COVID still kills in California, but the demographics of its victims are shifting
As California settles into a third year of pandemic, COVID-19 continues to pose a serious threat. But the number of people dying — and the demographics of those falling victim — has shifted notably from the first two years.
Given the collective immunity people have garnered through a combination of mass vaccination and earlier infections, Californians overall were far less likely to die of COVID-19 in 2022, when the Omicron variant dominated, than in 2020 and 2021, when other variants were largely at play. That mirrored a national trend.
Still, the coronavirus is killing hundreds of Californians each week, hitting hardest among the unvaccinated.
COVID-19 remained among the state’s leading causes of death in July, trailing heart disease, cancer, stroke and Alzheimer’s disease but outpacing diabetes, accidental death and a host of other debilitating diseases. In the first seven months of the year, about 13,500 California residents died of COVID-19, according to preliminary death certificate data from the state Department of Public Health. By comparison, the disease killed about 31,400 people in 2020 and almost 44,000 in 2021.
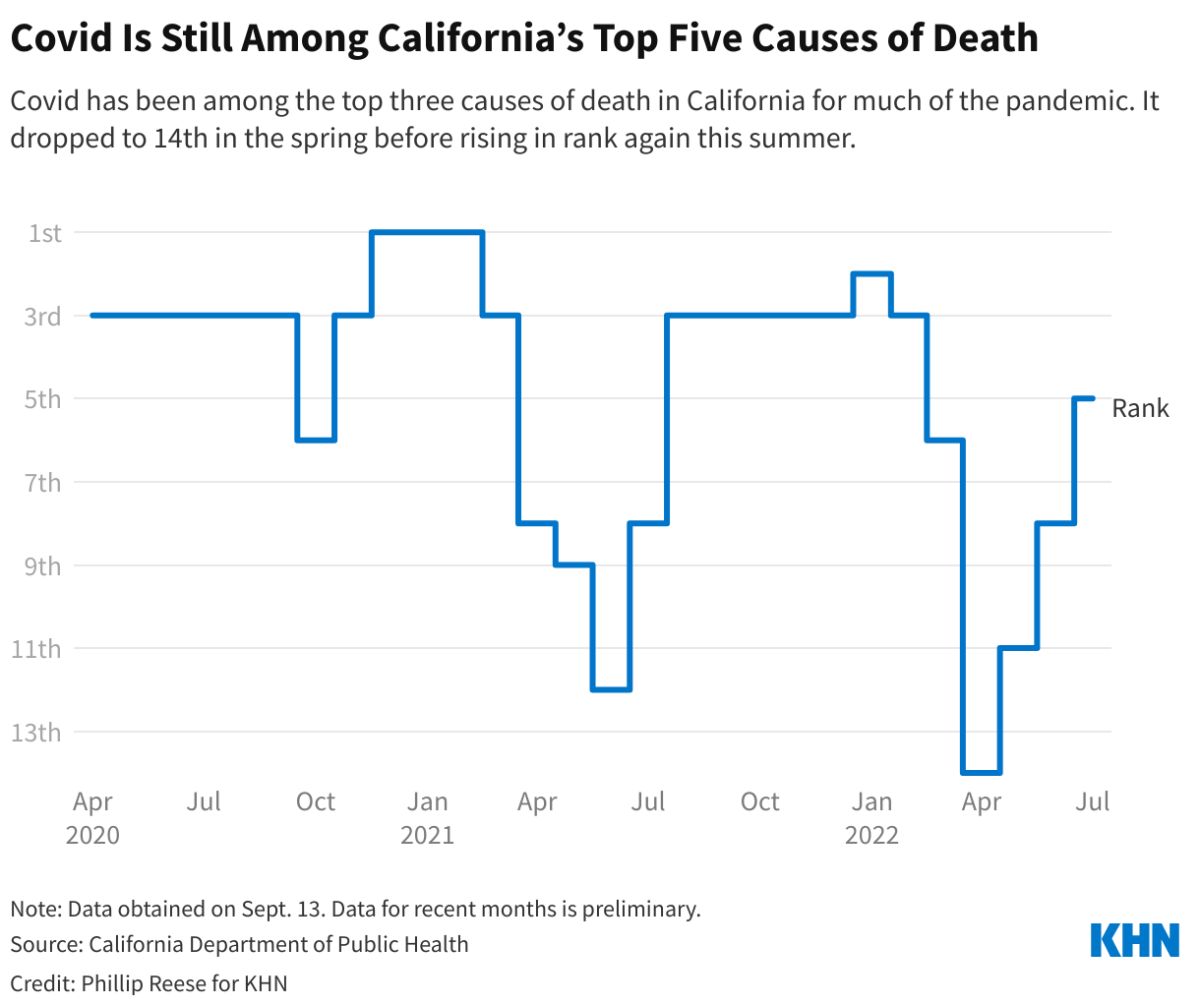
From April 2020 through December 2021, COVID-19 killed an average of 3,600 people a month, making it the third-leading cause of death in the state for that time period, behind heart disease and cancer. From December 2020 through February 2021, it briefly overtook heart disease as the leading cause of death, claiming the lives of more than 38,300 Californians in just three months. During its most recent peak, in January 2022, COVID-19 took about 5,900 lives.
