Can Omicron overtake the Delta variant? Here’s what it will take

With a handful of cases now confirmed across the country, it’s clear that the Omicron variant has established a toehold in the United States.
But whether these initial infections fade out or become the beachhead for a new viral assault depends largely on how Omicron stacks up against a now-familiar foe: the Delta variant.
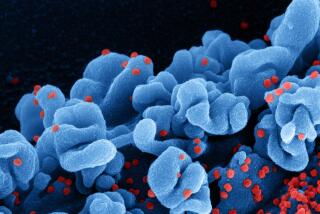
Since it burst onto the scene last week, scientists have been working to figure out whether its numerous mutations help it spread more easily than its predecessors, make its victims sicker, or reduce the effectiveness of COVID-19 vaccines and medicines.
Yet there’s another question that’s just as important for forecasting Omicron’s effect on the pandemic: What if it’s no match for the devil we know?
“Can Delta outcompete Omicron, or will Omicron thrive in the face of Delta?” said John Moore, a professor of microbiology and immunology at Weill Cornell Medical College. “That’s just a complete unknown at the moment.”
The Delta variant has long been the dominant strain in the U.S. — and it was the culprit behind a renewed wave of cases, hospitalizations and deaths that swept the country over the summer.
“Dominant” undersells just how widespread Delta is. In the United States, it’s nearly omnipresent.
“I know that the news is focused on Omicron, but we should remember that 99.9% of cases in the country right now are from the Delta variant,” said Dr. Rochelle Walensky, director of the U.S. Centers for Disease Control and Prevention. “Delta continues to drive cases across the country, especially in those who are unvaccinated.”
Omicron’s impact on the COVID-19 pandemic will depend on a variety of factors that will take days to weeks for scientists to untangle.
The reason for the strain’s supremacy is simple: It’s twice as transmissible as the original SARS-CoV-2 virus. As a result, it’s been able to elbow aside other variants that otherwise might have spread more widely.
Look no further than the Beta variant, which scientists considered a potential threat because it looked like it might imperil the efficacy of COVID-19 vaccines.
“Never happened,” Moore said. “Beta was squelched out by Delta. Well, that could happen to Omicron.”
In Africa, Omicron has been linked to a steep rise in new infections, suggesting it is indeed highly transmissible. But it may have faced less daunting competition in Africa than it will in the United States.
The Alpha and Beta variants continue to circulate widely in Africa, accounting for almost half of new infections examined there. It’s possible that Omicron can outcompete them but will be stymied by Delta.
That’s not entirely good news. Delta has proved more than capable of cutting a devastating swath through the U.S.
Even without factoring in Omicron, “we already are facing a Delta-driven winter surge that is going to kill another 100,000 to 150,000 Americans,” Moore said.
The Omicron variant was probably incubated in a person with poorly controlled HIV who struggled to clear a coronavirus infection.
Omicron’s rise in South Africa came at a time when new infections were relatively low, a context that could lead to overestimates of its transmissibility. As scientists stepped up their collection of viral samples around an outbreak, they may have captured a high rate of spread that was unique to that cluster but won’t reoccur in a broad population.
There have been early signs that Omicron is more capable of reinfecting people who have recovered from earlier coronavirus infections.
“Not a massive effect. But it’s statistically significant,” Moore said, based on preliminary analyses he’s reviewed. “And that would be consistent with the highly mutated nature of Omicron.”
A new threat assessment from the United Kingdom’s Health Security Agency says that models developed by scientists at Oxford University suggest Omicron may replicate more quickly in the body by binding more tightly to the ACE2 receptor on human cells. That binding affinity appears to happen “to a much greater extent than that seen for any other variant,” the report states.
Officials note the pandemic is different this year, given the ample supply of vaccines, which should provide some protection against the new variant.
Scientists have long argued that in a virus’ unending quest to infect new hosts, genetic mutations that increase transmissibility will best ensure its survival. New variants give the coronavirus fresh opportunities to spread and secure its future, said Wesleyan University microbiologist Frederick Cohan.
There are many ways to do that, and the virus needs to hit on the right change to improve its prospects, Cohan said. It could make itself more transmissible by hovering longer in or traveling more readily through the air. It could keep infected people contagious for longer. It could cause milder illness, keeping spreaders in wide circulation.
Widespread vaccination slows transmission by making the virus work harder to find its next victim. But if Omicron — or any other variant — finds a way to overcome the protection offered by vaccines, the reward will be a bigger pool of potential hosts.
In a sense, a vaccine-resistant variant would regain the target-rich environment the original strain enjoyed at the beginning of the pandemic, said Dr. Jonathan Schiffer, an infectious-diseases expert at the Fred Hutchinson Cancer Research Center in Seattle.
“The virus that might win now is not necessarily the same variant that won in the past,” Schiffer said.
President Biden announces new measures as scientists try to determine how dangerous the new Omicron variant of COVID-19 will be.
Still unknown is whether people sickened by Omicron are more or less likely to become severely ill than people sickened by Delta.
The chair of the South African Medical Assn. said in a newspaper op-ed this week that “no one here in South Africa is known to have been hospitalized with the Omicron variant.”
That’s heartening, but officials say it’s still too early to know whether Omicron will make people more sick than Delta does. It’s possible that Omicron has treaded more lightly on its victims in South Africa because it has infected younger, otherwise healthy people who aren’t particularly likely to become severely ill with COVID-19. If the new variant encounters a more vulnerable population, the picture could change, Moore said.
“Usually, it takes time for a severe illness to really require hospitalization,” said Dr. Regina Chinsio-Kwong, an Orange County deputy health officer. “So we will find out, probably in another two weeks, how severe Omicron can be on the system.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.