Biden launches a new push to limit healthcare costs, hoping to show he can save money for families
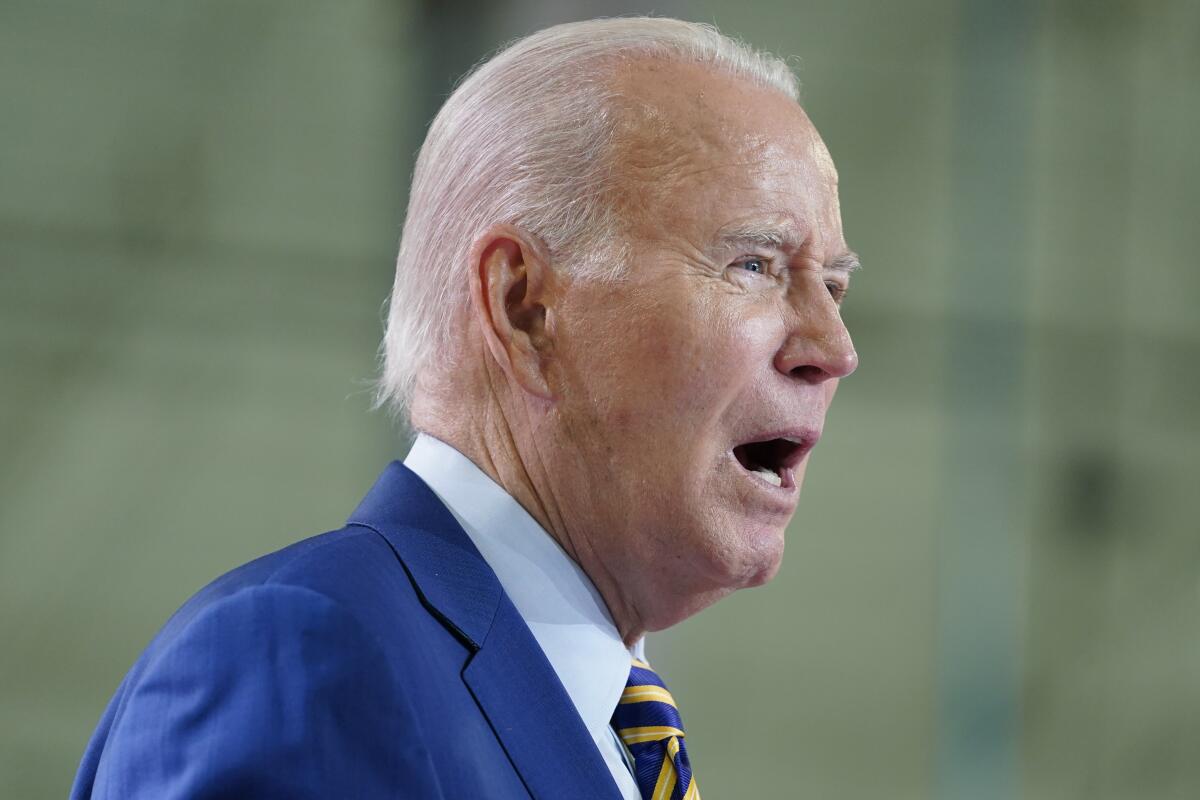
President Biden on Friday rolled out a new set of initiatives to reduce healthcare costs: a crackdown on scam insurance plans, new guidance to prevent surprise medical bills and an effort to reduce medical debt tied to credit cards.
Biden’s remarks will build on previous initiatives to limit healthcare costs, with the Department of Health and Human Services releasing new estimates showing 18.7 million older adults and other Medicare beneficiaries will save an estimated $400 per year in prescription drug costs in 2025 because of the president placing a cap on out-of-pocket spending as part of last year’s Inflation Reduction Act.
Gearing up for his 2024 reelection campaign as inflation remains a dominant concern for voters, the Democratic president has emphasized his policies to help families manage their expenses, as well as a spate of government incentives to encourage private sector development of electric vehicles, clean energy and advanced computer chips.
Republican lawmakers have criticized Biden’s policies by saying they have spurred higher prices that hurt the well-being of families.
The Biden administration plans to limit what it calls “junk” insurance plans, such as short-term policies that can deny basic coverage as people transition between employers and still need temporary healthcare coverage.
Inflation is down sharply, employment is holding steady and GDP is growing. But Americans are still blaming Biden for a lousy recovery.
Neera Tanden, director of the White House Domestic Policy Council, highlighted the case of a man in Montana who received a $43,000 healthcare bill because his insurer said his cancer was a preexisting condition.
“That’s not real insurance — that’s junk insurance,” Tanden told reporters on a phone call previewing Biden’s remarks. “We will propose a rule to crack down on these plans.”
The president also announced new guidance on medical billing stemming from 2020’s No Surprises Act. The guidance would limit the ability of insurers that contract with hospitals to claim that provided care was not in network and require customers to pay more money. Health plans also would need to disclose facility fees that are increasingly charged to patients and can surface as an unexpected cost in a medical bill.
“Frankly, what they are doing is gaming the system — this is not allowed,” Tanden said.
The Consumer Financial Protection Bureau and Treasury Department also are seeking information on third-party credit cards and loans that are specifically used to pay for healthcare. The higher costs and interest charges can discourage people in need of treatment from seeking care.
The president is expected to also highlight previous efforts to reduce healthcare costs, including a plan allowing Medicare to negotiate lower prices for prescription drugs and a $35 monthly price cap on insulin for people in Medicare Part B.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.











