Tens of thousands of L.A. County residents could soon lose Medi-Cal coverage. Here’s why
Tens of thousands of people in Los Angeles County could lose their Medi-Cal coverage in July, according to preliminary data provided to a health plan that serves Angelenos on the public program.
L.A. Care, a publicly operated health plan in L.A. County, said that early data provided by the state indicate that roughly 40,000 of its members enrolled in Medi-Cal could lose their coverage this month, although final numbers are still pending.
Those figures do not include Medi-Cal recipients who are not covered by L.A. Care, which serves roughly 2.7 million of the nearly 4.7 million people in L.A. County who were enrolled in Medi-Cal as of this spring, according to state figures. The numbers are expected to keep shifting as more people return paperwork that was due Friday to renew their coverage in California’s Medicaid program, the beginning of a process that will play out over the next year.
But the tentative figures are an early sign of the serious shift underway as the federal government has rolled back rules that helped people stay on Medicaid, one that has troubled health providers and advocates who fear many patients will unnecessarily lose medical coverage for which they qualify.
“Losing Medi-Cal coverage is not a mere inconvenience or annoyance,” said David Kane, an attorney at the Western Center on Law & Poverty. “For far too many it can be life-threatening. It can mean that transportation to dialysis does not show up. Surgery is canceled. You cannot pick up your prescription drugs.”
Earlier in the pandemic, federal rules had prevented states from booting people from their Medicaid programs, allowing people to hang onto coverage without turning in paperwork to prove they were still eligible.
By late June, the rollback of those rules had pushed more than 1.5 million people off Medicaid across the country, according to a KFF analysis. Some may have started earning too much money to qualify for Medicaid, but many were stripped of their coverage for “procedural reasons” such as not turning in paperwork on time, raising alarm that eligible patients could be losing their health benefits because of missed mail or other bureaucratic hang-ups.
When that happens, it’s “not because the state has affirmatively validated that that individual or kids or family is over income,” but rather due to “red tape” such as a family not responding to a renewal notice, which “could be because their contact information was outdated — they moved three times since the start of the pandemic,” said Daniel Tsai, deputy administrator at the federal Centers for Medicare & Medicaid Services.
California will soon require Medi-Cal recipients to prove their eligibility again. But it has a safety net for people who lose their coverage.
“So we have been both pressing and urging every state ... to really do everything in their power to help keep people covered,” Tsai told reporters.
California, which had more than 15 million people in its Medi-Cal programs as of this spring, is starting to eject people in July, later than in many other states. More people are expected to lose their coverage over the next year, as a new round of cases comes up for reassessment each month.
In Orange County, the CalOptima Health plan said that more than 10,000 of the 46,000 members whose paperwork was due back by the end of June had not returned it by early Friday, putting those Medi-Cal enrollees at risk of losing their coverage in July. Such patients would still have a chance to renew their coverage within 90 days and get retroactive coverage to July, according to a CalOptima Health spokesperson.
In L.A. County, nearly 180,000 renewals were due back to county officials by the end of June, according to its Department of Public Social Services. More than 53,000 cases were automatically renewed as L.A. County checked information against a federal database for other government programs, but roughly 126,000 households were mailed packets and had to provide information by the end of the month, according to the county department.
