Racism and inequity fuel coronavirus-related death toll among L.A. County minorities, officials say

Black, Latino and Pacific Islander residents of Los Angeles County are twice as likely to have died of COVID-19 than white residents, according to new data, a troubling sign of the role racism and inequity have played in the uneven spread of the novel coronavirus.
For the first time in L.A. County’s weekly tracking, the age-adjusted death rate per 100,000 people among Latinos is now double that of white people, according to data released Friday by county officials.
White residents of L.A. County were the least likely racial and ethnic group to die of COVID-19, with 15 fatalities reported per 100,000 Caucasian residents.
Officials estimated that if minorities were dying at the same rate as whites, there would have been at least 700 fewer deaths in L.A. County. As of Tuesday, there had been 2,710 coronavirus-related deaths in the county.
“The very real impact of the injustices plays out every day ... and amplifies why racism is a public health issue,” Dr. Barbara Ferrer, Los Angeles County’s public health director, said. “And the disproportionately higher number of deaths from COVID-19 among Black and brown people is an indication of the impact of racism and discrimination on health and well-being.
“These numbers are absolutely devastating and represent real people whose lives have been lost,” Ferrer said. “They also starkly show how inequities have a life-and-death consequence.
“We shouldn’t see these big differences,” she added.
Those living in areas with high rates of poverty have almost four times the rate of death from COVID-19,
For every 100,000 residents who live in areas with very low poverty rates, 13 have died. But for every 100,000 residents who live in areas with high rates of poverty, 51 have died.
“It starts at the beginning of life, when Black babies are three to four times more likely to die before they reach their first birthday, and at the very end of life, when Black residents die, on average, six to 10 years younger than all others,” Ferrer said.
“We must look at the structure, systems and practices in our society to understand the root cause of these inequities, which really have much to do with a long history of institutional racism. And that’s resulted in — and continues to result in — fewer resources and opportunities that are needed for optimal health and well-being,” Ferrer said. She thanked “everyone who’s been on the front lines for this last week, standing to end racism and oppression.”
Here’s what we can do about COVID-19’s racial inequality.
Health disparities that have led Black people to be sicker and caused them to die younger than white people have persisted since the founding of the United States, Dr. Mary Bassett, a former health commissioner for New York City and professor of Harvard’s T.H. Chan School of Public Health, said recently.
Dr. Christina Ghaly, director of health services of L.A. County, agreed that the disproportionate impact of the coronavirus on minorities “is due to the long-standing structural and systemic racism that is apparent in multiple aspects of our society.”
How minorities are dying at substantially greater rates than white people
Death rates due to the coronavirus are worse for every other racial and ethnic group in Los Angeles County compared to white residents.
For every 100,000 white residents in L.A. County, there have been 15 COVID-19 deaths. Here are the COVID-19 death rates for other racial and ethnic groups:
For every 100,000 Black residents, there have been 31 deaths.
For every 100,000 Native Hawaiian/Pacific Islander residents, there have been 30 deaths.
For every 100,000 Latino residents, there have been 29 deaths.
And for every 100,000 Asian American residents, there have been 21 deaths.
The rates were adjusted for differences in age distribution among each racial and ethnic group.
The disparity in the death toll is also striking when factoring in community poverty levels.
Most California voters say coronavirus is increasing inequality, especially among blacks, poll finds
Some 70% of California voters believe that the COVID-19 pandemic is increasing inequality in the United States, according to a UC Berkeley IGS poll. Most also agreed that there were racial disparities in the virus’ effect.
People in areas with high poverty rates have nearly four times as many deaths from COVID-19, L.A. County public health director Barbara Ferrer says.
‘A disturbing picture’ of excess deaths among minorities
L.A. County officials also calculated the numbers in a different way: How many more minorities died because they didn’t have the health advantages white people have?
When there are big differences in health outcome by race, ethnicity or where you live, public health scientists know that “what they’re reflecting is the result of not having access to resources and opportunities that really contribute to optimal health,” Ferrer said.
So health experts can calculate a number of excess deaths among groups of people that “didn’t have the advantage of being in that reference group — whichever group does the best,” Ferrer said.
When county scientists looked at excess deaths linked to the coronavirus by race, ethnicity and income, “it paints a disturbing picture,” Ferrer said.
“If the coronavirus death rate for all groups were the same as it is for white residents — who have the lowest death rate — we would have 754 fewer deaths,” Ferrer said, of the 2,373 people who have died in L.A. County whose race and ethnicity information was available.
The latest maps and charts on the spread of COVID-19 in Los Angeles County, including cases, deaths, closures and restrictions.
This means that, because of the disproportionate effect the coronavirus is having on these racial and ethnic groups compared with white people, there were:
- Among Latinos, 485 excess deaths
- Among Blacks, 143 excess deaths
- Among Asian Americans, 125 excess deaths
And when experts look at communities by income, and assume that death rates for all groups could be the same as for people living in wealthier areas, they found:
- Among people living in areas with higher levels of poverty, 981 excess deaths
The death rate in Los Angeles County is far greater for Native Hawaiian/Pacific Islander, black and Latino residents than for white people, data show.
