Sex pods? Long sleeves? Californians try to cut monkeypox risk while waiting for shots

As Kelechi Kalu books gigs as a musician, he wonders whether he is putting himself at risk for monkeypox.
He finds himself second-guessing how close people are getting to him at bars or music venues. He got nervous when his boyfriend said he had scheduled a massage. He has even avoided trying on clothes when out shopping, worried that the virus could spread on contaminated fabric.
“I haven’t necessarily stopped going out,” said Kalu, a queer man living in West Hollywood, “but I’d be lying if I said that monkeypox wasn’t on my mind 24/7.”
For many Californians — especially gay and bisexual men — worries about the disease have transformed the ways they have fun and connect.
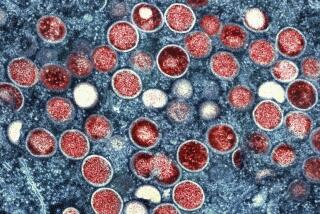
Right now, Kalu is not eligible for a vaccine to combat monkeypox, an infectious disease that can cause painful lesions. The scarcity of vaccines to combat the virus, which has disproportionately hit men who have sex with men, has led health agencies to limit who can get the shots as they await more doses.
So gay and bisexual men, transgender people and others worried about their risk are coming up with practical strategies to protect themselves as they wait for vaccinations. The virus can spread through skin-to-skin contact with lesions, scabs or infected fluids, as well as through contaminated clothing or bedding. Health officials say it can also travel through respiratory droplets.
The gay community is “already under attack from many who’d rather use us as a scapegoat than help us,” Andy Cohen said of the monkeypox outbreak.
The illness is rarely fatal, but can be excruciatingly painful, leave enduring scars, and force people to isolate for weeks. Dr. Kaiyti Duffy, chief medical officer for the Los Angeles LGBT Center, said some patients have suffered lesions that make it agonizing to sit, stand or have a bowel movement. The need to isolate has also forced some patients to “out themselves” to employers, she said.
“The government needs to produce more vaccine and get it in the arms of people who need it — like now,” said Matthew J. Mimiaga, a professor of epidemiology and psychiatry who directs the UCLA Center for LGBTQ+ Advocacy, Research and Health. “But I don’t think gay and bisexual men will let that be the only prevention opportunity that they take.”
As of Thursday, more than 1,300 monkeypox cases had been reported across California, including more than 450 in the Los Angeles and Long Beach areas.
Alarm over the spread of the virus, which prompted emergency declarations from Gov. Gavin Newsom and the Biden administration last week, has spurred many queer men and transgender people to change how they are socializing, celebrating, and seeking love and sex. Some said they were steering clear of crowds or not seeking out new partners.
Much like COVID-19, “the more contacts you have, the more risk you have — and others have — of getting exposed,” said Dan Wohlfeiler, co-founder of Building Healthy Online Communities, a public-private partnership between dating sites and apps and STD and HIV prevention organizations. His group has encouraged people to ask sexual partners if they have had any recent rashes or sores; to get a phone number or other contact information for any hookups to alert them if they were exposed; and to hold off on sex if they feel unwell, among other guidance.
Sexual expression “is a huge part of gay culture and building gay community,” said Ian W. Holloway, a UCLA professor of social welfare and director of its Gay Sexuality and Social Policy Initiative. But “in the face of a pathogen that’s spreading in a way that we haven’t seen before ... it’s not a bad idea to press pause for a period of time. We know the vaccine is on its way.”
Matías Gomez Constenla, a bartender at the Eagle LA, said that people seem to be going out less; some are suggesting leaving shirts on at circuit parties that are normally a bonanza of skin. In San Francisco, writer and activist Race Bannon has noticed that whenever someone comes up and wants a hug, “they’re back to asking me, ‘Are you hugging?’”
