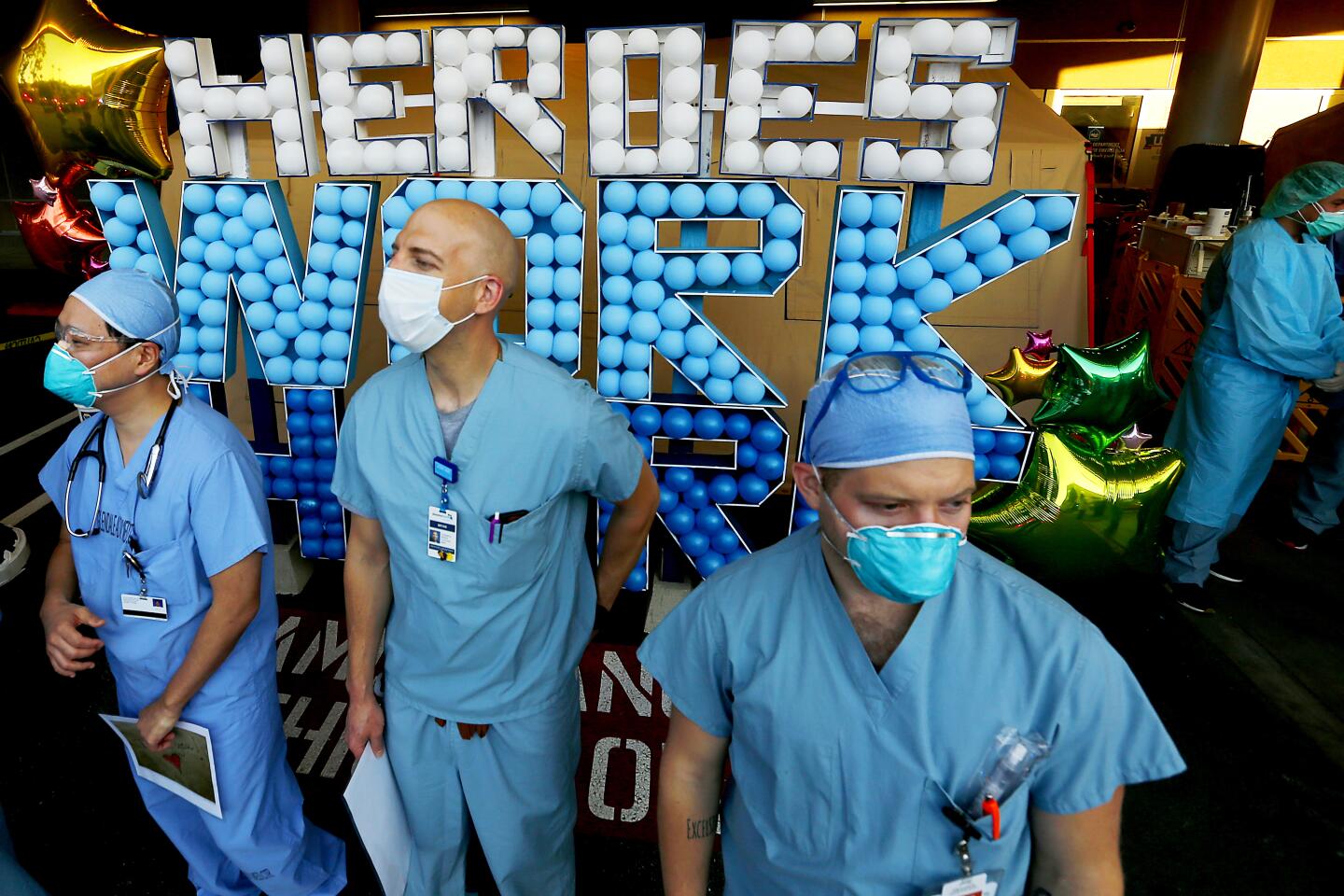
Paul Simon, chief science officer for Los Angeles County’s public health department, noted that the county was averaging 50 deaths from coronavirus a day, eclipsing cardiac disease as the top killer.
“If this mortality were to continue for the whole year — we hope it doesn’t, but if it did — COVID would be the leading cause of death in Los Angeles County,” Simon said.
Preliminary data from Los Angeles found that men were more likely to be infected than women. Seven percent of blacks in the study tested positive, compared with 6% of white participants, 4% of Asian Americans and 2.5% of Latinos.
“There seem to be some differences by gender, and by race/ethnicity, but we really need to dig deeper into that to figure out,” Sood said. “Is it something about where you live? Is it something about you taking public transportation? Is it something about your biology or some genetic predisposition?”
The Santa Clara study recruited around 3,300 participants from social media, which has raised some concerns that the results may not be representative of the county as a whole. The researchers made adjustments to their data to account for that problem.
The study was composed differently in Los Angeles; 863 adults were selected through a market research firm to represent the makeup of the county. The county and USC researchers intend to repeat the study every two to three weeks for several months, in order to track the trajectory of the virus’ spread.
Both counties used rapid antibody tests supplied from Premier Biotech, a Minneapolis-based company. The test has not yet been approved by the FDA, although the federal government does allow for such tests to be used for public health surveillance.
Neither the Stanford nor USC studies have been vetted by the typical peer review process, and their initial conclusions have been fiercely debated. USC researchers did not release an underlying technical report Monday that detailed their methodology.
Dr. Warner Greene, a virologist with Gladstone Institutes in San Francisco, said that research out of Wuhan, China — where the virus is believed to have originated — found that the number of infections was likely 2.5 times higher than originally known. The studies in Los Angeles and Santa Clara, by contrast, said the true case counts were between 28 and 85 times greater than official reports.
