Corinne Purtill is a science and medicine reporter for the Los Angeles Times. Her writing on science and human behavior has appeared in the New Yorker, the New York Times, Time Magazine, the BBC, Quartz and elsewhere. Before joining The Times, she worked as the senior London correspondent for GlobalPost (now PRI) and as a reporter and assignment editor at the Cambodia Daily in Phnom Penh. She is a native of Southern California and a graduate of Stanford University.
1
In November 2017, days after her daughter Mallory Smith died from a drug-resistant infection at the age of 25, Diane Shader Smith typed a password into Mallory’s laptop.
At this point, keeping myself alive is a full-fledged mission, enlisting all of my energy and hours every day. I need to fight the chronic deadly resistant bacteria eating away at my fragile, scarred lungs. Fight the billions of bacteria overtaking my lungs and clear out the mucus so I don’t feel like I’m breathing through a straw with a boulder weighing on my chest.
— Mallory Smith, Oct. 16, 2014
Her daughter gave it to her before undergoing double-lung transplant surgery, with instructions to share any writing that could help others if she didn’t survive.
Had this idea today that I wanted to write down before it leaves my mind or I stop feeling inspired or I forget it or something inside me tells me it’s not possible. I want to start an online media source (podcast? website?) that tells the stories of people who have struggled with something in their life and found hope somewhere.
— Mallory Smith, July 20, 2015
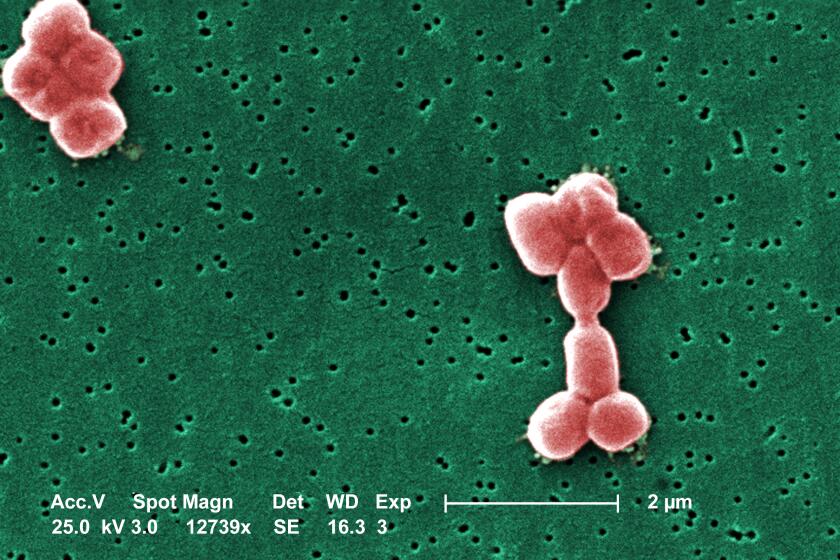
The transplant was successful, but Burkholderia cepacia — an antibiotic-resistant bacterial strain that first colonized her system when she was 12 — took hold. After a lifetime with cystic fibrosis, and 13 years battling an unconquerable infection, Mallory’s body could take no more.
Cepacia has taken over, and it’s time to figure out a transplant option. I realize I want to write my story.
— Mallory Smith, July 29, 2016
In the haze of grief and pain, Shader Smith found herself looking through 2,500 pages of a journal her daughter had kept since high school. It chronicled Mallory’s hopes and triumphs as an ebullient, athletic student at Beverly Hills High School and Stanford University, and her private despair as bacteria ravaged her systems and sapped her considerable strength.
In the years since, the journal has become a source of solace for Shader Smith as she has traveled the globe speaking about the growing threat of antimicrobial resistance. It is also now the inspiration for two new projects she hopes will spark greater understanding of the public health crisis that ended her daughter’s life prematurely and could claim millions more.
