Malaria drugs aren’t the only ones on the shelf that might help coronavirus patients

When a pandemic springs up as fast as the one sparked by the novel coronavirus, doctors must rummage around in their medicine cabinets for drugs that are already available and might be repurposed to treat a wholly new disease.
Treating patients with mild or moderate COVID-19 is essentially a preventive mission: The principal aim is to stop the disease from progressing to a severe stage that would typically require mechanical ventilation.
But it’s hard to slow or disrupt the progress of an infection when you have only begun to see how it unfolds. And it’s inherently difficult to prove that a particular medicine has prevented severe illness or death when neither was never a sure bet in the first place.
Given the lack of other good options, doctors are forced to try these medicines anyway.
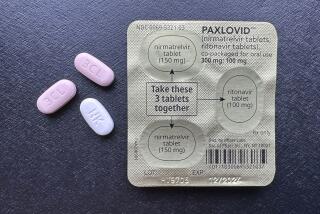
Among the best known are several antiviral medications — remdesivir, lopinavir and ritonavir — that were developed to treat Ebola and AIDS.
All of those medications are the focus of a U.S.-sponsored international trial with as many as 60 sites. It could begin producing preliminary results in the coming weeks, said one of its principal investigators, Dr. Andre Kalil of the University of Nebraska Medical Center.
The World Health Organization has called remdesivir, which was developed (but failed) to treat Ebola, the “most promising” antiviral to treat COVID-19. It was widely used on patients in China, and the results of clinical trials conducted there are also expected in the coming weeks.
Gilead Sciences Inc., which makes remdesivir, is also sponsoring a major trial of its drug at 93 sites, including 18 in California.
President Trump has touted the drugs chloroquine and hydroxychloroquine, used to treat malaria, rheumatoid arthritis and the autoimmune disease lupus, as a potential “game changer.” And they, too, are being tested as a treatment for moderate COVID-19 cases in two U.S. trials and many more around the world.
President Trump’s hype of a potential treatment for COVID-19 gives false hope to virus patients and causes real harm to others.
There’s also a passel of less celebrated drugs and therapies that are being tested in the United States and abroad. Some seem like a shot in the dark. Some are dangerous. And a few are truly promising.
But anything that shows promise in keeping people with COVID-19 off ventilators is getting a look from scientists.
Consider thalidomide. It was prescribed from 1957 to 1962 as a morning-sickness drug, but was pulled from the market after it was found to cause stunted limbs in babies born to mothers who took it. Now it’s used to treat leprosy and multiple myeloma, and was considered as a treatment for lung injury caused by the H1N1 flu virus when it first appeared in humans in 2009.
Thalidomide appears to tamp down inflammation in the lungs, reduce scarring, and rein in an overactive immune system. In Wenzhou, China, scientists are planning to test whether the drug could shorten the time to recovery in patients with pneumonia caused by the novel coronavirus, and reduce the proportion of patients who need mechanical ventilation or die.
Recombinant human interferon is another drug with serious side effects. It’s used to treat some viral infections, as well as cancers like leukemia and melanoma. But it can cause depression, nausea, sleeplessness and flu-like symptoms that some would say make COVID-19 look like a day at the beach.
In labs, interferon slowed or stopped the growth of two coronaviruses related to the one that causes COVID-19 — the viruses responsible for severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). Scientists think the drug might help bottle up this coronavirus too, giving the immune system a chance to kill it. Clinical trials are either planned or underway in China, Italy and France.
Medicines designed to treat COVID-19 won’t be available for months, so doctors are looking to drugs already approved for treating other diseases.
In China, where the government remains a champion of traditional medicine, researchers are also testing herbal remedies which may prove to have antiviral properties. In China, Huaier granule, a mushroom-derived elixir that’s been used in traditional medicine for 1,600 years, will be tested in 550 people with mild COVID-19.
Tetrandrine, drawn from the root of a vine that grows in China and used in Chinese medicine to treat inflammatory lung diseases, will get a trial there too.
The antiviral favipiravir was developed by the Japanese firm Fujifilm Toyama Chemical to treat influenza and other RNA viruses by disrupting their ability to replicate inside human cells. Since the novel coronavirus also stores its genetic code in RNA, scientists thought it might clear COVID-19 infections more quickly.
Favipiravir was tested in a group of 340 COVID-19 patients in China whose illness was not severe. Half of the participants in the randomized controlled trial got favipiravir, and they cleared the new coronavirus in a median time of four days. The other half of study participants got the drug Arbidol, an antiviral medication widely used to treat flu patients in China and Russia, and it took a median of 11 days for them to clear the virus.
In addition, lung function improved in 91% of those who got favipiravir, compared with 62% of those who got Arbidol.
Favipiravir is now being tested in patients with moderate COVID-19 disease at 11 sites in China, along with the antiviral tocilizumab, a biologic drug that dampens the immune system in patients with rheumatoid arthritis. That property could be key: Although a robust immune system reaction is important during the initial stages of fighting off COVID-19, in patients who fare worst, it is most often immune overreactions — so-called “cytokine storms”— that lead to multiorgan failure, and often death.