UC has a solution to the national shortage of coronavirus testing — do it in house
The University of California’s five medical centers are gearing up to expand their own in-house testing for cases of the novel coronavirus — a move that could greatly accelerate efforts to identify infected patients and stem the pandemic.
By the time they fully ramp up in the coming days and weeks, the centers could provide hundreds of tests a day to their patients. It’s questionable, however, whether they will have the capacity to open testing to the public.
Such an increase in testing can’t come quickly enough for public health professionals, as it would ease the pressure on overwhelmed state and county health labs to contain the contagion by quickly identifying infected Californians. So far, a limited number of tests — both in California and nationwide — have prevented everyone with symptoms from being tested for the virus.
The UC system joins Stanford University, which was the first academic medical center in California to develop its own test and begin using it on a limited basis to diagnose patients.
In Baltimore, Johns Hopkins Hospital also began using its own test this week on about 50 patients per day. Researchers there say they hope to move to a daily load of 1,000 samples in the next few weeks, using both manual and automated testing processes.
“Pretty much every academic medical center is either in the process of looking into in-house testing or already started to go live,” said Nam Tran, UC Davis Health’s senior medical director of clinical pathology. “Everyone is accelerating plans and identifying workarounds one way or another because there is a shortage of supply and commercial labs may not be able to keep up with the demand of the country.”
A lack of test kits, testing ingredients, lab staffing and equipment has slowed California’s response in particular.
Statewide, only about 1,900 people have been tested for the coronavirus as of Friday morning, despite several thousands — if not hundreds of thousands — of people who have probably been exposed to it. Without testing, it is unclear who is sick and needs to be quarantined, allowing the illness to spread to more people.
The UC system, along with private companies and other universities, aims to ease the logjam.
“The academic medical centers, Stanford and the UCs, are leading the charge in California,” said Omai Garner, an associate clinical professor who directs clinical microbiology testing for UCLA Health. “We have the resources and we have the in-house expertise.”
UCLA, along with UC San Francisco and UC San Diego, already have begun in-house testing for their patients and hope to rapidly ramp up in coming days. UC San Francisco has developed its own test and aims to use it for as many as 400 patients a week. UCSF officials emphasized, however, that they are using the test for their own, sickest patients, not the public.
UCLA and San Diego also are serving their own patients. The Westwood medical center is using the test developed by the U.S. Centers for Disease Control and Prevention, but began processing the samples on its own equipment Tuesday.
Taking it in-house has cut the turnaround time to as little as eight hours compared with a few days for samples sent out to an external lab, Garner said. UCLA can now handle from 40 to 80 tests a day, he said, adding he would like to increase that volume tenfold.
San Diego is testing about 20 patients a day with its own test. The turnaround time is eight hours, which includes first ruling out other respiratory illnesses, such as influenza.
“We are taking multiple strategies to substantially increase this capacity in the next few weeks,” Steven Gonias, chief of pathology for UC San Diego Health, and David Pride, associate director for diagnostic microbiology in the UCSD Center for Advanced Laboratory Medicine, said in a statement.
UC Davis, however, is poised to vastly expand in-house testing with a new state-of-the-art instrument that can automatically process more than 1,400 samples daily — far faster than testing at most other labs, which do so manually.
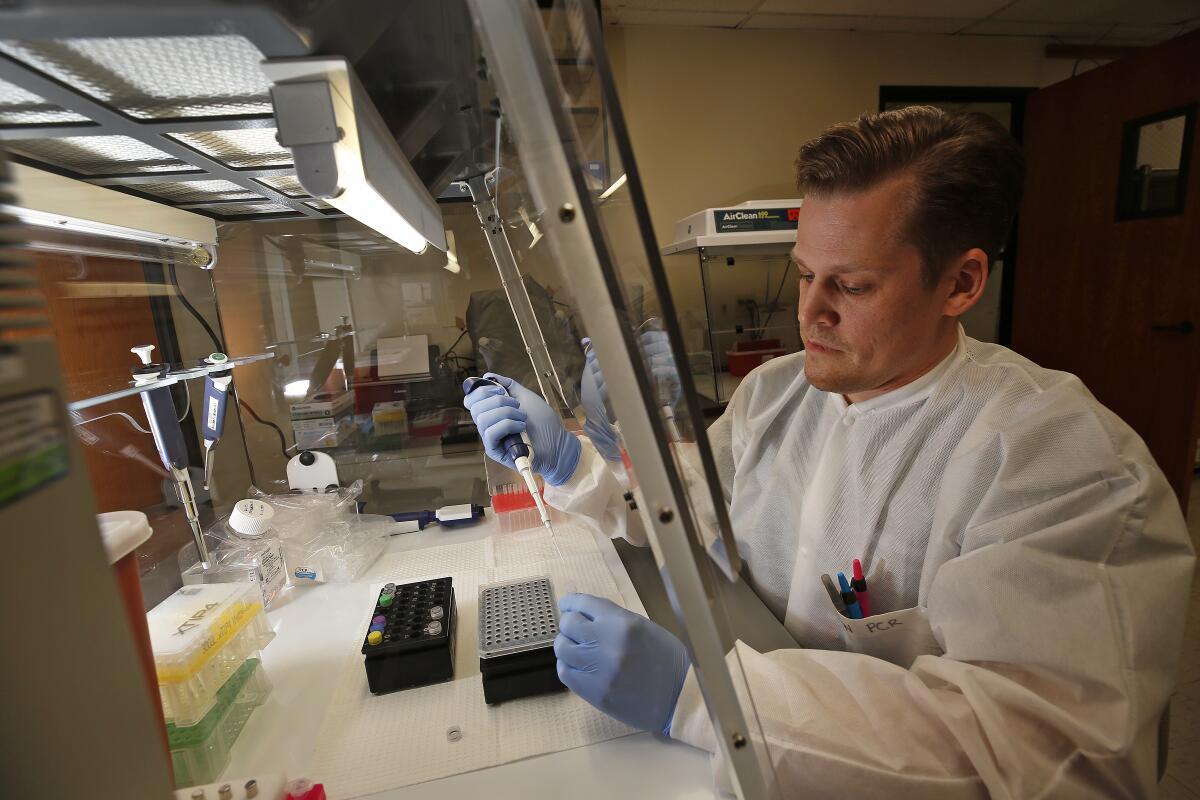
