Will children spread COVID-19 if they go back to school?
Is it safe for children to return to school while the coronavirus is on the loose?
That depends on what’s likely to happen if a student becomes infected. Will the virus jump to his classmates, who could then fuel its spread throughout the student body? Will it find its way to his teacher and hitch a ride to the break room, putting the faculty on campus at risk as well?
Scientists don’t have definitive answers to questions like these — and they probably won’t for quite awhile.
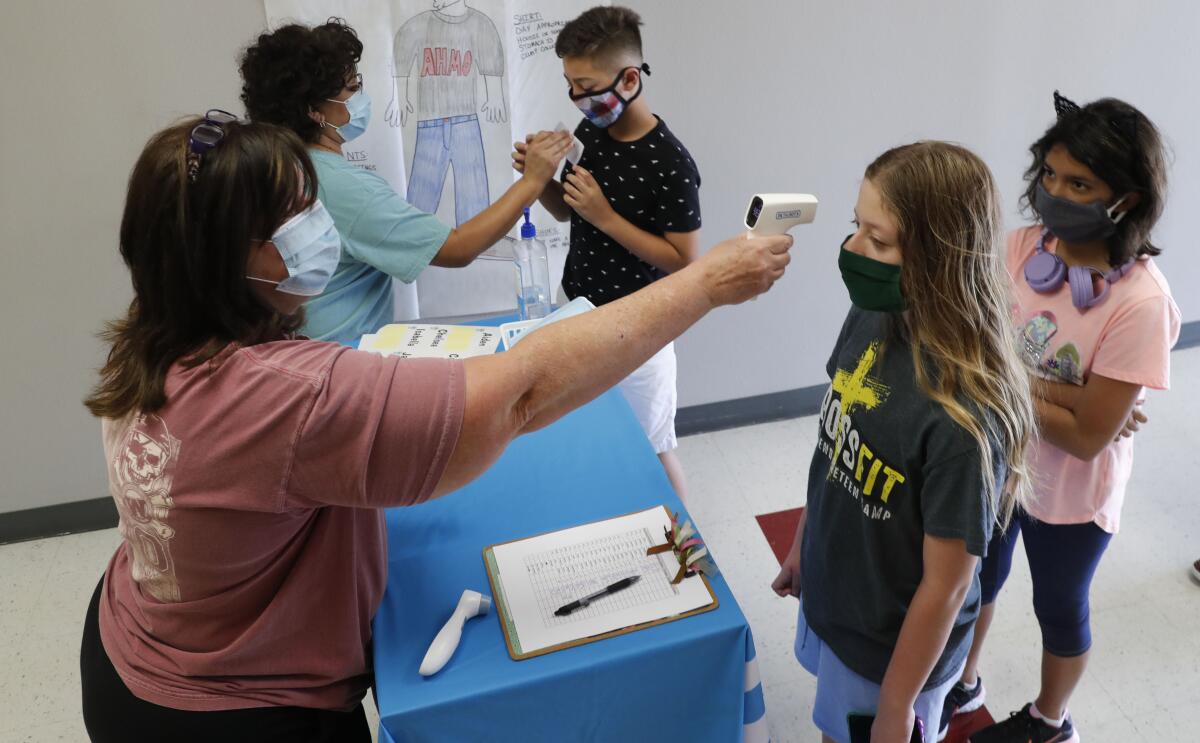
Schools are coping with this uncertainty in different ways. In Southern California, the state’s two biggest districts — Los Angeles Unified and San Diego Unified — said they would begin the new school year with full-time distance learning. Sandwiched between them is Orange County, where the Board of Education voted to let students come to campus without requiring masks or social distancing.
A report released Wednesday by the National Academies of Sciences, Engineering, and Medicine acknowledges the bind schools are in.
“There is insufficient evidence with which to determine how easily children and youth contract the virus and how contagious they are once they do,” the report says. This knowledge gap “makes it extremely difficult for decision-makers to gauge the health risks of physically opening schools and to create plans for operating them in ways that reduce transmission of the virus.”
But decisions must be made anyway. Here’s a closer look at what scientists do know about kids and COVID-19 — and what it suggests about the risks of sending them back to school.
Do children have some kind of natural protection against the coronavirus?
They do seem to be less susceptible to the virus, and that’s especially true for younger children.
Data from the U.S. Centers for Disease Control and Prevention show that, through May 30, the incidence of COVID-19 was 51.1 cases per 100,000 children under 10 and 117.3 cases per 100,000 kids and young adults between the ages of 10 and 19. Both of those figures were well below the nationwide figure of 403.6 cases per 100,000 Americans.
Scientists aren’t sure what accounts for this phenomenon. One theory is that children’s cells have fewer of the ACE2 receptors that the coronavirus needs to bind to in order to initiate an infection. Researchers analyzed the level of ACE2 gene expression in 305 people between the ages of 4 and 60 and found that it increased steadily with age.
“Lower ACE2 expression in children relative to adults may help explain why COVID-19 is less prevalent in children,” the researchers reported in the Journal of the American Medical Assn.
But that doesn’t mean kids can’t get sick. Indeed, a small number of pediatric patients have developed a serious disease called multi-system inflammatory syndrome, or MIS-C, in children.
“While the balance of the data shows that kids are less susceptible to infection and less likely to transmit it, less susceptible doesn’t mean they’re not susceptible,” Dr. Scott Gottlieb, former commissioner of the Food and Drug Administration, said this week on Face the Nation.
If children are less likely to be infected, doesn’t that mean they’re less likely to spread it?