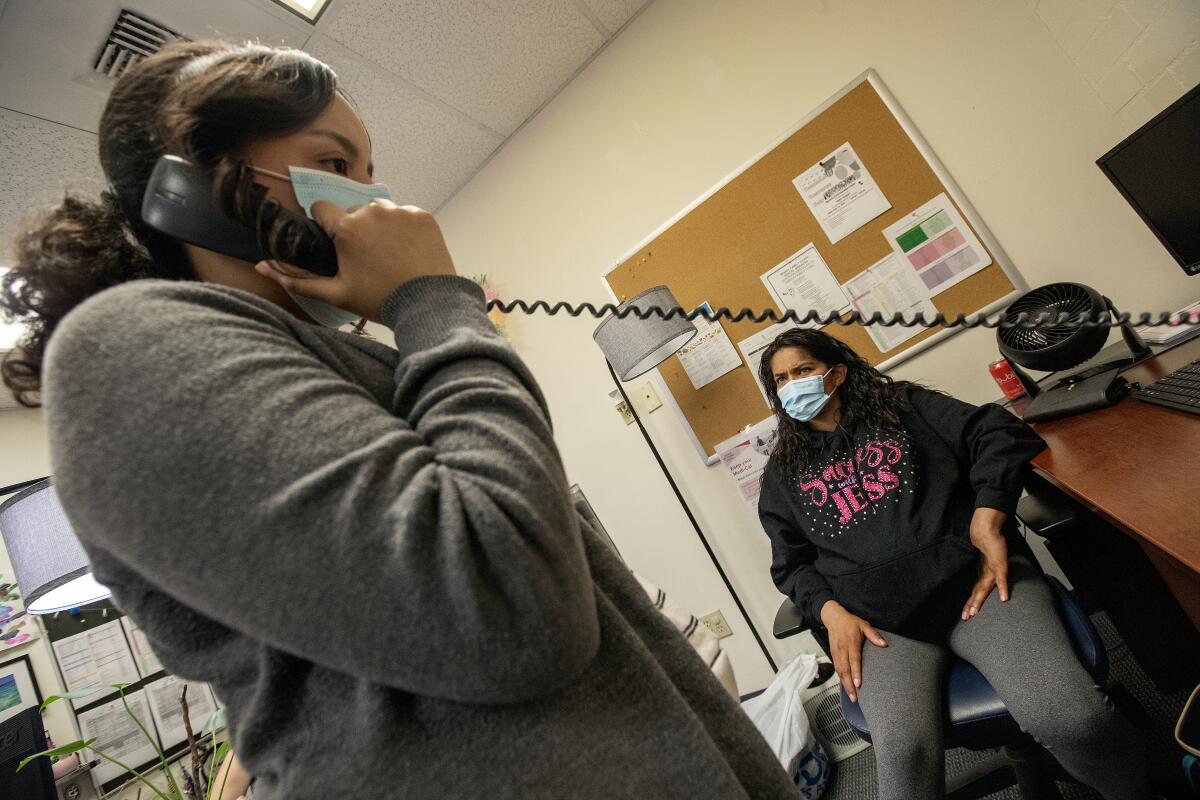
L.A. County officials said they would not have data on the total number of local households losing their Medi-Cal coverage in July until the middle of the month. Community groups have raised concerns about whether L.A. County is prepared for the deluge of renewals that it will need to process over the next year, especially with Angelenos already facing long waits for help when they dial the county for assistance with Medi-Cal.
Kane said he was especially alarmed that across the state, some people who have filled out, scanned and uploaded paperwork to a state website have still gotten mail warning them they will lose their Medi-Cal, raising concerns that people could be disenrolled despite turning in their information on time.
“It’s critical that counties process every piece of information that comes in, because that is what is needed to keep people covered,” Kane said.
L.A. Care projects that 13% of its Medi-Cal members will lose their coverage over the coming year. Government agencies and community groups have worked to alert people that the process is underway and ensure that people ejected from Medi-Cal obtain other health coverage.
As the health plan has started to get tentative figures for how many people could be disenrolled in July, “I’m somewhat relieved that it wasn’t bigger,” said John Baackes, chief executive of L.A. Care. Baackes credited automatic renewals for sparing many families from having to fill out and return paperwork.
But the numbers nonetheless leave him concerned. “Some of those people who didn’t complete the process need the coverage — and they won’t discover it until they go to fill a prescription or go for a doctor’s appointment,” Baackes said.
Some may realize that quickly enough to try to retroactively reinstate their coverage within the 90-day window, Baackes said, but others will “have to start all over again.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.