Women are giving up on in vitro fertilization too soon, study says

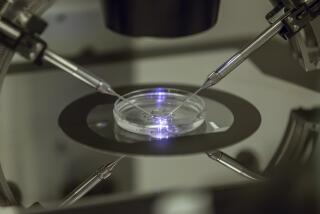
A doctor performs an embryo transfer in a fertility clinic. Although many women abandon IVF treatment after three or four unsuccessful attempts, a study shows the odds of success continue to rise through as many as nine cycles.
Too many women give up on in vitro fertilization too soon, a new study suggests.
After analyzing more than 250,000 in vitro fertilization attempts by more than 150,000 women over nearly a decade, researchers found that women could keep increasing their chances of having a live birth through up to nine IVF cycles, according to a report in Wednesday’s edition of the Journal of the American Medical Assn.
What’s more, the researchers defined an IVF cycle more expansively than experts have done in the past. Instead of considering each attempt to transfer one or more embryos into the womb as an individual cycle, the authors of the JAMA study counted each attempt to stimulate the ovaries and retrieve eggs as the beginning of a new cycle. That means each cycle may include multiple attempts to transfer embryos.
The conventional wisdom in assisted reproduction circles is that women who do not have a baby after three embryo transfers suffer “repeat implantation failure,” the study authors wrote. Also, doctors continue to be guided by an outdated study that said live birth rates decline after four IVF cycles. Together, these have prompted many women to abandon fertility treatment after three or four unsuccessful embryo transfers.
The study authors, led by medical statistician Andrew Smith of the University of Bristol in England, had a hunch that at least some of these women were giving up too easily. So they gathered data on 156,947 women in the United Kingdom who completed 257,398 cycles of IVF. (The UK Human Fertilisation and Embryology Authority collects detailed data on assisted reproduction.) All of the cycles began between Jan. 1, 2003, and Dec. 31, 2010, and subsequent embryo transfers were tracked through June 2012.
Altogether, 30% of the women had a live birth after their first IVF cycle, and the live-birth rate was at least 20% for the next three cycles, the researchers found. After that, the live-birth rate declined in each additional cycle, but the cumulative odds having a baby continued to rise through nine cycles.
After accounting for a woman’s individual prognosis based on her age when she began treatment and the number of eggs collected in her previous cycle, the researchers calculated that a woman had a 69% chance of having a baby by the end of nine IVF cycles.
For the sake of comparison, the researchers estimated that 58% to 74% of women under 40 who tried to conceive naturally for one year would wind up with a baby.
Some women had better odds with IVF than others. For instance, women under 40 who were using their own eggs had a 68% chance of having a baby by the end of six cycles; after nine cycles, their odds of a live birth were 72%.
On the other hand, women ages 40 to 42 had only a 33% chance of a live birth after nine IVF cycles, and women older than that had a 16% chance of a live birth after nine cycles, the researchers found.
Women could erase this age differential by using donor eggs instead of their own. In these cases, 30% of women had a baby in any given cycle, up to and including the ninth cycle. By the end of six cycles with donor eggs, the cumulative chance of a live birth was 87%, according to the study.
When the fertility problem could be traced to the male partner, some women used a treatment that involved injecting a single sperm into each egg. In those cases, the odds of having a live birth by the end of six cycles were 71%. When women used donor sperm instead, their odds of a live birth after six cycles were 81%.
The findings should encourage many women to continue with fertility treatments for longer than they initially planned, Smith and his colleague concluded. But even though that sixth, seventh or eighth IVF cycle might be the one that produces a baby, it doesn’t mean every patient will want to stick with it that long.
“For some couples, the emotional stress of repeat treatments may be undesirable, and the cost of a prolonged treatment course, with several repeat ovarian stimulation cycles, may be unsustainable for health services, insurers, or couples,” they wrote. “However, we think the potential for success with further cycles should be discussed with couples.”
An editorial that accompanied the study agreed that these findings should be shared with fertility patients “so that they can make a truly informed decision.”
The study authors did not attempt to do a cost-benefit analysis of continuing for treatment for up to nine cycles; indeed, they noted, other researchers have laid out the many difficulties of doing so, since the definitions of “costs” and “benefits” of reproduction can be so subjective.
Still, they did a rough calculation (assuming two attempts at embryo transfer per cycle) to determine that six cycles of IVF would cost up to $132,000, compared with $66,000 for the more traditional three cycles.
Follow me on Twitter @LATkarenkaplan and “like” Los Angeles Times Science & Health on Facebook.