COVID-19 fell out of the top 10 causes of death for a brief period in the spring, only to reenter this summer as new Omicron subvariants emerged. In July, even with more than 70% of Californians fully vaccinated, COVID-19 was the fifth-leading cause of death, cutting short more than 1,000 lives, state data show.
The death toll has fallen from past surges, but rates this summer still equate to COVID being one of the leading causes of death in the U.S.
Clearly vaccinations made a difference. COVID-19 death rates fell in recent months as vaccines and prior infections afforded much of the population significant protection against severe illness, said Dr. Timothy Brewer, a professor of medicine and epidemiology at UCLA.
Brewer also said the Omicron variant, while more transmissible than earlier strains, appears to be a milder version of the virus. Research into that question is ongoing, but preliminary data suggest Omicron is less likely to cause serious disease and death, according to the Centers for Disease Control and Prevention, which also notes that the severity of symptoms can be affected by vaccination status, age and other health conditions.
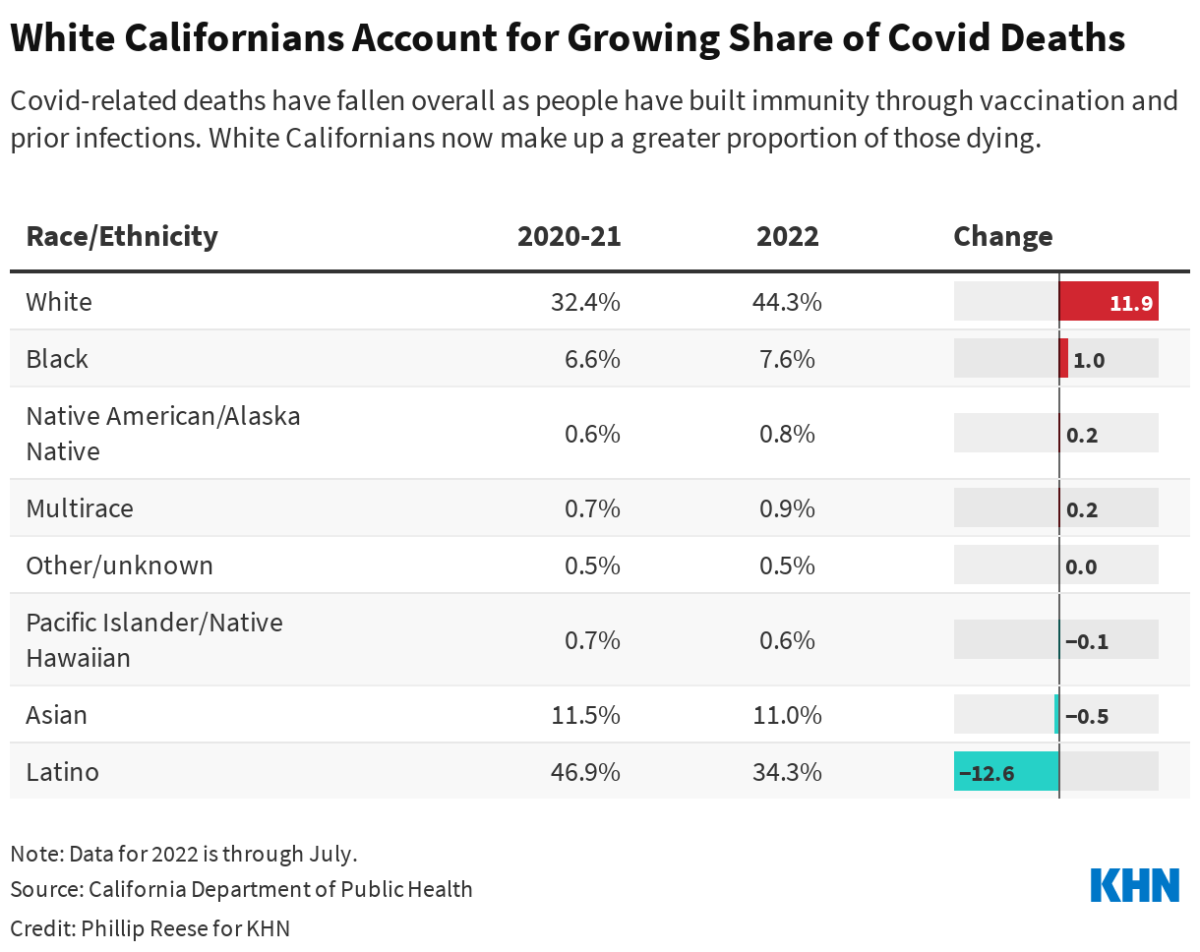
The decline in deaths was particularly striking among California’s Latino population.