“I don’t know where the truth lies yet,” Greene said. “I do know that we knew all along that we were missing a lot of infections. The degree of the miss is what’s in question.”
Eric Topol, a physician and executive vice president of Scripps Research in La Jolla, contrasted the Los Angeles study findings with those from a Wuhan hospital that found an infection rate hovering between 2% to 3%.
“You have to check your serology versus what’s known in the rest of the world, and the 4.1% that they came up with is ... considerably higher than Wuhan,” Topol said. “We are not Wuhan anywhere in California, by any stretch of anyone’s imagination.”
The two studies in California are among the surge of new research underway across the globe attempting to detect the presence of coronavirus antibodies to find cases that may have been missed initially.
“Early data from some of these studies suggest that a relatively small percentage of the population may have been infected, even in heavily affected areas — not more than 2% to 3%,” said Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization.
Collecting and analyzing real-time data on the number of cases and deaths during a disease outbreak is crucial. Here’s why we’ve failed.
As antibody testing has risen in prominence and are increasingly available on the commercial market, so too have concerns about accuracy over the results, particularly the occurrence of false positives, which could inflate estimate of infection rates.
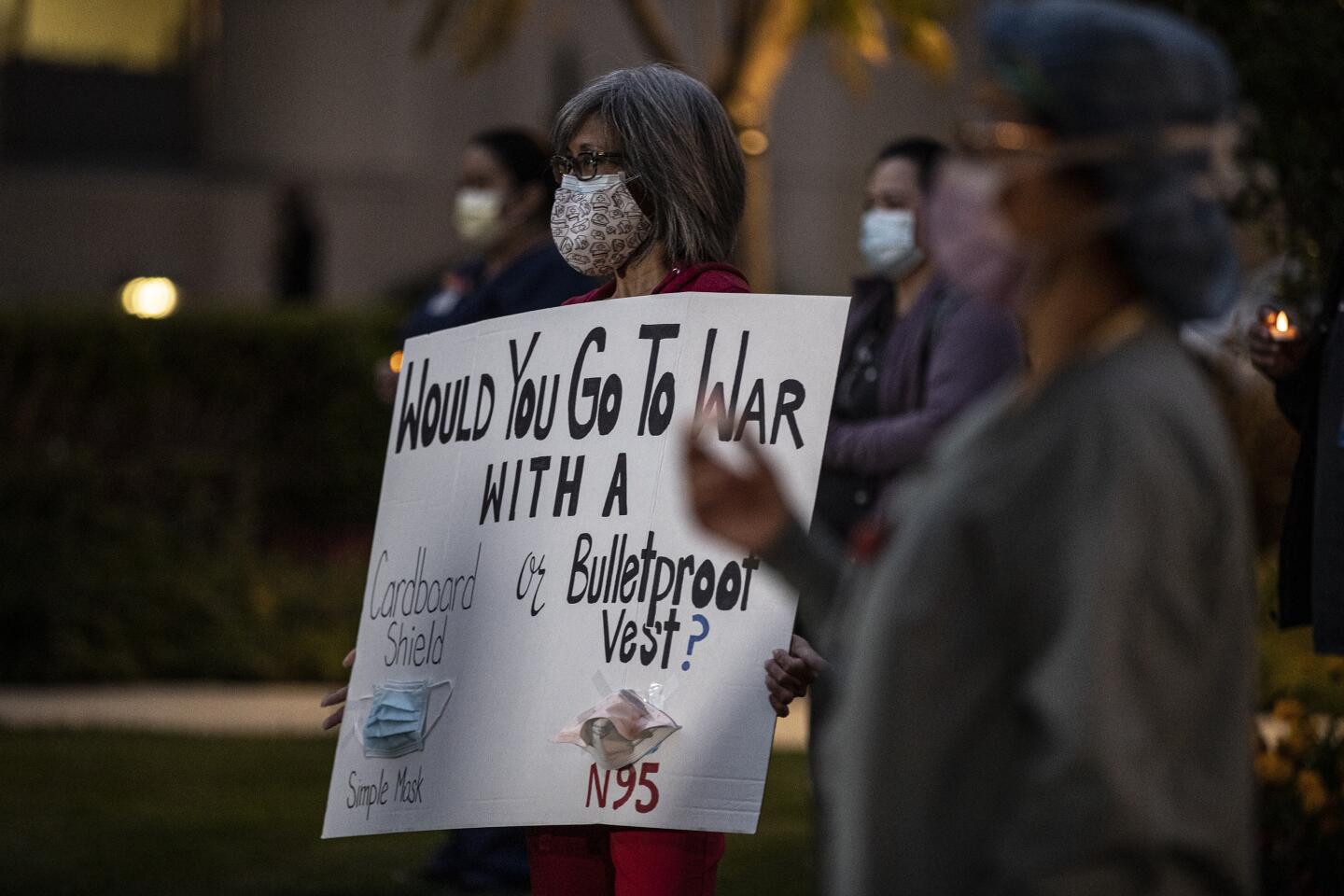
It is unlikely the initial findings will cause county officials to immediately change their response to the virus. Barbara Ferrer, the county’s top health official, said that the high rate of infection only underscored the need to continue with physical distancing, wearing cloth face coverings and staying home if sick.
“We need to assume that at any point in time, we could be infected and that all of the other people we come in contact with could also be infected,” Ferrer said Monday.
Ferrer also took pains to note that much is still unknown about whether the presence of antibodies to this virus means a person is immune.
“Being positive for COVID-19 antibodies does not mean that a person is immune, or that a person is not able to be reinfected,” Ferrer said. “More research is really needed to understand what protections people have who may have already been infected with COVID-19.”
Times staff writers Deborah Netburn, Emily Baumgaertner and Noah Bierman contributed to this report.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.