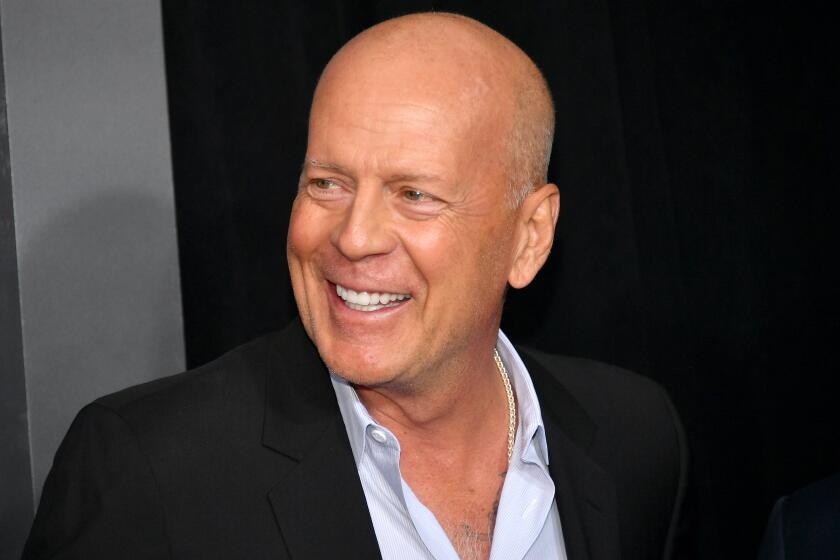
What is frontotemporal dementia? The disease afflicting actor Bruce Willis is incurable

On Wednesday, the family of actor Bruce Willis disclosed that he has been diagnosed with frontotemporal dementia, a degenerative brain disease that currently has no cure.
Calling the diagnosis a “cruel disease,” Willis’ wife, Emma Heming Willis, ex-wife Demi Moore and daughters Rumer, Scout, Tallulah, Mabel and Evelyn posted their statement on the website of the Assn. for Frontotemporal Degeneration, an advocacy group for patients and their families.
“We know in our hearts that — if he could today — he would want to respond by bringing global attention and a connectedness with those who are also dealing with this debilitating disease,” they wrote.
An estimated 50,000 people in the U.S. live with frontotemporal dementia, said Dr. William Seeley, a neurologist at UC San Francisco who in 2011 was awarded a MacArthur Foundation “genius” grant for his work on the condition he described as a “complex and heterogeneous disease that’s difficult to diagnose.”
What is frontotemporal dementia?
Frontotemporal dementia is a progressive brain disease that affects the frontal and anterior temporal lobes of the brain. It’s the most common form of dementia for people who are diagnosed under the age of 60.
The condition first asserts itself in one of two ways depending on the specific part of the brain in which the disease begins: with major changes to the person’s behavior or to their language ability.
Bruce Willis, who retired from acting last year due to aphasia issues, has been diagnosed with frontotemporal dementia, his family said Thursday.
Just over half of patients are diagnosed with behavioral-variant frontotemporal dementia. Because the disease destroys cells in key parts of the brain that coordinate social functioning, patients may become suddenly and uncharacteristically uninhibited, saying and doing things that appear inappropriate or impulsive to those around them.
They often appear apathetic or uninterested in activities, said Dr. Mario F. Mendez, a neurologist and director of the Behavioral Neurology Program at UCLA. Most painfully for their loved ones, they can also seem detached and unempathetic to the feelings of those around them.
The remainder of FTD patients fall into the subcategory of primary progressive aphasia, a broad term for language problems that get progressively worse.
This version of FTD also has two main types. In the non-fluent variant, people may struggle to form sentences that make grammatical sense — or to produce words at all.
Those with the semantic variant are often still able to speak fluently but lose the ability to understand words.
Willis’ family did not disclose details of his frontotemporal diagnosis. They shared his diagnosis of aphasia last year upon announcing his retirement from acting. Many who worked with Willis in the final films he made before going public with his aphasia diagnosis noted changes in the actor’s language and memory.
“Someone would give him a line and he didn’t understand what it meant,” a crew member on the film “White Elephant” told The Times.
What causes frontotemporal dementia?
The answer is the same as it is for other types of dementia: we don’t really know.
“For the typical patient, we really don’t have great ways of predicting who’s at risk or understanding why they got the disease,” Seeley said.
‘Die Hard’ and ‘Pulp Fiction’ actor Bruce Willis ends his acting career after being diagnosed with aphasia, his family announces.
The disease itself is the result of rogue proteins that clump together in the brain, but what triggers that protein formation is unclear.
Genetics play a role. Roughly 40% of FTD cases are familial, meaning there is some history of dementia in the patient’s family, according to the Assn. for Frontotemporal Degeneration.
Most people who are diagnosed with the condition have no family history of dementia at all. At the same time, having a parent or other biological family member with FTD is by no means a guarantee that you will develop the disease.
How is frontotemporal dementia different from Alzheimer’s disease?
“Dementia” is a broad term covering many types of brain impairment. The most common and best-known type is Alzheimer’s disease, which typically starts in the hippocampus, a part of the brain essential to memory formation. That’s why forgetting is the condition’s first and most characteristic symptom.
The disease then usually progresses through the brain in a predictable pattern, triggering new symptoms as it atrophies the tissues in different regions. From the hippocampus it moves on to the amygdala, provoking feelings of fear and anxiety; to the parietal lobes, disrupting physical sensation and spatial awareness; and finally to the frontal lobes, which manage memory retrieval, problem solving, sensory processing and communication.
Little-known brain disease rips apart lives of victim, loved ones
But for people with frontotemporal dementia, the damage starts there first. While personality changes, loss of inhibitions and difficulty remembering and maintaining relationships happen in the late stages of Alzheimer’s, those with FTD must confront those deeply difficult symptoms far earlier in the course of the disease.
“Whether it’s a behavioral or a language form of the disease, it’s taking away aspects of personhood that are really central to who we are. And so it’s so hard on the patients and the families,” Seeley said.
What is the prognosis and treatment?
The number of years people can live with frontotemporal dementia varies widely among patients, Mendez said.
The Assn. for Frontotemporal Degeneration says that once symptoms become apparent, the average life expectancy for patients is between seven and 13 years.
Some medications can help alleviate some of the disease’s symptoms. But at the moment, no treatment can stop or reverse the disease itself.
“Unfortunately,” Mendez said, “a central aspect of neurodegeneration is that it is insidiously, gradually progressive. And so eventually it causes death, like many of these illnesses do.”