Growing need. Glaring gaps. Why mental health care can be a struggle for autistic youth

In April, a group of Orange County parents flew to Sacramento to attend a conference hosted by Disability Voices United, an advocacy group for people with disabilities and their families.
They wanted to emphasize three issues to state officials at the event: the paucity of mental health care for children with developmental disabilities, the confusing mess of government systems meant to help them, and the gaps in availability of day-to-day caregiving.
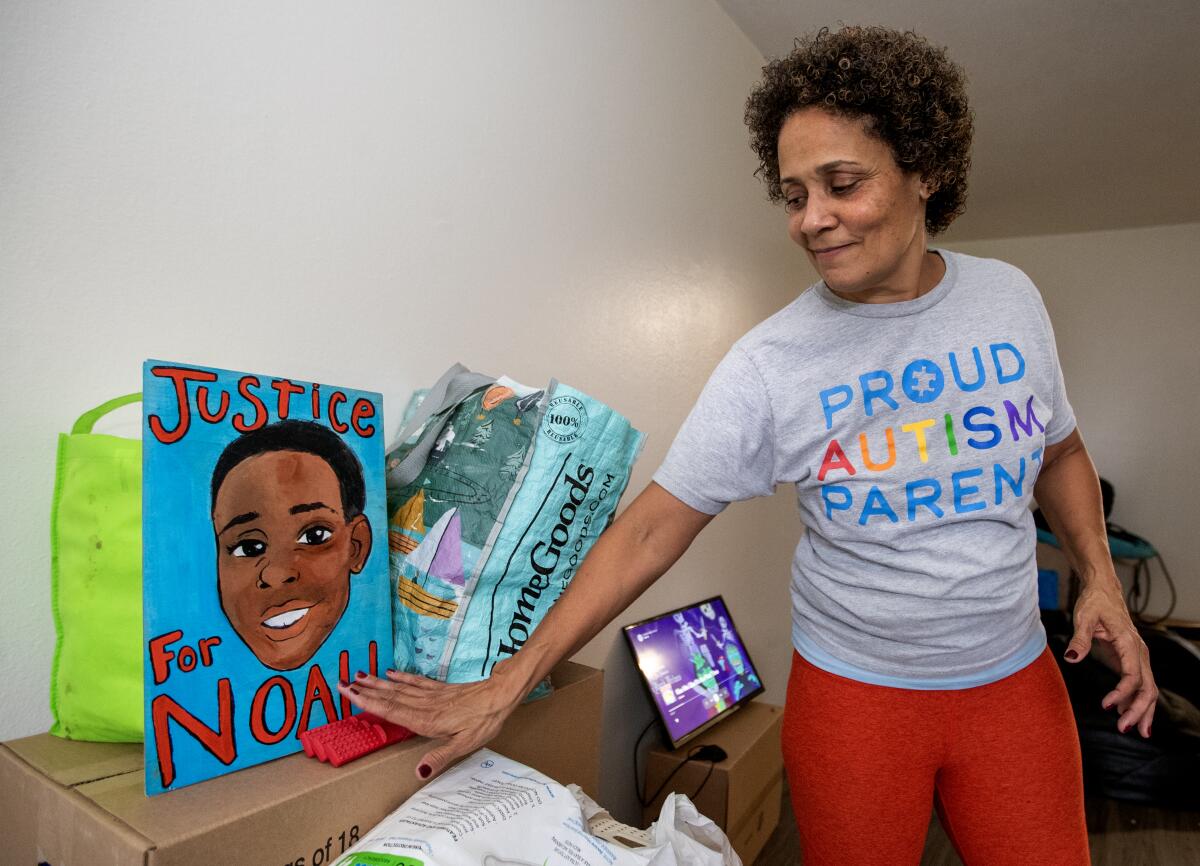
Among them was Christine LyBurtus, a single mom living in Fullerton. Last fall, after repeated rounds of 911 calls and emergency hospitalizations, she had made the agonizing decision to move her son, Noah, who is autistic, into a state-operated facility for at least a year.
LyBurtus had struggled to find the support she needed to keep him at home. “Families are being forced to give up their children to group homes and treatment centers over 12 hours from their homes ... or out of the state of California entirely,” she told the crowd at the conference.

“I beg you to hear us,” she said to state officials before turning from the microphone.
Despite the growing diagnosis of autism, which has been estimated to affect more than 2 million children and teens across the country, experts and advocates have bemoaned glaring gaps in services to meet the mental health needs of autistic youth.
Some researchers have estimated that upward of 90% of autistic youth have overlapping conditions like anxiety, depression or ADHD. Many have suffered alarming levels of trauma.
Yet “there are very few specialized facilities in the country that meet the unique needs of individuals with autism and co-occurring mental health conditions,” especially in crisis situations, said Cynthia Martin, senior clinical psychologist at the Child Mind Institute, which is based in New York.
