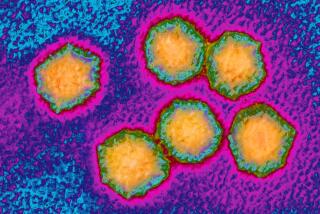
How San Diego’s hepatitis A outbreak became the worst the U.S. has seen in decades
Experts say San Diego took all the right steps in addressing what is now one of the largest hepatitis A outbreaks the country has seen in decades, but variables unique to the city’s situation contributed to the outbreak.
At least 481 people have been infected and 17 have died of the infection since November in San Diego. Another 88 cases have been identified in Santa Cruz and Los Angeles counties, where hepatitis A outbreaks have been declared.
Officials throughout the state are now scrambling to vaccinate homeless populations, which are considered the most at risk. Doctors say people who have already been infected could travel and unknowingly spread it elsewhere.
Dr. Janet Haas, president-elect of the Assn. for Professionals in Infection Control and Epidemiology, said the outbreak is unusual for the U.S. because the spread of the liver infection has been blamed on a lack of basic hygiene and sanitation, not contaminated food.
This means public health officials can’t solely rely on previous containment methods.
“It’s not like there’s never been a hepatitis A outbreak before…. We know what’s worked in the past. Usually that contains it and the story ends,” Haas said. “But sometimes it doesn’t work, or circumstances are different and you have to ramp it up.”
In San Diego, where nearly 85% of all confirmed cases are located, cleaning crews are hitting the streets, attacking them with high-pressure water mixed with bleach in an effort to sanitize any surfaces contaminated with feces, blood or other bodily fluids.
A private company was hired in September to deliver portable hand-washing stations in locations where homeless residents tend to congregate.
Despite these efforts, the disease is spreading and many are asking what could have been done and what will effectively prevent future transmission.
According to Dr. Monique Foster of the Centers for Disease Control and Prevention’s division of viral hepatitis — in San Diego this last week for a national infectious disease conference — there is no national standard that outlines how every public agency should respond.
“You can’t have a checklist that says ‘do x, y and z,’ because no outbreak is the same,” Foster said following an impromptu session at the conference about San Diego’s outbreak. “The type of illness, the group of people it’s affecting and how it’s being spread are all factors that will impact how a government should respond and when the public should be notified.”
For example, San Diego’s problem looks similar to a hepatitis A outbreak in Michigan, where state health officials have confirmed at least 341 cases since August 2016. Of those, 268 people have been hospitalized and 14 died.
But Michigan and San Diego have different resources, Foster said. The underlying populations being affected are different and the laws in both areas are different.
“This is why the CDC assists. We connect them with people who have answers, but we don’t come in and take over,” Foster said. “The local governments and local health departments are the first in line because they know their needs better than we do.”
The California Code of Regulations outlines reporting procedures for hepatitis A cases among a specific class of people, including daycare workers, healthcare facilities and food handlers who are more likely to spread the liver disease to other people.
County health officials have been hesitant to release any additional information about where the cases are specifically concentrated, citing state and federal health privacy laws.
“This information is gathered from confidential medical interviews and documents,” Eric McDonald, director of the county’s epidemiology and immunization services branch, said after presenting with Foster at the infectious disease conference. “The public’s need to know has to override the confidentiality of the infected individuals.”
According to Dr. Oscar Alleyne, senior public health advisor to the National Assn. of County and City Health Officials, the Control of Communicable Diseases Manual is often referred to as the “bible” among health officials.
The American Public Health Assn. lists the book, which is now in its 20th edition, as a “must-have sourcebook on identifying and controlling infectious diseases.”
Alleyne said it’s the closest thing to a guidebook public officials have and has been an industry standard reference for more than 100 years.
According to the manual, prevention is key for hepatitis A, since the vaccine provides lifelong immunity. Data show since being added in 2006 to the recommended list of vaccinations for young children, the number of hepatitis A cases in the United States has decreased by 95%. Officials are instructed to control patients confirmed to have hepatitis A and quickly vaccinate those in immediate contact with infected individuals to increase the likelihood that the vaccine will be effective.
County epidemiologists identified the rash of hepatitis A cases in early March, and dated the infection to the previous November. From the outset, the priorities have been vaccination and education, in line with manual instructions.
It’s easier said than done.
“The normal method for preventing other people from getting sick gets thrown out the door when the community it’s infecting lives outside,” Alleyne said. “You have to know where they went, who they came in contact with…. The likelihood of being able to capture everyone on that list is small.”
In the event of an outbreak, public health officials should first determine how hepatitis is being spread, vaccinate the at-risk community and make special efforts to improve sanitary and hygienic practices to eliminate fecal contamination, the manual says.
By early summer the official focus shifted to sanitation — hand washing and street cleaning.
According to Dr. Jeffrey Engel, executive director of the Council of State and Territorial Epidemiologists, that might not be enough.
“I can tell you that washing the doorknobs is not going to do it,” Engel said. “This is more about human behavior than anything else.”
Hepatitis A is more commonly transmitted through contaminated food. In 2003, 935 people in multiple states were infected by eating contaminated green onions at a restaurant. It was the largest outbreak since 1998, according to the Centers for Disease Control and Prevention. No one died.
Lauryn Schroeder writes for the San Diego Union-Tribune.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.