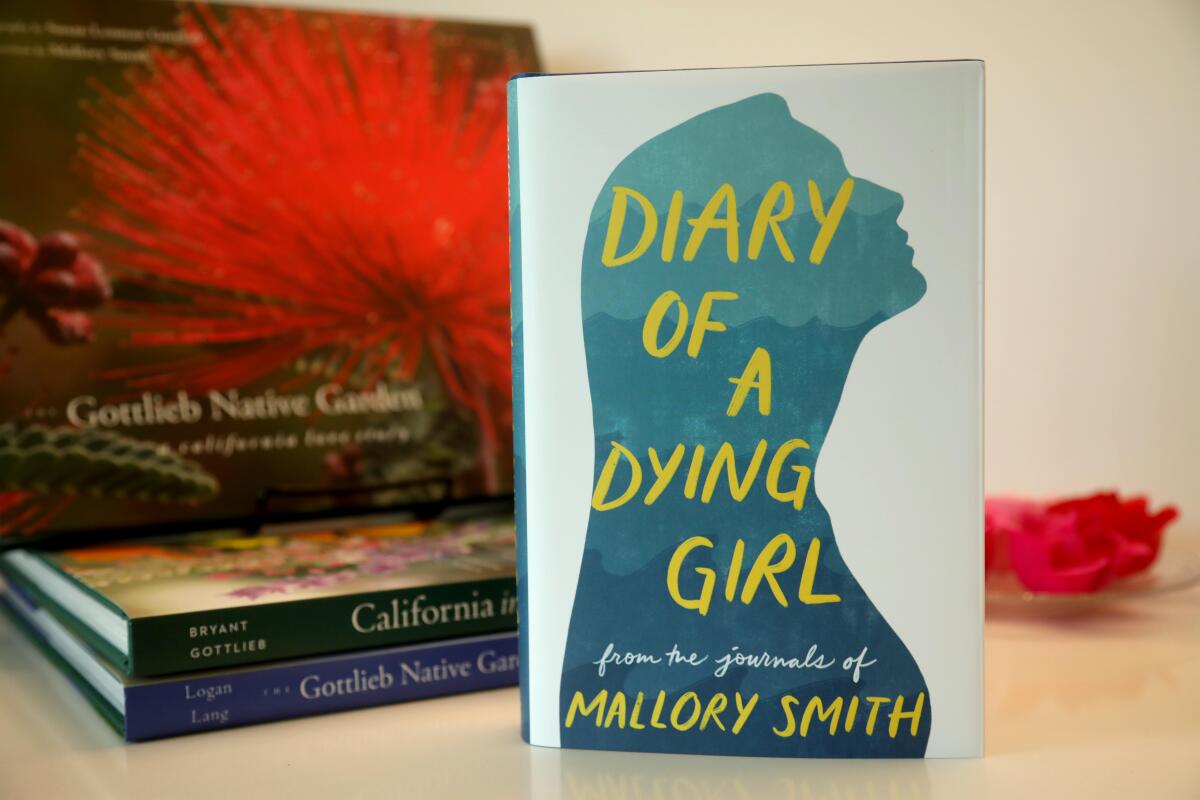
“Diary Of A Dying Girl” excerpts Mallory Smith’s own writings, which chronicle her 13-year battle against an antibiotic-resistant lung infection.
(Genaro Molina / Los Angeles Times)
On Tuesday, Random House published “Diary of a Dying Girl,” a selection of Mallory’s journal entries. The same day saw the launch of the Global AMR Diary, a website collecting the worldwide stories of people battling pathogens that can’t be defeated by our current pharmaceutical arsenal.
An estimated 35,000 people die in the U.S. each year from drug-resistant infections, according to the U.S. Centers for Disease Control and Prevention. Worldwide, antimicrobial resistance kills an estimated 1.27 million people directly every year and contributes to the deaths of millions more.
Despite the mounting toll — and the prospect of an eventual surge in superbug fatalities — the development of new antibiotics has stagnated.
Shader Smith is acutely aware of what we stand to lose when medicine can no longer save us.
“I don’t want to live in a post-antibiotic world,” Shader Smith said. “Until people understand what’s at stake, they’re not going to care. My daughter died from this. So I care deeply.”
Over the last 50 years, opportunistic pathogens have evolved defenses faster than humans can develop drugs to combat them.
Misuse of antibiotics has played a large part in this imbalance. Bugs that survive antibiotic exposure pass on their resistant traits, leading to hardier strains.
Crucial as they are, antibiotics don’t have the same financial incentives for developers that other drugs do. They aren’t meant to be taken over the long term, as are medications for chronic conditions such as diabetes or high blood pressure. The most powerful ones have to be used as rarely as possible, to give bacteria fewer opportunities to develop resistances.
“The public does not understand [the] scope of the problem. Antimicrobial resistance truly is one of the leading public health threats of our time,” said Emily Wheeler, director of infectious disease policy at the Biotechnology Innovation Organization. “The pipeline for antibiotics today is already inadequate to address the threats that we know about, without even considering the continuous evolution of these bugs as the years go on.”
