Why easing COVID-19 restrictions too soon could be a boon for coronavirus variants

COVID-19 vaccine rollout has accelerated to more than 2 million shots per day in the United States. A more transmissible coronavirus variant from the U.K. is muscling its way across the country. And governors from Texas to Massachusetts are racing to loosen mask mandates and strictures on gatherings and reopen gyms, restaurants, workplaces and schools.
For a virus in search of new ways to spread and sicken, this convergence of events is a moment of unique opportunity, and new research underscores the peril.
Two studies published this week in the journal Science explore some of the circumstances that are known to give rise to new genetic variants of the SARS-CoV-2 virus.
In both a mathematical modeling exercise and a genetic deep dive into 1,313 coronavirus samples, researchers show that worrisome genetic changes to the virus are most likely to take root and spread when infection rates surge, when many people have only partial immunity, and when the virus is made to work harder to find its next victim.
The findings suggest the coming months could bring new challenges to a country already battered and exhausted by pandemic and eager for life to return to normal.
There’s reason for hope as well as worry.
The Centers for Disease Control and Prevention projected in late January that the U.K. coronavirus variant known as B.1.1.7 would overtake existing strains in the United States by late March. At that point, the CDC projected, B.1.1.7, which is roughly 50% more transmissible and is thought to be more virulent, would drive a resurgence of infections in the U.S.
That grim projection would probably have been less stark had the CDC foreseen the dramatic rise in vaccinations. With more than 95 million doses administered as of Wednesday, 24% of American adults have received at least a first dose of vaccine, and 12.9% have been fully vaccinated.
Meanwhile, the seven-day moving average of new coronavirus cases has plummeted from a high of 249,360 on Jan. 11 to 62,555 as of March 5. Many state governments have seized on the decline to roll back public health restrictions.
Dr. Rochelle Walensky, director of the CDC, has sought to walk this tightrope between hope and fear. The prospect of new viral variants, and of the conditions that foster their emergence, has been her central message to the public.
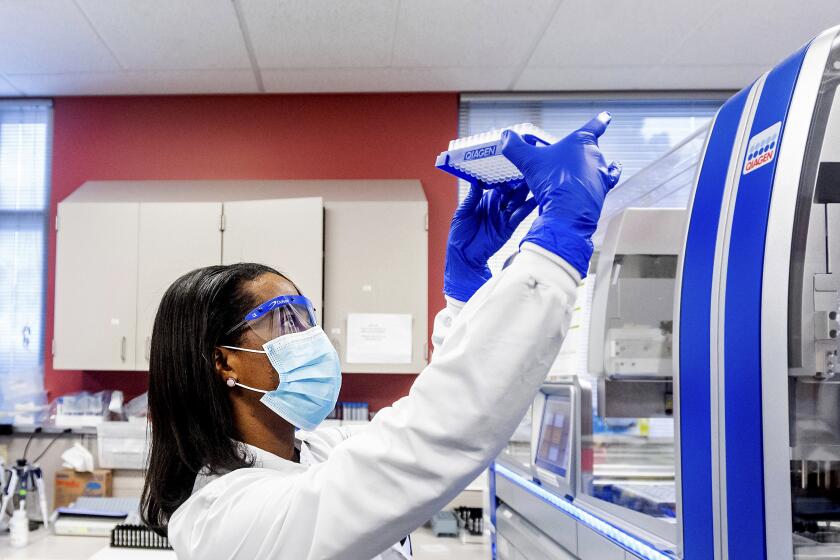
The Biden administration is boosting efforts to identify and track coronavirus variants to help scientists see where the pandemic is heading next.
“The more virus that’s circulating, the more variants that are possible,” Walensky said on MSNBC. “And those variants can emerge and diminish the effect of the vaccine. So while we’re vaccinating people, we want to make sure there’s less and less virus circulating that doesn’t put our vaccine efficacy at risk.”
March and April “are critical periods here,” Walensky added. It’s a race between vaccines and variants, and a rapid vaccine rollout is the nation’s most potent counter to threats like the U.K. strain. Mask-wearing, social distancing and limits on gatherings “give us a fighting chance to get vaccine to as many people as possible” before cases surge again and create conditions that are ripe for the emergence of new variants, she said.