Probably. After all, you can’t spread a virus if you don’t have it in the first place.
Some health experts suspect that one reason infection rates have been lower in kids than adults is that they’ve been relatively isolated at home while their parents have left the house to work, shop or socialize. Once kids are back in school, they might start to catch up.
COVID-19 claims the lives of Black and Latino Americans earlier than it does for whites. Nonwhite victims are typically a decade younger than whites, the CDC says.
Even so, there’s evidence that kids just don’t have the same coronavirus-spreading power as adults. Studies that tracked how infections spread through households in the U.S., Switzerland, and several countries in Asia have shown that adults are far more likely than kids to bring the virus into their homes, said Dr. Naomi Bardach, a pediatrician and policy researcher at UC San Francisco.
“Most often, the adult in the household was the one who was originally infected,” added Dr. Ibukun Christine Akinboyo, medical director of pediatric infection prevention at Duke University Medical Center. “If it was the child, there seemed to be a less than 15% risk that the child would transmit across the household.”
Should we be thinking about kindergartners the same way as high school seniors?
No. For one thing, infection rates are lower for elementary school-age kids than for teenagers.
Another consideration is that secondary school students can do more to protect themselves than young children. For instance, they should be able to wear a mask the whole time they’re on campus, something kindergartners probably can’t handle. Older students ought to be better at social distancing as well.
And when they get home, high schoolers can operate more independently than elementary school kids. That could help mitigate the risk that a teenager, if infected, would pass the virus along to family members at home, said Dr. Charlene Wong, a pediatrician who also studies health behaviors at Duke University.
Is it safe for kids to be on campus if they’re too young to keep a mask on their face?
Pediatricians recognize that younger kids may not wear masks at all times, stay apart from their classmates, or keep their hands away from their faces. But since they’re less vulnerable to infection, that’s probably OK, they said.

Data from the Netherlands back up the idea that “children play a minor role in the spread of the novel coronavirus,” said Dr. George Rutherford, an infectious diseases expert at UCSF.
That country allows children up through the age of 12 to get close to both kids and adults without having to worry about social distancing, he said. Even teens ages 13 to 17 can be in close contact with each other. But since adults account for the bulk of viral spread, they need to stay at least six feet away from each other whenever possible.
What has happened in other countries when students went back to school?
Generally speaking, not much. For example:
• A report from Australia’s National Center for Immunization Research and Surveillance examined 15 schools in New South Wales that reported COVID-19 cases in March and April. Nine students had confirmed coronavirus infections during that time, and they may have spread it to a grand total of two fellow students out of 735 who were considered “close contacts.” Nine adults in those schools caught the coronavirus as well, but they did not spread it to any of their 128 “close contacts” among teachers and staff, health officials concluded.
• Ireland’s first known COVID-19 patient was a child who visited Northern Italy in early March, just as that country’s coronavirus crisis was beginning to take off. Schools in Ireland were closed soon after, on March 12; by then, health officials had identified a total of three infected students — one in primary school and two in secondary school — along with a teacher and two other adult instructors. None of the kids’ 924 fellow students caught the virus from them at school, nor did 101 school-based contacts of the three infected adults. Even outside of school, the six infected people didn’t spread the virus to any of the 1,001 children who were among their close contacts, according to a report in the journal Eurosurveillance.
• A study published in the journal Clinical Infectious Diseases traced what happened after an English tourist who caught the coronavirus in Singapore visited a ski chalet in France. He spread the virus to 11 others, including one child who later visited three schools and a ski class. None of that child’s contacts became infected.
• In the Netherlands, schools and childcare centers began reopening on May 11, and by June 8 students had returned to campus full time. The country’s National Institute for Public Health and the Environment said it received “a few reports” of infections among school employees since resuming normal operations, but none of them caught it from children on campus. In addition, the average number of people who contract the virus from a single infected person has remained below one since March.
The older you are, the greater your risk for a severe case of COVID-19, the CDC says as it expands its list of risky underlying health conditions.
Although no significant coronavirus outbreaks have been traced to schools, that doesn’t mean it couldn’t happen in the future, Akinboyo said, especially since the virus is more widespread in the community now than it was in the early days of the pandemic.
We should also keep in mind that the U.S. population is more diverse than in most other countries, so their experiences may not reflect what is likely to happen here, said Lisa Gennetian, a Duke economist who studies childhood poverty.
Closing down schools and switching to distance learning were hugely disruptive. Did it actually help slow the pandemic?
It seems like the answer ought to be yes, but it might have helped less than you’d think.
Several studies have tried to quantify the benefits of measures aimed at slowing the spread of the coronavirus, including quarantines, stay-at-home orders, school closures and social distancing policies. Together, these policies did seem to impede transmission of the virus, though by how much isn’t clear.
A new tracker from Johns Hopkins University lets you compare the trajectory of coronavirus cases in each state with the reopening policies there.
One preliminary study that focused on Hong Kong found that measures aimed at keeping people apart may have reduced community spread by as much as 44%, but the authors did not estimate how much of that benefit could be attributed to closing schools.
A review in the journal Lancet Child and Adolescent Health turned up only one study that used models to estimate the impact of school closures on community health. Members of the Imperial College COVID-19 Response Team calculated that if all primary and secondary schools were closed, along with 25% of universities, COVID-19 deaths in the United Kingdom would be reduced by 2% to 4%. In part, those numbers are low because the benefit of keeping children out of school was offset by a 25% increase in their time spent in the community, not to mention a 50% increase in close contact with family members.









