Opinion: Surgeons give patients too many opioids. A few simple steps could curb excess prescribing

America’s opioid epidemic is as bad as it has ever been. Although the sharp increase in opioid overdose deaths over the last decade is largely attributed to the rise in fentanyl distributed through drug cartels, a startling number can be traced to prescriptions. In fact, the Centers for Disease Control and Prevention estimates that 45 people died each day in 2021 from a prescription opioid overdose — about one-fifth of all opioid-related deaths.
When towns lose bowling alleys or movie theaters or libraries, they lose a safety net in the battle against addiction.
Some efforts to curb opioid prescribing have shown promise, including prescription drug monitoring programs, promotion of alternative analgesics, provider education and informing prescribing physicians when their patients die from opioid overdoses. But there is one medical specialty for which opioids are still a crucial part of most patients’ treatment plan: surgery. Nearly every patient discharged after surgery leaves the hospital in significant pain, which is why surgeons prescribe more opioids than almost any other specialty.
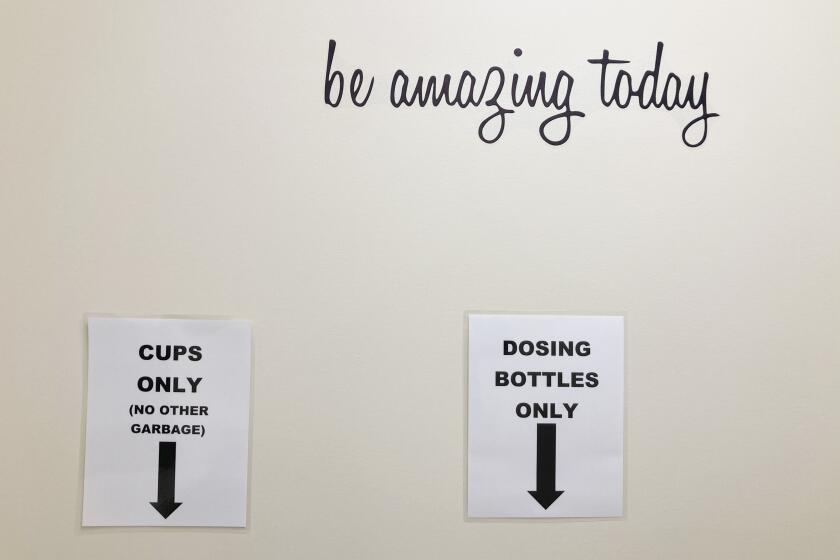
The FDA just made access to Narcan easier to stop overdose deaths. Methadone also should be made more widely available to treat addiction.
Most patients, however, do not use all the opioids they are prescribed after an operation. That leaves excess pills in circulation and helps fuel the epidemic. If we could get surgeons to prescribe only the number of pills patients need for their own use, this could greatly reduce the number of excess pills available for diversion and misuse, among patients, their families and members of their communities. This, in turn, could reduce addiction and overdoses.
Minimizing how often a surgery patient ends up with extra opioids would not solve the crisis, but it’s part of the solution — and it’s achievable.
Experience during the pandemic shows the value of increased access to care and prescriptions, both in preventing and treating substance abuse.
Changing prescribers’ behavior is hard. They get set in their ways, moored by a strong belief that what they are doing is best for their patients. Moreover, they strenuously resist attempts to constrain their freedom to decide what is best. Our research team looked to behavioral science for ways to nudge providers to prescribe in accordance with best practices, while leaving them with full autonomy to choose what they think would be best.
Conventional strategies for curbing excessive opioid prescribing assume that surgeons are rational actors who, whenever they are informed about patient needs and incentivized to attend to them, will act to maximize the welfare of patients. If that were the case, simply educating doctors about the dangers of overprescribing might be sufficient.
However, numerous studies from experimental psychology and behavioral economics have shown that people are highly selective in the information they focus on and more socially minded than traditional models of rational self-interest would predict.
Such insights from behavioral science provide promising avenues for curtailing excessive opioid prescribing by surgeons. For instance, one group of researchers found that setting the default opioid quantity in the electronic health record system to match the amount patients actually use substantially reduces the amount of opioids prescribed. Apparently, busy surgeons tended to go with the flow when prescribing — presumably because the default number of pills became a salient reference point, was easiest to enter and suggested a norm of correct behavior.
Surgeons, like other humans, are social animals who are strongly motivated to adhere to the norms of good behavior endorsed by their peers. We capitalized on this for our recent study, a randomized trial to test two simple interventions across 19 hospitals in Northern California for a year.
In one version, the emails informed surgeons that they had prescribed more pills than other surgeons in their health system had been prescribing for the same procedure. This message highlighted “descriptive” norms of actual behavior. In a second, simpler version, whenever a surgeon prescribed opioid amounts that exceeded recommended quantities for the procedure they had performed, we sent the doctor an email notification informing them. This intervention highlighted “injunctive” norms of ideal behavior.
Surprisingly, both social norm interventions had the exact same impact on prescribing. Subsequent patients were about 25% less likely to receive an opioid prescription that exceeded the recommended amount. This resulted in about 42,000 fewer pills in the community for the 26,000 patients who were part of the intervention group.
Imagine how many fewer pills would be prescribed if this were scaled up nationwide, given that there are more than 50 million inpatient surgical procedures performed each year in the U.S. Surely this would lead to millions, if not tens of millions, fewer opioid pills circulating in the U.S. each year.
Inexpensive solutions grounded in evidence on human behavior can be powerful tools in our campaign against opioid addiction. Sometimes just a light touch — a tweak to the default settings in the electronic health system or an automated email to surgeons — can have an outsize effect on prescribing decisions with life-or-death consequences.
Zachary Wagner is a health economist at USC and Rand. Craig R. Fox is a professor of psychology and medicine at UCLA and chair of the Behavioral Decision Making Area at the UCLA Anderson School of Management.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.