In the emergency department at MLK Community Hospital, masked patients lay in wheeled stretchers lining the hallways.
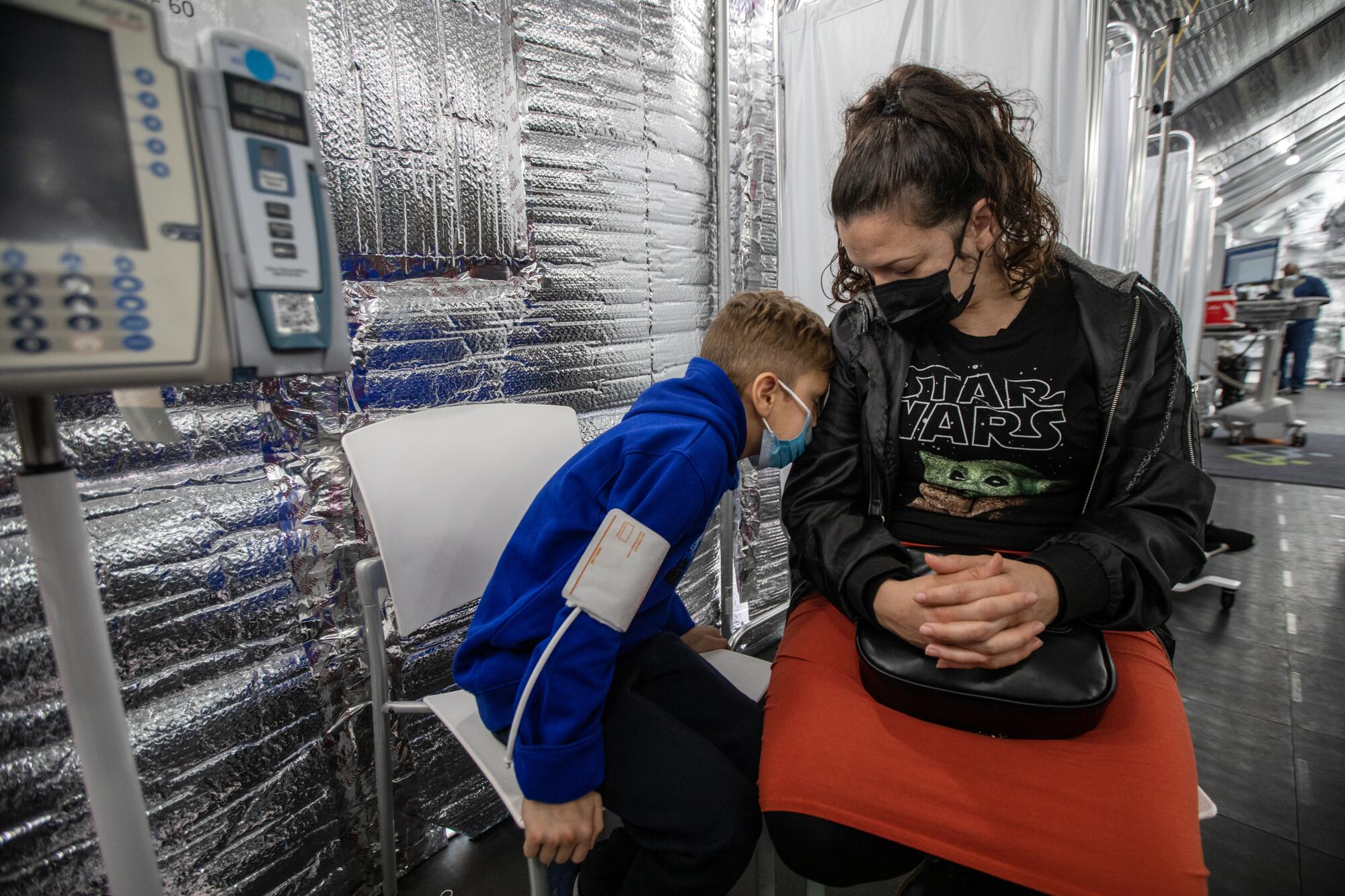
Others slumped in chairs where nurses attended to them. Amid the crush of people on a recent day in December, only the sickest or most severely injured got one of the 29 rooms.
The rise of flu, RSV, COVID and other winter viruses has exacerbated overcrowding that existed even before the pandemic, hospital officials said — the result of stark shortages in medical care in a low-income South Los Angeles neighborhood where most residents are Black or Latino.

Patients come to MLK’s emergency department with minor ailments they haven’t been able to get treated elsewhere, or more serious conditions that have become dire in the absence of care to prevent or manage them, said Dr. Elaine Batchlor, chief executive of MLK Community Healthcare.
When it opened seven and a half years ago, MLK’s emergency department was expected to handle 110 patients a day, or roughly 40,000 patients annually. Last year, more than 400 patients arrived on especially hectic days, for an annual total of more than 112,000 patients.
“We kind of put patients everywhere we could.”
— Dr. Elaine Batchlor, chief executive of MLK Community Healthcare.
Earlier in the pandemic, the crowds at the emergency department had dissipated as some people stayed away. But now, as fears of catching COVID have lessened, the number of people seeking care at the emergency department has surged again, exceeding pre-pandemic levels, Batchlor said.
As Batchlor walked through the emergency department, she gestured to an area full of chairs and cubicles. “This used to be the waiting room, but it is completely converted into treatment space,” she said.