At the New Jalisco Bar in downtown Los Angeles, bartender Lorena Garcia lamented that the crowds had dwindled with the latest COVID wave and the added threat of monkeypox. “It has slowed down a bit here at night,” Garcia said in Spanish, as roughly half a dozen men sipped Bud Lights and watched a performer lip-sync to Mexican ballads.
As monkeypox cases across California and the U.S. continue to rise, experts address some of the concerns and questions swirling about virus, and what activities people should consider risky, or not.
Garcia missed the usual tips, but was glad that the regulars were paying attention. “Everyone is definitely aware of the danger,” the bartender said.
And in Palm Springs, an event planner said monkeypox had stirred up confusion in his industry. “Everyone’s asking, ‘What do we do?’ There’s a fear factor around travel,” said the event planner, who asked not to use his full name to avoid hurting his career. “It’s such a destination valley for the gay community and now people are asking, ‘Do I really want to get in that hot tub?’”
Community advocates have come up with practical guides to help sexually active people reduce their risks.
“There’s never been a better time to dress from top to bottom in latex or leather,” the San Francisco AIDS Foundation advised people headed to a kink and fetish festival. The foundation also encouraged people to “consider skipping the dark, back rooms at parties if they’re super crowded and there’s no way to control who you’re bumping up against and rubbing skin-to-skin with.”
Another guide, titled “Six Ways We Can Have Safer Sex in the Time of Monkeypox,” suggested that “it might be time to hang up the group sex and saunas until we all get shots one and two of the vaccine,” framing it as a stopgap measure until there are adequate supplies of the shots.
That guide, written by investigators with the LGBTQ community-led survey RESPND-MI, also suggested “sex pods” to reduce the risk. Those are the sexual equivalent of the insulated groups that people formed early in the COVID pandemic to keep socializing in smaller circles: groups of people who agree only to have sex with other members, after first checking for symptoms.
Grant Roth, one of the investigators with RESPND-MI, said that the most obvious way to protect oneself is to limit or abstain from sex, “but as we know historically, that does not work for a lot of people.”
“If you can’t get the average American to wear a mask to the grocery store, it’s a little myopic to tell gay men that they need to stay home and not have sex for an indefinite number of months” until the vaccine is rolled out, said Dr. Timothy M. Hall, a health sciences assistant clinical professor in UCLA’s Center for Behavioral and Addiction Medicine.
Some are asking: ‘Would monkeypox have received a stronger response if it were not primarily affecting queer folks?’
In Hollywood, marketing consultant Andrew Beaver said he’s not trying to meet new partners online, instead focusing on people he has already met. That makes it easier “to have a conversation about what’s going on,” said Beaver, a 59-year-old gay man. Hooking up with “somebody I just met and meeting in an environment that is darker or there isn’t a lot of pre-conversation ... that is something that, because of where we are right now, I have decided not to do.”
After repeated attempts, he recently got his first shot of the vaccine.
One challenge is that condoms go only so far to thwart a disease that can be spread by lesions all over the body, said Duffy of the Los Angeles LGBT Center. So Duffy said the center has urged people to have honest conversations with sexual partners about any possible exposures. If people are meeting through an app, those conversations can happen before they even meet.
“There is a level of responsibility that we have to ourselves and to our partners,” said Jeffrey C. King, founder and executive director of In the Meantime Men’s Group, which aims to enrich and empower Black gay men of all ages. King, who is gay, said someone he phoned recently told him that they had monkeypox.
That kind of openness needs to happen more, King said, but is often thwarted “because of this whole thing around stigma and shame.” Wohlfeiler noted that even the Centers for Disease Control and Prevention has gotten unusually frank about ways to reduce sexual risk, including suggesting that sexually active people consider touching themselves at a distance from a partner.
“The things that had given us freedom as a community to be sexual” — prophylactic treatments like PrEP to prevent HIV infection — “are not effective in this instance,” said Troy Masters, publisher of the Los Angeles Blade, an LGBTQ newspaper that recently helped host a forum on monkeypox. “So we’re in an odd space of not really understanding what we can do to have sexual expression — unless we’re just very, very cautious and mindful of the person that we’re with.”
