More babies, fewer multiple births, are resulting from assisted reproduction
Assisted reproduction is on the rise in the United States, resulting in the birth of 65,175 babies in 2014, says a new report.
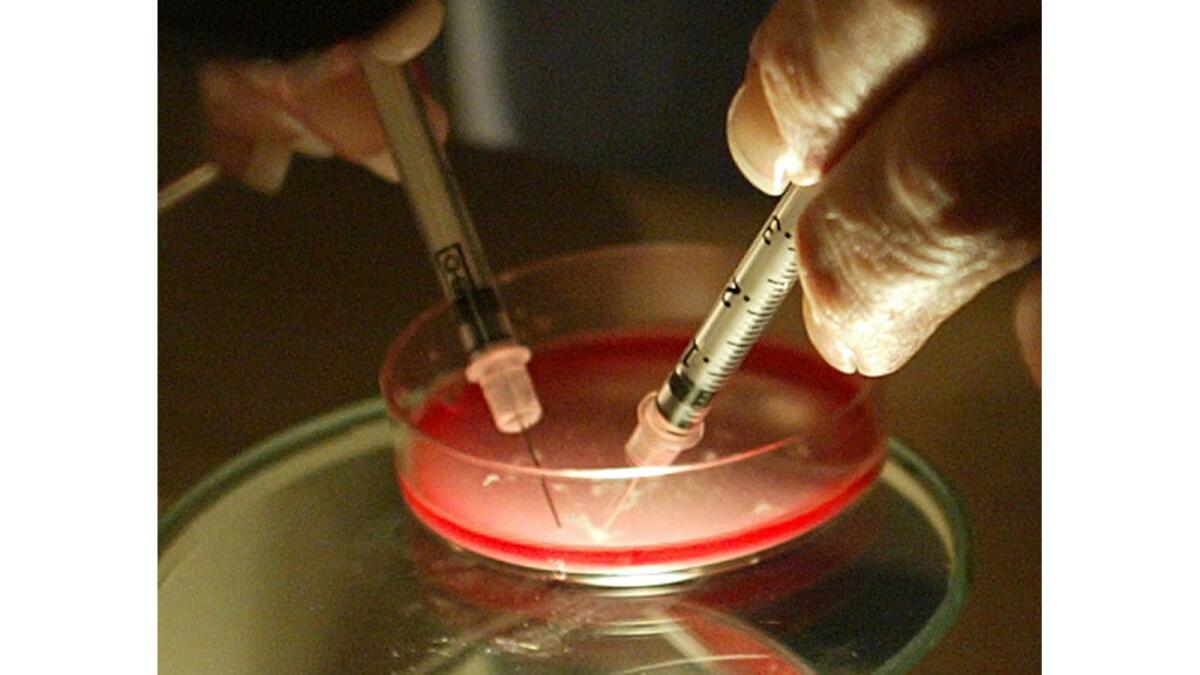
2014 saw the birth of more babies than ever who got their start in the petri dish of a fertility clinic in the United States. In its yearly review, the Society for Assisted Reproductive Technology reported a total of 65,175 live births resulting from a variety of procedures -- up from 63,286 in 2013.
Amidst growing concern about the numbers of twins and triplets born to women who undergo infertility treatments, the assisted reproduction industry also detailed its progress in driving down the rate of multiple births, and for the first time reported pre-term births among its patients. Some 78% of babies born to women who underwent such procedures as in vitro fertilization were singletons, up from 75.5% in 2013.
In 2014, between 22% and 31% of women undergoing infertility treatment were electing to have just a single embryo transferred, with women under 35 choosing that option at higher rates than women over 40. That rate of “elective single-embryo transfers,” however, remains much lower than physician groups have called for.
Infertility treatments generate an estimate 18% of all twin deliveries in the United States, according to the American College of Obstetricians and Gynecologists. Mothers carrying more than one baby in a pregnancy are at greater risk of birth complications, as are the babies they bear.
The nation’s 375 assisted reproduction practices performed 190,384 assisted reproduction cycles in 2014 -- up from 174,962 the year before. That uptick reflects a major acceleration of growth in infertility clinics’ business since 2009, when a flagging economy cut deeply into a medical practice that relies on patients’ willingness to bear steep out-of-pocket treatment costs.
A single cycle of in vitro fertilization treatment, which includes the stimulation of egg growth with medications, a procedure to retrieve those eggs, fertilization and incubation, and eventual transfer of embryos into a woman’s uterus, can cost between $15,000 and $18,000 including the cost of medications. While health insurance may cover some of those expenses for some women, much of the cost is borne by patients themselves.
As a result, the medical practice of assisted reproduction has been largely self-regulated and strongly entrepreneurial. As the leading industry group for infertility clinics and practices, the Society for Assisted Reproductive Technologies has tracked and produced yearly reports on the industry’s activities since the mid-1980s.
The number of procedures performed in 2014 represents a 43% growth in two years alone, said Jake Anderson-Bialis, co-founder with his wife, Deborah Anderson-Bialis, of FertilityIQ, a website that allows patients to review and compare fertility practices. Both said the increase appears to be driven by the economy’s recovery, by a continuing surge in older women and gay and lesbian couples seeking treatment, and by an increase in the number of procedures individuals are willing to undergo.
IVF was the most commonly performed procedure, and its success remained closely tied to the age of the woman seeking to use her own eggs to produce a child. Among women under 35 using their own eggs to conceive a baby by IVF, 48.6% of 40,805 IVF cycles initiated resulted in the live birth of a child. But the percentage of successful outcomes declined to 38.3% among women 35-37 and to 24.3% among women 38-40.
Among women 41-42, 12.3% of IVF cycles using a woman’s own eggs resulted in a live birth, and the success rate plummeted to 3.8% for women older than 42.
Those rates of live births reflect the growing use of embryo-freezing in U.S. fertility clinics. In some cases, multiple attempts to initiate a pregnancy using embryos that resulted from a single IVF cycle were required to achieve those success rates.
The Society for Assisted Reproduction Technology’s annual report shows that the number of women looking to conceive babies using eggs that come from someone else continues to increase. In 2014, some 9,961 cycles were initiated in which eggs were harvested from one woman, fertilized with sperm, and transferred into the uterus of another woman.
Roughly 70% of those procedures used eggs freshly produced by egg donors, which resulted in a live birth in 53.5% of cases. The remaining 30% of egg donor cycles were performed with frozen eggs, resulting in a live birth 38.5% of the time.
The growth of egg donor cycles, said Jake Anderson-Bialis of FertilityIQ.com, is substantial, with close to 700 more such procedures in 2014 than in the previous year.
“This idea is clearly taking hold,” said Anderson-Bialis. “The data suggests it’s going to be a trend.”
The Society for Assisted Reproduction Technology has aimed to improve its reporting of outcomes, the website co-founders said. But they added that the SART website, and efforts by the Centers for Disease Control and Prevention to track the rise of infertility treatments, have done little to help women and couples looking to compare practices and find ones that will help them build their families. That shortcoming prompted the Anderson-Bialises to build an independent website, which launched in mid-February, to help consumers of assisted reproduction services assess clinics and practitioners.
Follow me on Twitter @LATMelissaHealy and “like” Los Angeles Times Science & Health on Facebook.







