Column: ‘This work speaks to my heart’: A student helps take primary medicine to the street

The doctor is behind the wheel as the van pulls into a Shell station in Santa Monica, where a 36-year-old man with a serious heart condition lives in the parking lot.
Dr. Coley King of the Venice Family Clinic spots Rene behind the carwash, raking leaves. Rene maintains the grounds in an arrangement with management that allows him to call this place home.
“We saw him one day and he was swollen from head to toe,” says King, who tells me Rene was rushed to the hospital late last summer.
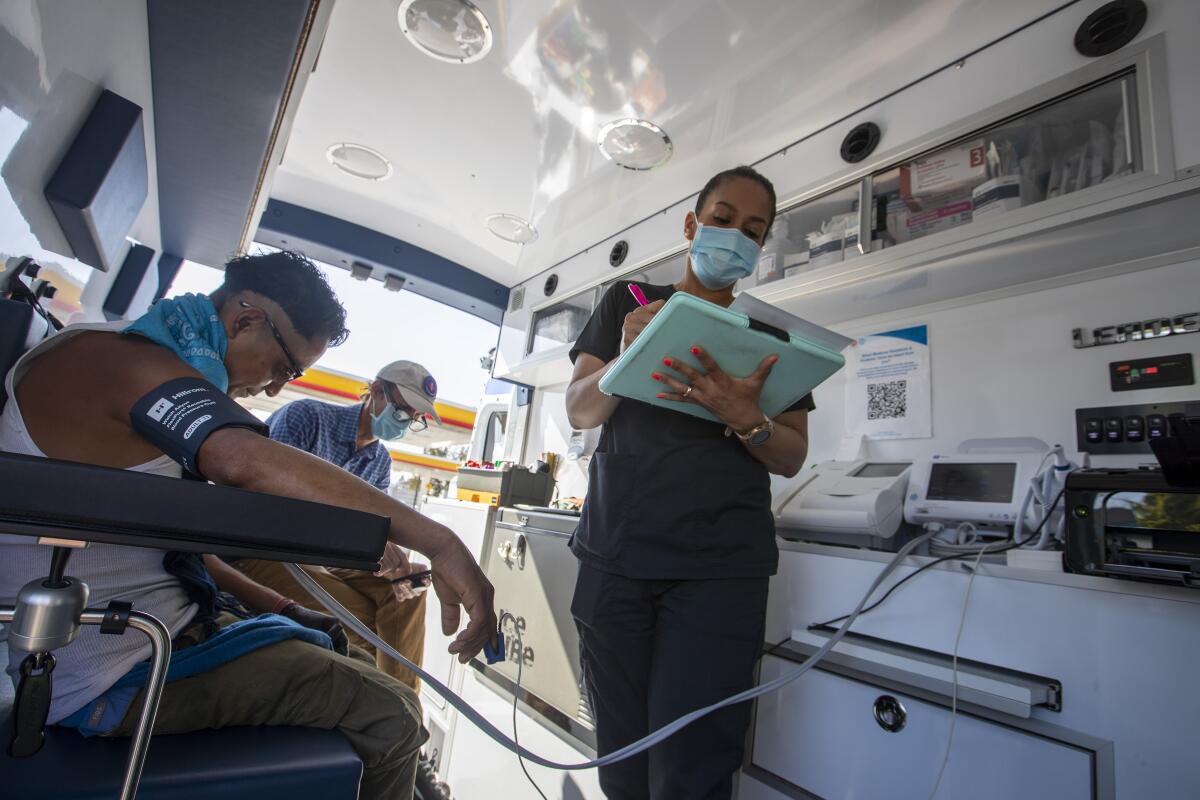
The team pops out of the van. Nick Wenzel is a therapist with the People Concern. Jacqueline Ramirez is an LVN with the Venice Family Clinic. And Francesca Reinisch is a street medicine trainee from USC, where she’s about to graduate as a physician assistant.

Wenzel checks on Rene, who steps up into the van, where the medical team draws blood and checks his blood pressure and vital signs. He’s in decent shape, King and Reinisch determine. King knows by a pill count that Rene is taking his meds, and he tells the team he’s been sober for several months.
“Pill management, for heart failure, is a big deal,” King says. “If he stays on meds, he stays out of the hospital. If he goes off the meds, he fills up with fluid.”
You’re walking down the street and you notice someone in distress. Should you stop and help? How? Mental health experts share the best steps to take.
Rene is glistening with sweat and complains of pain in his rib, back and shoulder. Reinisch checks his lungs and said he sounds OK. So maybe he’s overexerted himself with the raking and sweeping. He was assaulted twice, not long ago, but says there are no lingering injuries.
Rene tells me he has been homeless for about 20 years. Wenzel has helped reconnect Rene with his mother in Mexico, and I ask him if he misses home.

“The whole world is your home,” Rene tells me. “The ground you stand on,” that’s home. On the edge of the gas station parking lot, he’s set up bookshelves and planted a garden, with tomatoes and squash. The squash is just starting to come up. “Live life in full bloom,” says a sign he’s posted in his garden.
Managing Rene’s health is one task. Finding him a place to live is another. And shortages abound.
“We’re trying to get him into permanent supportive housing and looking hard for creative financing,” King says.
That’s what it often comes down to for care providers. They work the phones. Call in favors. Shuffle and scramble for hotel money, for rehab beds. Whatever it takes.
“We’re really bringing healthcare to where people are,” Reinisch says. When a patient comes to a clinic, it’s not as easy for medical staff to get a good sense of living conditions and barriers to better health.