Although the virus can spread during sexual encounters, health agencies and community groups have reminded people that other forms of skin-to-skin contact can also pose a risk. The Sacramento LGBT Community Center, which operates shelters for teens and young adults, has also cautioned them against sharing bedding and clothing.
“If I’m playing basketball, or if I’m in a club dancing” with skin-to-skin contact with someone who has lesions, “then I run the risk of contracting it,” said Alexis Sanchez, director of advocacy and training for the Sacramento center. She added that masks can double as a tool to protect against respiratory droplets for both monkeypox and COVID.
Sanchez, like others, said that health agencies and community groups have been walking a tightrope, trying to highlight that queer communities have been disproportionately hit by the rise of monkeypox and need to be targeted for help, while not stigmatizing them or perpetuating the idea that only gay men can contract the disease.
At Precinct, a downtown bar that caters to a more hirsute gay crowd, Chris Reyes and Bobby Cortez were hanging out on the patio after getting vaccinated the previous week. Cortez was glad that public health officials were prioritizing gay men and others at higher risk for vaccines, but expressed frustration that “they’re making it out to be just a gay thing.”
“My co-worker said, ‘You can’t get it if you’re not gay,’” Cortez said. “That’s a huge mistake, that people can think that.”
Eight of the top 10 metro areas searching online for nearby monkeypox vaccines over the last week were in California.
Kalu is in a monogamous relationship, but he worries about getting infected in other ways, including social events with friends. For the West Hollywood resident, who got COVID more than two years ago and has suffered enduring conditions, including nerve pain, the rise of monkeypox cases feels like being pulled back to the beginning of the pandemic.
“Two years later, I’m an anxious asthmatic mess and a new girl is here in town and her name is monkeypox and she’s come to get us,” Kalu said. “I don’t understand why we’re treating this as if we didn’t just go through another pandemic.”
Health and community groups have faulted the slow rollout of vaccines. Tyler TerMeer, chief executive of the San Francisco AIDS Foundation, lamented “the lack of urgency when a public health crisis is impacting the men-who-have-sex-with-men community in our country.” For some, the moment has pernicious echoes not only of COVID but of the beginnings of the AIDS epidemic.
“I’m from a generation which remembers what the stigma of HIV/AIDS was like in the ’80s and ’90s,” said Dorian Wood, 47, a gender-fluid musician who uses the pronouns she and they. Wood said she was the first person vaccinated against monkeypox at the Los Angeles LGBT Center in Hollywood. She was alarmed by government messaging that she felt was “singling us out,” rather than urging everyone to take precautions to avoid the virus.
“It’s infuriating. I feel like we are left, once again, fending for ourselves and taking care of our own,” Wood said.
Duffy said she hopes that the emergency declarations by Newsom and local officials will translate into more resources. “If there continues to be no funding and no messaging about what an emergency this is for those of us who are caring for the LGBT community, it’s going to spread,” she said.
Roth said that thankfully, there are already vaccines and treatment to combat monkeypox, unlike when HIV began to threaten queer communities. But the long and devastating history of AIDS in this country underscores that “in times of health crisis, the queer community really does step up for themselves,” he said.
Gay men and other queer people at risk have clamored for the vaccines when they can get them: In San Francisco and Los Angeles, people have waited hours to get the shots. An L.A. County public health official said that last month, when the department opened up thousands of additional slots on an online portal for monkeypox vaccinations, they were filled within three hours. At a recent news conference, TerMeer said the wait list for vaccines at the San Francisco AIDS Foundation had surpassed 10,000.
“I don’t know a single person that’s hesitating to get the vaccine,” said Bannon, the San Francisco activist. That too is the legacy of decades of the HIV/AIDS crisis, said Bannon, 68, who is HIV-positive and lost a partner. “Trust me, if anyone I knew back then knew that they could go and get a shot and stop it — they would have done it.”
Times staff writer Grace Toohey contributed to this report.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.