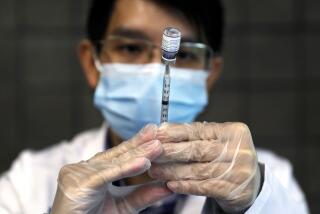
CDC finds the unvaccinated are 11 times more likely to die of COVID

New U.S. studies released Friday show the COVID-19 vaccines remained highly effective against hospitalizations and death even as the extra-contagious Delta variant swept the country.
One study tracked more than 600,000 COVID-19 cases in 13 states from April through mid-July. As Delta surged in early summer, those who were unvaccinated were 4.5 times more likely than the fully vaccinated to get infected, more than 10 times more likely to be hospitalized and 11 times more likely to die, according to the Centers for Disease Control and Prevention.
“Vaccination works,” Dr. Rochelle Walensky, CDC’s director, said at a White House briefing Friday. “The bottom line is this: We have the scientific tools we need to turn the corner on this pandemic.”
But as earlier data have shown, protection against coronavirus infection is slipping some: It was 91% in the spring but 78% in June and July, the study found.
So-called “breakthrough” cases in the fully vaccinated accounted for 14% of hospitalizations and 16% of deaths in June and July, about twice the percentage as earlier in the year.
An increase in those percentages isn’t surprising: No vaccine is perfect, and health experts have warned that as more Americans get vaccinated, they naturally will account for a greater fraction of the cases.
Op-Ed: As a doctor in a COVID unit, I’m running out of compassion for the unvaccinated. Get the shot
A doctor featured in a Times article published Sunday on the latest wave of COVID-19 speaks for herself in a searing letter to unvaccinated people.
Walensky said Friday that well over 90% of people in U.S. hospitals with COVID-19 are unvaccinated.
The CDC released two other studies Friday that signaled hints of waning protection for older adults. One examined COVID-19 hospitalizations in nine states over the summer and found protection for those 75 and older was 76% compared with 89% for all other adults. And in five Veterans Affairs medical centers, protection against COVID-19 hospitalizations was 95% among 18- to 64-year-olds compared with 80% among those 65 and older.
It isn’t clear if the changes seen over time are because immunity is waning in people first vaccinated many months ago, that the vaccine isn’t quite as strong against Delta — or that much of the country abandoned masks and other precautions just as Delta started spreading.
But U.S. health authorities will consider these latest real-world findings as they decide whether at least some Americans need a booster, and how soon after their last dose. Next week, advisors to the Food and Drug Administration will publicly debate Pfizer’s application to offer a third shot.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.