In 2020 and 2021, Latino residents accounted for 47% of COVID-19 deaths in California — about 35,400 of them — although they make up 40% of the state’s population. By comparison, Latinos accounted for 34% of COVID-19 deaths from January through July 2022, according to state data. That translates to about 4,600 deaths.
Conversely, the proportion of COVID-19 deaths involving white residents increased from 32% in the first two years of the pandemic to 44% in the first seven months of 2022. That equates to 24,400 deaths of white residents in 2020-21 and about 6,000 deaths in the first seven months of 2022. White people make up about 35% of the state’s population.
Researchers point to several factors in the shift. During the first two years of the pandemic, large numbers of the workers deemed essential, who continued to report to job sites in person, were Latino, while white residents were more likely to be employed in occupations that allowed them to work from home, U.S. Census Bureau surveys show.
“They just got exposed more,” said Dr. George Rutherford, a professor of epidemiology and biostatistics at UC San Francisco. “They’re doing essential jobs and had to leave the house and go to work.”
Some bosses consider telework as a benefit. Many workers don’t see it that way but are willing to accept a lower salary, up to a point.
An imbalance in remote work remains, census data show, but today a large majority of both Latino and white workers in California are reporting to work in person.
Seciah Aquino, deputy director of the Latino Coalition for a Healthy California, said efforts to make sure testing, treatment and vaccinations were available to underserved communities of color also had an effect. And because Latino communities were hit so hard during the pandemic, she said, many California Latinos are still wearing masks.
“They are still making sure that they’re staying home if they’re sick,” she said. “They’re still abiding by those policies even if the greater narrative is changing.”
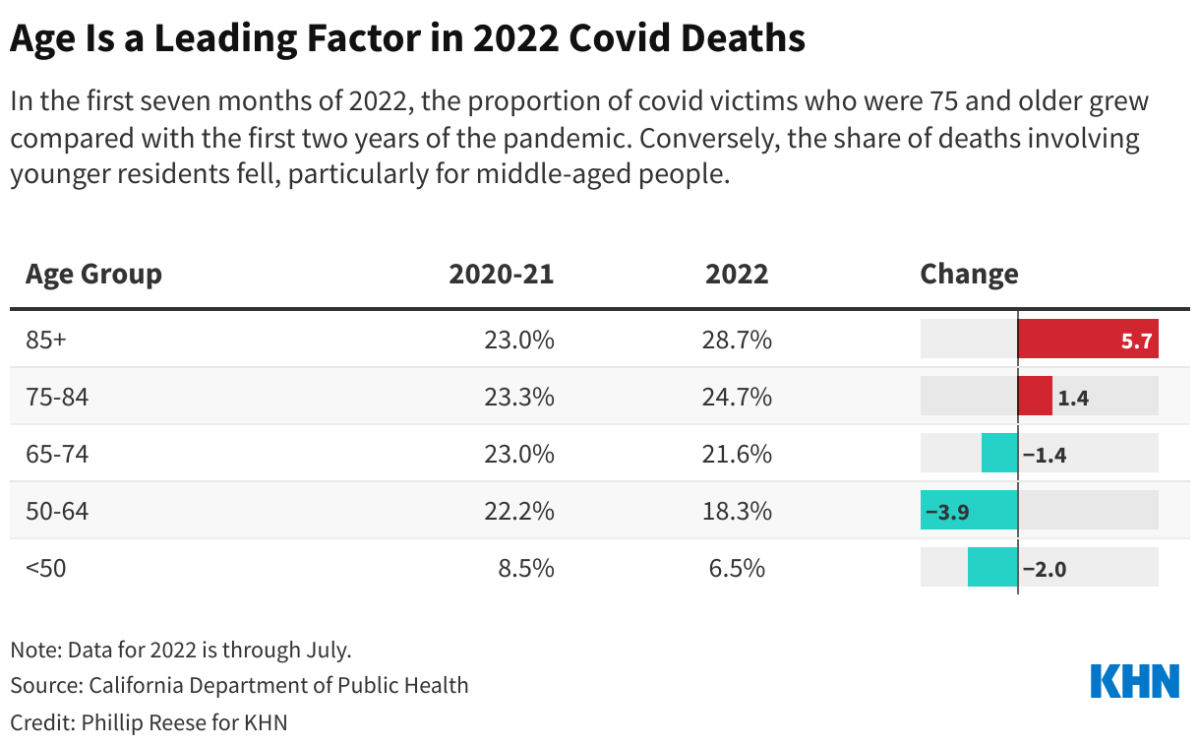
Age is also a key factor in the demographic shifts, Brewer said.
In 2022, Californians 75 and older made up 53% of COVID-19 deaths through July, up from 46% in 2020 and 2021. Only about 6% of the state’s residents are 75 and older. And white Californians 75 and older outnumber Latinos in that age group by about 3 to 1.
In the initial vaccination rollout, California prioritized seniors, first responders and other essential workers, and for several months in 2021 older residents were much more likely to be vaccinated than younger Californians.
“Now, the vaccination rates have caught up pretty much with everybody except for kids, people under 18,” Brewer said. “You’re seeing it go back to what we saw before, which is that age remains the most important risk factor for death.”
