The world could wipe out malaria. A new report shows why that isn’t happening
Despite progress toward preventing the spread of malaria, the world is moving too slowly toward elimination of the disease, which still claims hundreds of thousands of lives each year, the World Health Organization said Tuesday.
On the positive side, children and pregnant women in sub-Saharan Africa have greater access to tools that stop the transmission of malaria, according to the annual World Malaria Report. Diagnostic testing for children and preventive treatment for pregnant women has risen steeply across the region over the last five years, and the use of nets treated with insecticide has expanded rapidly.
But overall progress toward eliminating the spread of the disease is threatened by “substantial gaps” in the number of people with access to those measures, and the fragile health systems that exist in many countries, the international health agency said.
In addition, “For the last five years, global funding for malaria has flat-lined,” Pedro Alonso, director of WHO’s global malaria program, told reporters in a telephone briefing. “If this flat line remains, we shall not be able to achieve the ambitious goals and targets that the world has agreed upon.”
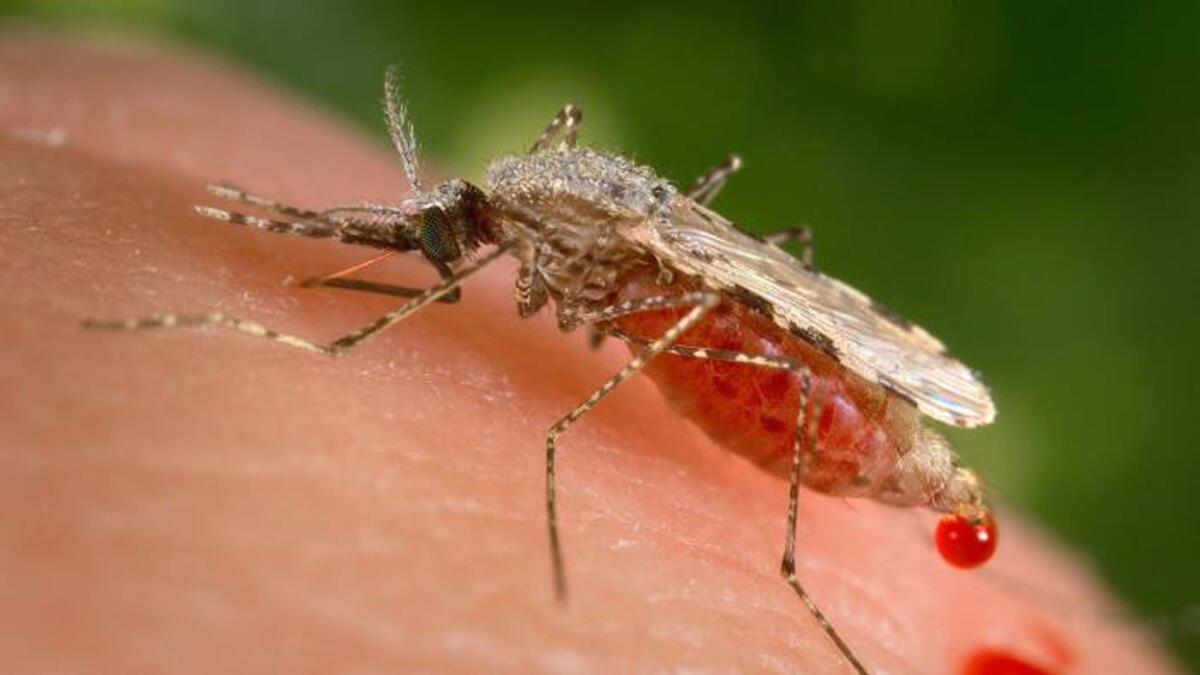
Malaria, which is primarily found in sub-Saharan African and South Asia, is spread to humans by the bites of infected female mosquitoes. It causes flu-like symptoms that can lead to severe complications and death.
The international community has a target of eliminating the disease in at least 10 countries by 2020, and to reduce the number of cases and deaths globally by at least 40% by that date. Eighteen Asian countries have set a goal of eliminating malaria by 2030.
But in 2015, there were 212 million new cases of malaria and 429,000 deaths worldwide, according to the report, which tracks data on progress and trends in 91 countries and areas where malaria occurs.