Technologists such as clinical lab scientists using the manual process must extract genetic material from each sample, obtained through a nasal or mouth swab, with a concoction of chemicals. Then they must analyze it to see if it matches the genetic sequence found in the virus that causes COVID-19. The process can take several hours for just one test.
Tran said the UC Davis molecular lab in Sacramento hopes to process up to 1,440 samples a day on its new instrument, a cobas 6800 by Roche Diagnostics of Switzerland.
The lab installed the molecular diagnostics instrument last December, Tran said, expecting to use it for routine tasks such as cancer gene screenings and testing for other infectious diseases, such as HIV. Then the coronavirus outbreak hit.
The model that UC Davis purchased allows researchers to run not only Roche tests but also their own. Once the federal government issued new rules in late February speeding the approval process for commercial, research and academic labs to develop their own tests for the virus, Davis researchers began working on their own “home brew,” as Tran put it.
Their recipe uses some different chemicals than those that are found in the federal CDC test, allowing the medical center to reach into its own supply chains and avoid the national shortages of the components, known as reagents, Tran said.
The test is being validated per U.S. Food and Drug Administration criteria and should be ready to roll out within a few weeks, he said.
“I think we’ll be able to offer faster testing and alleviate a lot of the burden on public health labs,” Tran said.
Dr. Aimee Moulin, an emergency room physician at UC Davis, said it currently takes about two days to get test results back from private labs. She said Davis has treated three positive COVID-19 patients so far.
UC Irvine Health also plans to begin in-house testing April 6.
UC San Francisco is at work on potentially game-changing research that could make testing for the virus as easy and widespread as flu screenings. An experimental test by Charles Chiu of UCSF and Janice Chen of Mammoth Biosciences in South San Francisco could produce results in as quickly as 30 minutes by incubating a sample in a test tube and determining the presence of the virus using a strip that would change colors like a pregnancy test.
The work is based on a technology known as CRISPR-Cas, which can identify genetic sequences.
“We are using CRISPR as a way to detect the needle in the haystack to be able to very rapidly identify whether or not a patient has been infected by looking for genetic sequence from the virus,” Chiu told KTVU Fox 2. “We need to be able to test for the virus in a doctor’s clinic, in an emergency room, or even potentially at the airport.”
The team is seeking FDA approval for the test but has not yet found a commercial partner to manufacture and distribute it widely.
Meanwhile, more tests are on the way. On Friday, Roche announced that the FDA had authorized the use of its high-speed test for the virus by certified laboratories and said it could make millions of tests available each month.
Garner, of UCLA, said the development of tests by diagnostic manufacturers offered the best way to ramp up testing quickly and make it available beyond specialized academic labs.
California health officials said such added capacity will be a godsend to the state, where confirmed cases have multiplied to 247 as of Friday morning. Five people have died.
At a press briefing Thursday, Barbara Ferrer, director of the Los Angeles County Department of Public Health, reiterated that county labs and even commercial labs have limited capacity for testing for the virus.
“We’re really excited about hospitals being able to order the machines and the tests in their own labs for their own patients,” she said.
Because of low testing capacity, Los Angeles County officials have maintained that patients without a history of travel to an affected country can be tested only if they are sick enough to be in the ICU. When patients did qualify for testing, it could take four to five days to get results back from the CDC, she said.
At UCLA, the limited number of tests has prevented everyone who has wanted to be tested from being tested, said emergency room nurse Marcia Santini.
“When we needed to test them,” Santini said, “we didn’t have the ability to test.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.