An analysis of death certificates from January to April showed COVID-19 deaths were nine times those caused by motor vehicles and more than five times the rate for flu and pneumonia.
More than 86% of Californians age 65 and older have completed their primary COVID-19 shot series. But the protection afforded by vaccines wanes over time, and since many seniors got their shots early, enough time passed between their second shot and the Omicron wave of early 2022 to leave them vulnerable. About one-third of Californians 65 and older had not received a booster by early 2022, when the Omicron wave peaked, and about one-quarter still haven’t received a booster.
Geographic shifts in COVID-19 prevalence have occurred throughout the pandemic: Outbreaks hit one area while another is spared, and then another community serves as the epicenter a few months later.
Residents of the San Francisco-Oakland metro area accounted for 7.8% of the state’s deaths in 2022, through early September, up from 5.4% in 2020-21. The area is home to about 12% of the state’s residents. The Sacramento metro area has accounted for a higher share of COVID-19 deaths this year: 6% in 2022 versus 4.5% in 2020-21.
At the same time, Los Angeles-Long Beach-Anaheim metro residents made up 42% of COVID-19 deaths in 2022, down slightly from 43% in 2020-21. The area is home to about 33% of the state’s residents. A similar dip occurred in the nearby Riverside-San Bernardino metro area.
L.A. County coronavirus weekly death rate 70% higher than in Bay Area: Why so much worse?
Again, age could be a factor in the geographic shifts. A higher proportion of residents in San Francisco and Sacramento are 75 and older than in Los Angeles and Riverside, census data show.
It’s unclear whether this shift will last. COVID-19 deaths grew at a faster pace in July in L.A. County than they did in the Bay Area.

The data also show that vaccination remains one of the strongest deterrents to death from COVID-19.
From January through July, unvaccinated Californians died at roughly five times the rate of vaccinated Californians. But the gap was much greater before. From April through December 2021, California’s unvaccinated residents died, on average, at around 10 times the rate of vaccinated Californians.
Brewer said the gap lessened because Omicron was more likely than earlier variants to “break through” and cause infections in vaccinated Californians. The Omicron variant, though less deadly, also infected many more people than earlier variants.
This trend, too, may prove short-lived: The next generation of COVID-19 booster shots are rolling out across the state, and they target Omicron as well as the original coronavirus strain from China.
Phillip Reese is a data reporting specialist and an assistant professor of journalism at California State University Sacramento.