In all, MLK has carved out more than 200 areas for patients to be treated, including the 29 traditional rooms and an unconventional range of spots in chairs, gurneys and under tents. Beds occupy what was once the gift shop. Ambulance bays hold tents for assessing and treating patients.
“We kind of put patients everywhere we could,” Batchlor said.
Nurses try to keep their voices low when speaking to patients seated between dividers in an effort to respect privacy, competing with the sounds of crying children and coughing.
In a period of less than three weeks this winter, the hospital asked 101 times to divert emergency vehicles to other medical facilities because it was full, according to Gwen Driscoll, vice president of strategic communications at MLK Community Healthcare.

Many patients have chronic illnesses — such as diabetes and heart disease — that could be managed at a doctor’s office, but “there aren’t enough doctors and there isn’t enough access in the community,” Batchlor said.
About 40% of MLK’s emergency visits could have been handled in an outpatient clinic, the hospital has estimated.
“You would never see that in areas that have more resources.”
— Dr. Oscar Casillas, MLK’s medical director of emergency medicine
Dr. Oscar Casillas, MLK’s medical director of emergency medicine, said a pregnant woman recently came in needing an ultrasound because the clinic she had visited couldn’t provide it. Others have an appointment scheduled elsewhere, but not for months, “for something that’s been bothering them for four or five weeks” already, Casillas said.
And some clinics send their patients to the ER for routine electrocardiograms to get cleared for surgery, he said.

“You would never see that in areas that have more resources,” Casillas said.
South L.A. needs 1,400 more doctors, including both primary care physicians and specialists, the hospital estimated in a recent report. The area served by MLK has been designated by federal agencies as a “shortage area” for health professionals.
More than three-quarters of patients in MLK’s emergency department rely on Medi-Cal — the California Medicaid program — and roughly 10% are uninsured, according to hospital figures.
Medicaid programs reimburse doctors at lower rates than private insurers, which can “reduce the number of providers that are willing to participate,” said Nadereh Pourat, associate director of the UCLA Center for Health Policy Research.
Batchlor argues that those financial incentives are at the root of the problems that MLK patients face in getting day-to-day care. Medi-Cal recipients were more likely than people who get insurance through their employer to say that they have no usual source of care or that a doctor would not accept their insurance, according to a report from the UCLA Center for Health Policy Research.

Some patients turn up at the MLK emergency department in need of things as simple as a medication refill.
On a rainy Tuesday, Mary Johnson came to get medicine for pain and to help her with breathing — a visit she makes every few months, she said.
Johnson said she has no primary care doctor.
“It’s so difficult right now with all of the COVID,” said Johnson, 57, who is unhoused and has been sleeping in a car.
Besides, she loves MLK.

“Whatever issue, they always take care of me,” she said. “And I know they’re going to move me out of here so fast.”
Batchlor said that patients with less serious problems are “in and out very quickly.”
“And the way they do that is by seeing the patients wherever they are,” she said — be it in a chair or a gurney or under a tent set up outside.
The crowds at the emergency department show the extreme need in the community but are also a sign to hospital staff that they are doing things right.

“That’s the success of the work that we’re doing here,” said assistant nurse manager Jesse Lynwood. “That the community is showing up.”
Batchlor and Casillas have also grown concerned about psychiatric patients being brought to the emergency department from beyond South L.A. Hospital officials say that such patients have been dropped off by police departments serving areas as far away as Santa Monica, Whittier and Huntington Beach.
A report requested by L.A. County Supervisor Holly Mitchell found that of the psychiatric emergency patients transported by emergency medical services, only a small fraction bypassed a closer hospital for MLK. But the report did not include dropoffs by law enforcement.
At MLK’s emergency department, two tents have been set up for psychiatric patients. On an average day, a dozen patients are awaiting a bed or an evaluation under a short-term involuntary hold known as a 5150, attended by “sitters” assigned by the hospital to stay with them for their safety.

The hospital has no inpatient psychiatric beds, so patients stay in the emergency department, often for days, until staffers can find somewhere else for them to go. The average stay is nearly 35 hours for patients on 5150 holds. One psychiatric patient remained there for 35 days, hospital officials said.
Amid the high demand for its services, the MLK emergency department has been losing tens of millions of dollars annually, Batchlor said, because Medi-Cal reimbursements do not fully cover the costs of care.
In the last budget year, MLK had a net loss of nearly $43 million for patient care in the emergency department — a hole that would be deeper if not for the slim 4% of patients with private insurance, whose care netted more than $6 million in profit, according to figures shared by hospital staff.
A state bill that would have bolstered funding for the MLK emergency department was passed by state legislators but vetoed last year by Gov. Gavin Newsom, who said the money wasn’t included in the budget.
MLK officials said they are again seeking a financial infusion from the state this year. Meanwhile, they are dipping into reserve funds.
“This can only go on so long,” Driscoll said.

Watch L.A. Times Today at 7 p.m. on Spectrum News 1 on Channel 1 or live stream on the Spectrum News App. Palos Verdes Peninsula and Orange County viewers can watch on Cox Systems on channel 99.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.