Notable gains marred by shortfalls
In 2015, around half of children with a fever who sought care at a public health facility in 22 African countries received a diagnostic test for malaria, enabling providers to quickly detect the disease and prescribe life-saving treatment, nearly double the number in 2010, according to the report. And last year in 20 African nations there was a five-fold increase in the percentage of women receiving the recommended three or more doses of preventive treatment in pregnancy, the report said.
Other regions, including Southeast Asia, the Western Pacific and the Americas, also saw progress. Of 91 countries and territories with malaria transmission in 2015, 39 are estimated to have achieved a reduction of 40% or more in mortality rates between 2010 and 2015. And globally, malaria mortality rates are estimated to have declined by roughly two-thirds between 2000 and 2015. A further 10 countries saw no deaths from malaria in 2015.
“Those are significant achievements,” said Richard Cibulskis, coordinator of the global malaria program’s strategy, evidence and economics unit at WHO. “We are, however, off track to reduce malaria incidents and mortalities by 40% by 2020.”
Progress has lagged in countries with a high number of malaria cases and death, Cibulskis said.
“What really needs to happen is to accelerate progress in those countries,” he said.
Despite the gains in sub-Saharan Africa, for example, the region recorded roughly 90% of last year’s new malaria cases and deaths. In addition, children under the age of 5 accounted for an estimated 70% of all malaria deaths, and the disease “remains a major killer of under-5s,” the report said.
Lack of protection still an issue
One reason for the continued transmission of malaria is the lack of protection against infected mosquitoes.
Consistent use of bed nets can reduce malaria transmissions by as much as 90%, according to Nothing But Nets, a global grassroots campaign to raise awareness and funding to fight malaria.

“Bed nets are the most cost-effective proven tool to prevent against malaria,” said Margaret Reilly McDonnell, campaign director for the group, which operates in 30 countries across sub-Saharan Africa. “There are other vector control programs but bed nets have given us the biggest bang for the buck in terms of prevention.”
It costs around $10 to buy a net, deliver it and educate a family about its use, said McDonnell, whose group expects to deliver 10 million nets by the end of 2016.
Still, more bed nets are needed. According to WHO, a fifth of households in sub-Saharan Africa did not have access to bed nets in 2015. And fewer than half the households had sufficient insecticide-treated nets.
According to WHO, an estimated 43% of the population in sub-Saharan Africa was not protected by treated nets or by insecticides sprayed indoors in 2015.
In many countries, health systems are short on money and are hard to reach for those most at risk of malaria, and that has also contributed to the death toll from the disease, according to the WHO.
Need for a super drug
Advocates for a malaria-free world are calling for new tests and medicines that would help eradicate the disease.
Martin Edlund, chief executive officer of the Seattle-based advocacy group Malaria No More, underscored the need for better diagnostic testing that can detect the parasite even in people who show no symptoms of malaria. WHO recommends diagnostic testing for all people with suspected malaria before treatment is administered.
“We need a generation of malaria drugs that can eliminate all stages of the parasite in the human body, so you can take one course of treatment and eliminate all the parasites “ Edlund said. “And we need to stay ahead of the development of drug resistance, which we’re seeing in Southeast Asia.”
Mosquito resistance to insecticides and antimalarial drugs are a growing concern, WHO officials said. For example, since 2010, 60 of the 73 countries that monitor insecticide resistance have reported mosquito resistance to at least one type of insecticide used in nets and indoor sprays, according to the report.

Last month, the WHO announced that the world’s first malaria vaccine would be rolled out through pilot projects in three countries in sub-Saharan Africa in 2018.
If the vaccine trial is a success, the drug would be widely distributed, officials said.
Funding failure
WHO officials said a lack of funds for malaria control posed “a serious challenge” to combating the disease.
In 2015, malaria funding totaled $ 2.9 billion, just under half the annual target set for 2020. The United States is the largest international funder, accounting for about a third of donations.
“We know we have very cost-effective malaria interventions,” said Cibulskis. “We know that when we apply them at scale we do reduce malaria significantly.”
Alonso warned against the world becoming complacent because of the many gains in fighting malaria.
“The sense that the job has been completed and therefore we move on, that’s a very dangerous one,” he said. “The fight against malaria is a success story. However, we still have in excess of 400,000 deaths. So we are far from having completed the job.”
For more on global development news, see our Global Development Watch page, and follow me @AMSimmons1 on Twitter
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.