Scientists have created a synthetic molecule that appears capable of attacking a broad range of bacteria that have become dangerously resistant to workhorse medicines.
Despite the global nature of the threat, Shader Smith said, the response from public health officials is curiously disjointed.
For one, no one can agree on a single name for the problem, she said. Different agencies address the issue with an “alphabet soup” of acronyms: the World Health Organization uses AMR as shorthand for antimicrobial resistance, while the CDC prefers AR. Medical journals, doctors and the media refer alternately to multidrug resistance (MDR), drug-resistant infections (DRI) and superbugs.
“It doesn’t matter what you call it. We just have to all call it the same thing,” said Shader Smith, who works as a publicist and marketing consultant.
Since Mallory’s death, Shader Smith has made it her mission to get the people and organizations working on antimicrobial resistance to talk to one another. For the Global AMR Diary, she enlisted the help of a dozen agencies working on the issue, including the CDC, WHO, the European Center for Disease Prevention and Control (the European Union’s equivalent of the CDC), the Biotechnology Innovation Organization and others.
Antimicrobial resistance can “feel abstract given the scale of the problem,” said John Alter, head of external affairs of the AMR Action Fund, one of the organizations involved with the project. “To know there are millions of families at this very moment going through struggles similar to what Mallory experienced is simply unacceptable,” he said.
“Not only does this firsthand experience help others who might be going through something similar, but it also reminds those tasked with creating solutions and care who they are working for. They aren’t just test tubes or charts,” said Thomas Heymann, chief executive of Sepsis Alliance, another contributor.
For the first time in half a century, researchers have identified a new antibiotic that appears to kill a deadly, drug-resistant superbug.
The stories in the online diary are often harrowing. A 25-year-old pharmacist in Athens had to put her cancer treatment on hold when an extremely resistant strain of Klebsiella attacked. A veterinarian in Kenya suffered permanent disability after contracting resistant bacteria after hip surgery. Around the world, routine outpatient procedures and illnesses have rapidly become life-threatening when opportunistic bugs take hold.
Mallory was 12 when her doctor called to confirm that her cultures were positive for an extremely resistant strain of cepacia, a form of bacteria found widely in soil and water. The pathogen can be deadly to people with underlying conditions such as cystic fibrosis, a genetic disorder that impairs the cells’ ability to effectively flush mucus from the lungs and other body systems.
Life expectancies for people with cystic fibrosis have grown since Mallory’s diagnosis in 1995, with many people of them living into their 40s and beyond. The cepacia curtailed that possibility for her.
“This is all we’re ever going to have,” Mallory wrote in June 2011, at the end of her freshman year at Stanford, “so if you’re not actively pursuing happiness then you’re insane. And I don’t think I would have this perspective if I didn’t have resistant bacteria that will likely kill me.”

A shrine to Mallory Smith. She fought a drug-resistant bacteria from age 12 to 25, all through high school, then at Stanford. (Genaro Molina / Los Angeles Times)
Mallory’s intuition that her journal could be valuable to others was prescient. “People can easily understand and relate to actual experiences,” said Michael Craig, director of the CDC’s Antimicrobial Resistance Coordination and Strategy Unit. “The Global AMR Diary takes this approach and expands on it with a global lens — increasing the potential to get these critical messages to more people around the world.”
An earlier version of Mallory’s diaries was published in 2019 as “Salt in My Soul: An Unfinished Life.” The new book includes entries that Shader Smith said she wasn’t ready to grapple with in the immediate aftermath of Mallory’s passing: ones addressing depression and private despair, concerns about relationships and body image issues complicated by chronic illness.
It also includes a coda about phage therapy, a promising advance against AMR.
As cepacia overwhelmed Mallory’s system in the weeks after her transplant, her family secured an experimental dose of phage therapy. Widely used to treat infection before the advent of antibiotics, phages are viruses that destroy specific bacteria. The treatment arrived too late to save Mallory’s life, Shader Smith writes in a last chapter of the book, but her autopsy revealed that the phages had started to work as intended.
The systems that bring new drugs to patients move slowly, Shader Smith said, and “Mallory might have been saved if they had moved faster.” Her mission now is to make sure that they do.
“Mallory died six years ago. Six years is a long time, day in and day out,” she said. “And I’ve never taken my foot off the pedal.”
Ozempic and other drugs raised the possibility of reversing the country’s obesity crisis. Doctors are frustrated that they’ve made health disparities worse.