Op-Ed: Hard lessons we learned from the COVID-19 tragedy at San Quentin prison

San Quentin State Prison has been no match for the coronavirus. Of the nearly 3,200 incarcerated individuals, 2,237 have been infected, more than 100 have been hospitalized, and 26 have died.
As we stand over the rubble of this public health disaster, still stunned by the events of the past three months, we are compelled to give our account as front-line physicians and offer some hard-earned lessons for preventing similar outbreaks in correctional facilities.
On May 28, we were informed that the state Department of Corrections would transfer 121 inmates from the state prison in Chino, the facility with the largest coronavirus outbreak at the time, to San Quentin. The intent was to move uninfected vulnerable people out of harm’s way and to a safer setting. However, a move this size, on two days’ notice, involving older people with serious medical conditions and during a global pandemic, struck us as profoundly ill-advised.
San Quentin is the oldest prison in California’s overcrowded system. Many buildings date from the turn of the 20th century. Our patients are often housed two people to a 6-foot-by-10-foot cell with barred doors in five-tier blocks. This degree of overcrowding is the main reason 16 of the 17 largest coronavirus outbreaks in the country have been in correctional institutions. San Quentin has the largest cluster of all.
Our careful efforts to avoid such a catastrophic outbreak, put in place in March, were upended by the transfer from Chino. We had developed plans with the prison’s correctional staff to test, surveil, isolate, quarantine, triage and treat our patients.
We advocated for the basics of infection control — masks, soap and water, and staggered yard times. Visitations, volunteer programs and county jail transfers were all eventually suspended. We were judicious when approving offsite visits to specialty care for our patients. By May 28, there were six reported coronavirus cases among the staff, but none among the prison population.
Then the buses from Chino arrived. We soon discovered many of the people transferred had not been tested for several weeks before departure. Some had symptoms upon arrival. Ideally, those transferred would have been moved into an isolated housing unit with their own dedicated staff for at least 14 days. But there was no such space in our overcrowded institution and no time to empty out a housing unit and rearrange staff assignments.
Instead, the new arrivals were placed in cells that had bars rather than solid doors on the fourth and fifth floors of a poorly ventilated housing unit. The virus spread easily through the air and via staff movement between buildings. Once the virus took hold, its transmission was swift and widespread.
As the virus engulfed the facility, many of those incarcerated at San Quentin opted out of testing and even declined to participate in routine monitoring or divulge COVID-19-like symptoms because they feared that medical isolation would result in solitary confinement.
As the number of infections spiraled out of control, we moved quickly to try to mitigate the harm, assessing and treating hundreds of patients a day with limited staff and resources. Still, the amount of suffering, sickness and death has been staggering.
Before the outbreak, two or three medical emergencies would occur on a given day; during the worst of the crisis, there were as many as 20 a day. Support has arrived in the form of housing tents, a field hospital and staff. But that help, while appreciated, came weeks past the outbreak’s peak.
Many of us — physicians, nurses and correctional staff — have worked more than 80 hours per week during this outbreak. We have shared the fear and anger of our patients while attempting to uphold their constitutional right against cruel and unusual punishment — in this case, preventable illness from a deadly virus.
As the pandemic rages on in this country, the virus will continue to infiltrate and thrive in correctional institutions. San Quentin’s COVID-19 experience lays bare the injustices of our correctional system and the vulnerabilities of incarcerated people. But there are sensible ways to prevent this from happening elsewhere.
First, and most important, we have to further reduce the population in overcrowded prisons and jails to below capacity. This could be done safely by minimizing new incarcerations, releasing those within months of parole or imprisoned on technical charges, and expanding the use of compassionate release for people who are frail and at high medical risk. In Norway, where prison populations have been reduced significantly, coronavirus-related deaths in custody have been almost nonexistent.
Second, it is imperative that corrections officials make decisions during a pandemic in partnership with experts in infection control, epidemiology and public health. We need to give local public health officials the jurisdictional breadth and authority to take all necessary measures to protect the health of correctional populations. These local leaders should be supported by regional command centers that can provide additional staffing, isolation housing, rapid testing and data management immediately in the event of an outbreak.
Finally, the system needs to listen to the people living within its walls. Those perspectives and experiences will give us better insight into our missteps. A detailed analysis of the San Quentin outbreak and rigorous preparation going forward are the only ways to rebuild our patients’ trust.
We cannot protect our patients, the staff and the surrounding communities without systemic accountability and change. It is time to put health first. The only thing worse than the San Quentin tragedy would be to not learn from it.
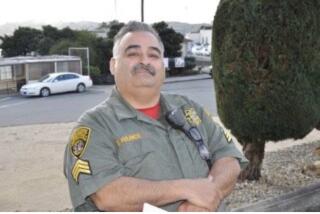
Haiyan Ramirez Batlle is an internist at San Quentin. John Grant is a family physician at San Quentin. George Beatty and Laura Collins, both physicians at San Quentin, also contributed to this article. They are all members of the Public Policy Committee of the Union of American Physicians and Dentists.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.