The new research in Science bears out her concerns.
In one of the studies, researchers from Oxford University led an effort to watch “evolution in action.” They collected and genetically sequenced a series of viral samples from Britons who tested positive for coronavirus infection between March and June 2020. Their goal: to see up close how the virus changed as it moved from person to person and household to household.
This work revealed that mutations that threaten the effectiveness of COVID-19 vaccines or medicines arise only rarely in any single individual. When they do, they are rarely passed on in a sustained chain of transmission.
But the story was different for mutations with the potential to make the virus more transmissible or more virulent.
Like the “escape mutations” that erode vaccine efficacy, these genetic changes tended to get bottled up at their source. But their sheer volume made transmission of some mutations more likely, the authors said. These changes were happening “with sufficient frequency that even a rare transmission event … could result in rapid spread.”
Drop that prospect of “rapid spread” into a situation in which masks are coming off, diners are filling restaurants and fitness instructors are shouting encouragement to their students, and both the ignition and the fuel for a feared new wave are laid in place, experts said.
COVID-19 patients who take months to overcome their coronavirus infections despite treatment can become incubators of dangerous new strains.
“This finding underscores the need to limit subsequent waves of infection in order to decrease the likelihood of new, more contagious and virulent variants emerging,” said Dr. Joshua T. Schiffer, an infectious disease physician at the Fred Hutchinson Cancer Research Center in Seattle. “The more infections you have, the higher the probability that this can happen.”
Schiffer added that scientists increasingly fear a scenario that can arise when an initial outbreak is followed by a second one a couple of months later: Immunocompromised patients who have failed to clear an infection in the first wave become potent incubators of new viral strains that threaten to spread as a new surge kicks in.
“The best upstream strategy,” he said, “is just to prevent variants from happening in the first place. And to do that requires dampening a new wave of infections.”
In the second study, a team of infectious disease modelers set out to glean the impact of extending scarce supplies of vaccine by delaying the second dose of a two-dose vaccine regimen.
The answer, they found, relied heavily on an X-factor that likely changes from vaccine to vaccine: the level and duration of immunity conferred by a single dose. If a vaccine’s first shot confers somewhat strong protection against COVID-19, and if that protection doesn’t wane before a second shot can be delivered, then the regimen could effectively slow transmission, the researchers concluded.
But if stretching out first and second doses were to leave large swaths of the population with compromised immunity — enough to prevent death, perhaps, but not enough to stamp out infection completely — “the outcome could be more pessimistic,” the authors wrote.
Essentially, people who are only partially vaccinated could fail to clear a coronavirus infection in the same way that immunocompromised patients do. That means the virus, under pressure to evolve ways to circumvent the effects of vaccine, would find a plentiful supply of hosts in which to spawn genetic mutations.
Mixing and matching doses of different COVID-19 vaccines was an idea that scientists dismissed out of hand. Now they’re taking it seriously.
Some of those mutations could change the virus’ behavior in ways that make it more dangerous for its hosts and fuel its ability to spread.
Most ominously, they could undermine efforts to end the pandemic through mass vaccination by encouraging the emergence of viral variants that make vaccines less effective, the researchers wrote.
“A vaccine strategy with a very long inter-dose period could lead to marginal short-term benefits (a decrease in the short-term burden) at the cost of a higher infection burden in the long term and substantially more potential for viral evolution,” the authors wrote. The risk is particularly high “in places where vaccine deployment is delayed and vaccination rates are low.”
If such variants emerge, the threat won’t be limited to the countries in which they arise, the study authors added: “This underlines the urgent need for global equity in vaccine distribution and deployment.”
University of Minnesota pandemic expert Michael Osterholm warned that low- and middle-income countries whose populations remain largely unvaccinated will not only sustain the pandemic: As long as their vaccination needs are neglected, they will also become a bottomless source of new coronavirus variants.
“That’s where the variants are going to spin out fast and furious,” said Osterholm, who directs the Center for Infectious Disease Research and Policy. “We’re going to have to take care of those low- and middle-income countries — not strictly as a humanitarian issue but also as a means of protection.”