In one case, a couple with multiple health problems agreed to move into temporary housing, but not without their pet iguanas, and not at the risk of losing their belongings, which included custom-built dollhouses. King was on the phone with an aquarium, trying to persuade them to host the iguanas, while the rest of the team arranged to keep the dollhouses in someone’s garage.
“I love this work,” Reinisch says, telling me that the collaborative, interdisciplinary approach makes it a little easier to manage someone’s health and cut through bureaucracy.
Reinisch is one of 16 USC students who did field rotations this semester in the street medicine program established by Brett and Corinne Feldman, who teach family medicine as assistant professors at Keck USC. Brett Feldman tells me the couple worked in street medicine in Pennsylvania, and when he came to L.A. in 2017 as a consultant, he was “completely blown away by the magnitude of the crisis here.”
He got to know about King’s medical outreach in Venice, “and we knew there needed to be a whole lot more people doing this work,” as well as a pipeline of Francescas to join the cause.
Many times over the years, I’ve wondered why Los Angeles, with its tens of thousands of homeless people and multiple daily deaths, doesn’t have hundreds of full-service mobile clinics like this one. It seems like an obvious first step in getting people well, and housed.
Now there’s progress afoot, with several street medicine programs in place, run mostly by nonprofits and universities. And Dr. Heidi Behforouz, medical director of the county’s Housing for Health program, tells me funding has been secured to keep four medical vans rolling.
During the pandemic, they were operated with COVID-19 funding and focused on vaccinations, she says. But the medical teams identified numerous untreated conditions — including injury, chronic disease and addiction — that argued for full-service mobile units.
“I wish we had more vans, and we just don’t right now, but it’s a start. It’s the beginning of our revolution,” says Behforouz. She tells me she’s working to link all mobile medical teams in the county to the same database, so that wherever a patient is contacted, caregivers will have access to medical and prescription histories.
Back at the wheel, King takes the team to a spot near the beach, and Wenzel goes in search of a patient on medication for bipolar disorder. The patient is waiting for housing, King says, and one of the last obstacles is that a doctor has to do an exam and sign a verification of disability form to open a funding door.
Wenzel returns to the van with 43-year-old Kevin, who tells me he’s eager to move indoors and get back to work. He’s got welding experience. On the beach, he says, he can’t let himself fall into deep sleep because someone might steal his belongings.
King asks Kevin how he’s doing and Reinisch moves a stethoscope over his upper body. She tells King:
“I definitely got some wheezing in the lower right lung,” she says. She checks Kevin’s prescription and finds that he’s good for another year of asthma medication.
King, who wrote the curriculum for trainees like Reinisch, tells me that he can often tell early on which students have the will, the patience and the temperament to become good at street medicine. He knew right away that Reinisch has a desire to do her part in the midst of a teeming humanitarian crisis.
“This work speaks to my heart,” says Reinisch.
It’s a job that requires a terrific bedside manner, because a lot of unhoused people don’t trust that anyone is ever there to help. King, with his folksy, engaging manner, is a master at putting patients at ease.
“He’ll kind of just chat with people, as if they’re a friend, or he’s wanting to get to know them. And in that conversation, he’ll ask some pointed medical questions … and use his casual, disarming nature to build a medical history” that helps him build a treatment plan, says Reinisch.
She says she hasn’t been surprised by the amount of mental illness, chronic physical illness and addiction she sees. But trauma is perhaps more prevalent than she expected, and it’s often early childhood trauma with years-long effects. She’s also observed the ways in which poverty impacts health and health impacts poverty.
Get the lowdown on L.A. politics
Sign up for our L.A. City Hall newsletter to get weekly insights, scoops and analysis.
You may occasionally receive promotional content from the Los Angeles Times.
Reinisch says one big surprise for her is the level of intellectual development challenges that make it difficult for people to sort through options and make decisions in their best interest. She’s learned to listen, to try to inhabit the world of her patients, to share objectives, to compromise.
And to keep going back.
In the current L.A. mayoral and council campaigns, there’s a lot of back-and-forth among candidates about how many times you should have to offer help to someone before cracking down. Once? Twice?
No two cases are alike, and some people can benefit from a bit of prodding. But thousands of people are so damaged and distrustful, you can’t begin to help them without multiple repeat visits aimed at building trust.
A good example of that plays out at Reed Park in Santa Monica. Reinisch examines the badly swollen foot of a man in a wheelchair whose right side is paralyzed. King checks up on a woman he treated for drug addiction and potentially deadly infections.
Together, King and Reinisch come upon a homeless man King has known for two years. The man pretty much avoided any outreach until recently, when King broke through and prescribed medication for schizophrenia. In their last visit, the man wasn’t very talkative and refused to have his blood pressure taken.
This time, he lets Reinisch take his blood pressure, which is a healthy 110 over 80. He tells King he’s been taking the meds, and King tells him his speech and thoughts are much more clear. They talk about getting him into supportive housing, and the man says that’s something he’s got to work out in his head, but he’s not closing the door on the idea.
“This is a home run,” says King as he and Reinisch walk toward the next patients.
It’s not a leap, it’s just a small step. But it’s progress.
“This is how you win the game,” says King.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.












