Hospital medication errors left SoCal patients at risk. One suffered a brain bleed

State regulators faulted two hospitals in Southern California for medication errors that put patients at risk, including an elderly patient who suffered a brain bleed after receiving repeated doses of blood thinner.
At Adventist Health Simi Valley, medical staff erroneously gave an 81-year-old patient two doses of the blood thinner Lovenox within two hours, which “probably caused” a brain bleed that preceded the patient’s death in March, investigators with the California Department of Public Health found.
State investigators determined that the medication error represented a “system wide failure” and may have led to the death, which occurred 18 hours after the brain bleed.
The hospital “failed to ensure that patients had been protected from medication errors,” they found, declaring its faulty practices an “immediate jeopardy” situation that put patients at risk of serious harm.
Adventist Health Simi Valley said in a statement that the state agency had undertaken the review after the hospital reported the medication error to regulators, and that concerns identified by the state team were “immediately addressed.”
“First and most importantly, we send our sympathies to the family,” the hospital said in its statement. “Patient safety is always our No. 1 priority.”
California Hospital Medical Center failed to recognize signs that the patient was bleeding internally, according to the state Department of Public Health.
State health officials found that physician orders for medications were not properly followed at the hospital, not only for the 81-year-old who died but also for another patient receiving intravenous medication, which may have “adversely affected” their blood pressure.
In the first case, the two doses of blood thinner were verified by two pharmacies — a corporate pharmacy for the hospital system in Roseville, Calif., accessed via telehealth and a pharmacy in Simi Valley — but the two “never talked with each other after verifying each of these two doses.”
Although nurses said they typically communicate with one another about medication, one appeared to be unaware that the patient had gotten an earlier dose, telling state investigators: “If I knew about the previous 60 mg dose of Lovenox then I would not have given another 40 mg dose of Lovenox ... It would have been too soon.”
And neither of the doses was correct. Both of them should have been reduced based on the patient’s kidney function “rather than rounding these doses up, as was done,” the investigators found.
The hospital also failed to make sure that oral doses of medications had correct expiration dates and were checked by a pharmacist before being given to patients. Such lapses could put patients at risk of receiving “ineffective, incorrectly prepared, or outdated medications,” according to the state findings.
Medications used for sedation and asthma relief, among others, were not properly administered or documented for several patients at the facility, the state found. In addition, the hospital had left “very old” medications such as “cocaine solution” on its list of drugs covered for patients, despite the existence of better and safer substitutes.
State officials removed the “immediate jeopardy” label in May, shortly after Adventist Health Simi Valley presented a plan that included pharmacy alerts for certain medications and random observations in each unit to verify that medications are being given in the right doses at the right times.
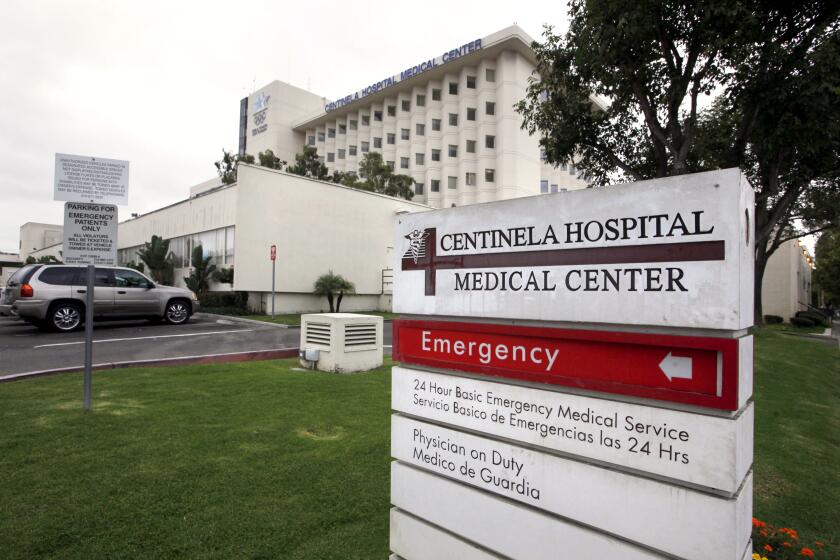
California regulators have fined Centinela Hospital Medical Center $75,000 for ‘deficient practices’ that led to the death of a patient admitted for labor and delivery.
California investigators also found “deficient practices” at Northridge Hospital Medical Center, where a patient had to be resuscitated after being given the wrong medication during a hospitalization in February.
The state Department of Public Health found that the patient, who was recovering from anesthesia after an operation, was given a blood pressure medication instead of naloxone, which is used to reverse the effects of opioids. The hospital also failed to assess the patient every five minutes while anesthesia was being administered, as required by its own policies, the state investigation found.
Investigators also found that nursing staff failed to regularly check the “crash cart” — a movable, locking unit that stores emergency drugs and supplies — to make sure that needed items were readily available for patients, according to a report on their findings.
Like the Simi Valley hospital, Northridge Hospital Medical Center was also found to be in an “immediate jeopardy” situation, a designation that was lifted in May after it submitted a plan to address the issues.
Northridge Hospital Medical Center, which is part of the Dignity Health system, said in a statement that it had reported the incident itself, “conducted a thorough review and worked closely with the medical staff, patient care staff, as well as with the Department of Public Health, to ensure that an incident like this does not happen again.”
“At Northridge Hospital Medical Center, there is no higher priority than the safety and well-being of our patients and staff,” the hospital said.
Both of the state reviews were authorized by the Centers for Medicare & Medicaid Services, a federal agency, to determine whether the hospitals were following specific rules for participating in federal programs such as Medicare. The agency did not immediately provide comment on whether the hospitals faced any fines connected to the findings.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.