Here’s what we can do about COVID-19’s racial inequality.
Large gatherings bring a risk of coronavirus. But health experts are supporting protests being held in response to the death of George Floyd.
Increasing testing in minority neighborhoods
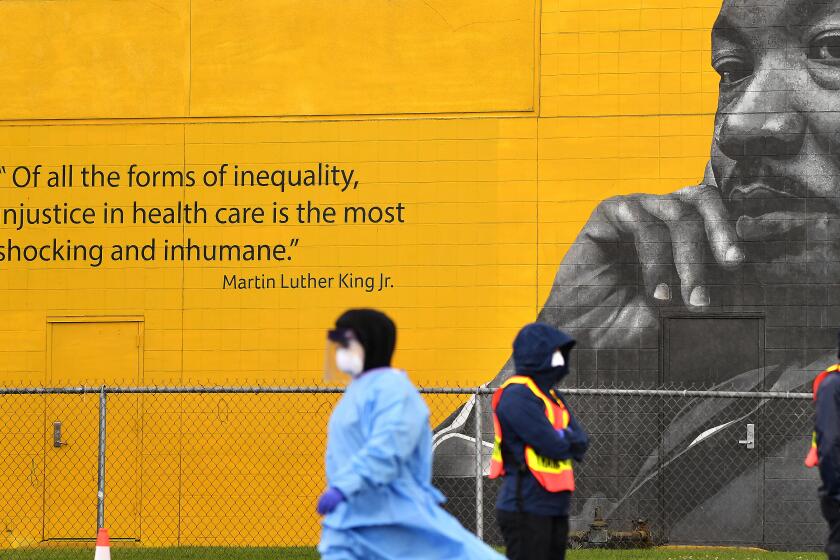
Ghaly said the county is focused on trying to ramp up testing sites in areas that especially need them and connecting people who are found to be positive with clinical care. One county testing site at the Charles R. Drew University of Medicine and Science in Willowbrook, south of Watts, is staffed by workers from the Martin Luther King Jr. Outpatient Center and connects people with the outpatient center or other clinics.
Ghaly said staff at Charles Drew University are trying to reach out to the community to encourage testing, canvassing local grocery stores and community-based organizations, a practice she credits with increasing daily testing from about 150 people to more than 700.
“This is a model that we’re very proud of and that we can follow — a successful community-based approach to testing and outreach,” Ghaly said.
She said the county plans to apply for a $4-million grant from the U.S. Centers for Disease Control and Prevention to help fund communications campaigns in hard-hit communities and among non-English speakers.
Some public health experts are bracing for a spike in COVID-19 cases in the wake of protests against police brutality.
One sign of promise, Ghaly said, is that communities of color are accessing drive-through testing sites at a rate proportionate to the overall population.
“But given how the death and case rate is disproportionately falling on these at-risk communities, we need to do more,” she said.
Experts have been worried about the brief closure of many government-run testing sites throughout L.A. County. Half of the approximately 40 facilities were shut down at some point in the last week amid protests against the death of George Floyd while in police custody in Minneapolis.
Ghaly said each testing site made its own choice whether to close or reduce hours. Volume of testing declined slightly last week, Ghaly said, in some cases related to closures; in others due to patients not showing up or canceling amid concerns about demonstrations or curfews.
Here are the percentages of L.A. County residents who had died as of Friday from COVID-19, categorized by race and ethnicity, for the 2,373 people for whom officials have such data:
Latino: 41%
White: 28%
Asian: 18%
Black: 12%
Native Hawaiian/Pacific Islander: Less than 1%
Other: 1%
For comparison, here are the percentages of L.A. County residents by race and ethnicity:
Latino: 49.3%
White: 27.6%
Asian American: 14.5%
Black: 8.2%
Native Hawaiian/Pacific Islander: 0.2%
While these statistics, on first glance, may suggest that Latino residents are not dying at a disproportionate rate in L.A. County, they do not take into account how Latino residents make up a relatively younger demographic in L.A. County compared with, for example, white residents.
A Los Angeles Times analysis published last month found that while the early weeks of the pandemic in L.A. County suggested infection rates were greater in wealthier communities, in mid-April infection rates in poor communities began to overtake wealthier ones.
The analysis found that infection rates across South and Central Los Angeles and the Eastside have increased sharply and now lead all regions in the county, exceeding 600 infections per 100,000 people, the analysis shows.
Poorer areas, such as Pico-Union and Westlake in Central L.A. and Vermont Square in South L.A., all reported low infection rates in early April but now rank among the top 10 communities out of more than 300 countywide.
The analysis found that areas hit hardest by the coronavirus are largely concentrated in the poorest, most crowded neighborhoods — areas with a high concentration of essential workers, more crowded housing and higher rates of underlying health conditions such as asthma, diabetes and heart disease.
Times staff writers Tony Barboza, Soumya Karlamangla, Ryan Menezes, Deborah Netburn and Ben Poston contributed to this report.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.