‘I don’t want him to go’: An autistic teen and his family face stark choices
Between 2020 and 2021, the number of California children and teens served by the state developmental disability system who were deemed to have “complex needs” — a state term for those who needed a range of crisis services or landed in a locked psychiatric ward — rose from 536 to 677, according to a report released last year by the California Department of Developmental Services.
California has been working to build more facilities to house and support such youth, including STAR homes that provide “crisis stabilization” for roughly a year, like the one into which Noah moved. But the state has seen an uptick in the number of people in need of such programs, as well as more former residents boomeranging back for “further stabilization,” the state report said.
As of this summer, the STAR homes could accommodate only 15 teens across the state; the one that accepted Noah budgets for more than $1 million per resident annually.
There are other community facilities where developmentally disabled youth in crisis can be placed, but “there remains a critical need for a ‘can’t say no’ option for individuals whom private sector vendors cannot or will not serve,” the state report concluded.
Autistic people and their families have also lamented that they cannot find adequate help in their communities before they reach a crisis point. Researchers have found that mental health workers are often unprepared to work with people with intellectual or developmental disabilities or may chalk up symptoms to their disabilities, rather than overlapping needs.
“It’s pretty common for a mental health practitioner to turn away someone with a developmental disability or say, ‘I don’t serve that population,’” said Zoe Gross, director of advocacy for the Autistic Self Advocacy Network.
Alison D. Morantz, director of the Stanford Intellectual and Developmental Disabilities Law and Policy Project, called it a “scandal” that amid a scarcity of psychiatric beds for youth, “if a family member discloses that their child is on the autistic spectrum, they can say, ‘No thank you.’”
“It puts parents in impossible situations,” she said.
The biggest challenges for many families of autistic youth often surround aggression, which isn’t a core feature of autism, but the symptom of other issues that need to be uncovered, child and adolescent psychiatrist Dr. Matthew Siegel told a federal committee last year.
“You have to look underneath or in front of that … for what could be contributing or what is driving this aggression,” said Siegel, founder of the Autism and Developmental Disorders Inpatient Research Collaborative. He and other researchers have seen promising results from specialized units at hospitals, but few exist — “not even one per state.”
“Even specialized clinics that can work on these challenges are quite rare,” he said.
The Supreme Court has ruled that institutionalizing people with disabilities who could live in the community is discriminatory if a community placement “can be reasonably accommodated.” Federal investigations have, at times, faulted states for failing to provide needed services for people to stay in their homes or communities.
The law “requires that services are provided in the most integrated setting appropriate to the needs of a person with a disability,” according to the U.S. Department of Health and Human Services.
But the struggle to find needed services can end up pushing autistic people with mental health needs out of their communities. Bonnie Ivers, director of clinical services for the Regional Center of Orange County, said last year that “more and more families are having to review options that are outside of our county.”
Some Californians even go outside the state: As of June 2022, there were 49 youth with “complex needs” getting services outside of California, and an additional 33 “at risk of being referred to out-of-state resources,” according to the developmental services department.
In the following year, that number grew to 57 youth out of state — and an additional 64 who might be at risk of joining them. The numbers may actually be higher: The state agency says it learns about out-of-state placements only when families inform the regional centers that coordinate developmental disability services.
Nancy Bargmann, director of the California Department of Developmental Services, said their goal is to provide “a continuum of supports” so that families “don’t need to make that really hard decision of having their child not live at home.”
California has launched more than a dozen teams focused on crisis prevention, called START teams, which it says have helped keep people in their homes. Their services include connecting different systems that assist families, such as mental health providers and disability services.
But they do not yet exist everywhere in the state. California also has mobile “Crisis Assessment Stabilization Teams” — or CAST — that are meant for people who have exhausted other kinds of help or are at risk of having to move into more restrictive settings. There were three of them as of this spring, according to the developmental services department.
Judy Mark, president of the advocacy group Disability Voices United, argued it is counterproductive to try to stabilize a child away from his or her family. If at all possible, she said, California should be ensuring constant support in the home, which she argued would also be less costly than caring for a child in a STAR facility.
But disability services providers say that getting such caregivers has continued to be a challenge, with state rates for such workers outstripped by what they can earn elsewhere. Increases in those provider rates have been slowly phased in over time, with the next bump slated for January.
In many cases, “what you’d want to see is somebody, 24 hours a day, in the home helping the parent,” said Larry Landauer, executive director of the Regional Center of Orange County. But “that’s where we have been just drastically short on staffing.”
All the gaps in the system can come to a head when young people with developmental disabilities hit puberty, especially if they face “the inability to communicate in such a complex and confusing time,” said California Commission on Disability Access member Hector Ramírez, who is autistic and lives in the San Fernando Valley.
If autistic teens and their families cannot get the support they need, Ramírez said, it “has compounding consequences that result in people just getting worse — when they shouldn’t be getting worse.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.











