Federal panel calls medical scopes unsafe
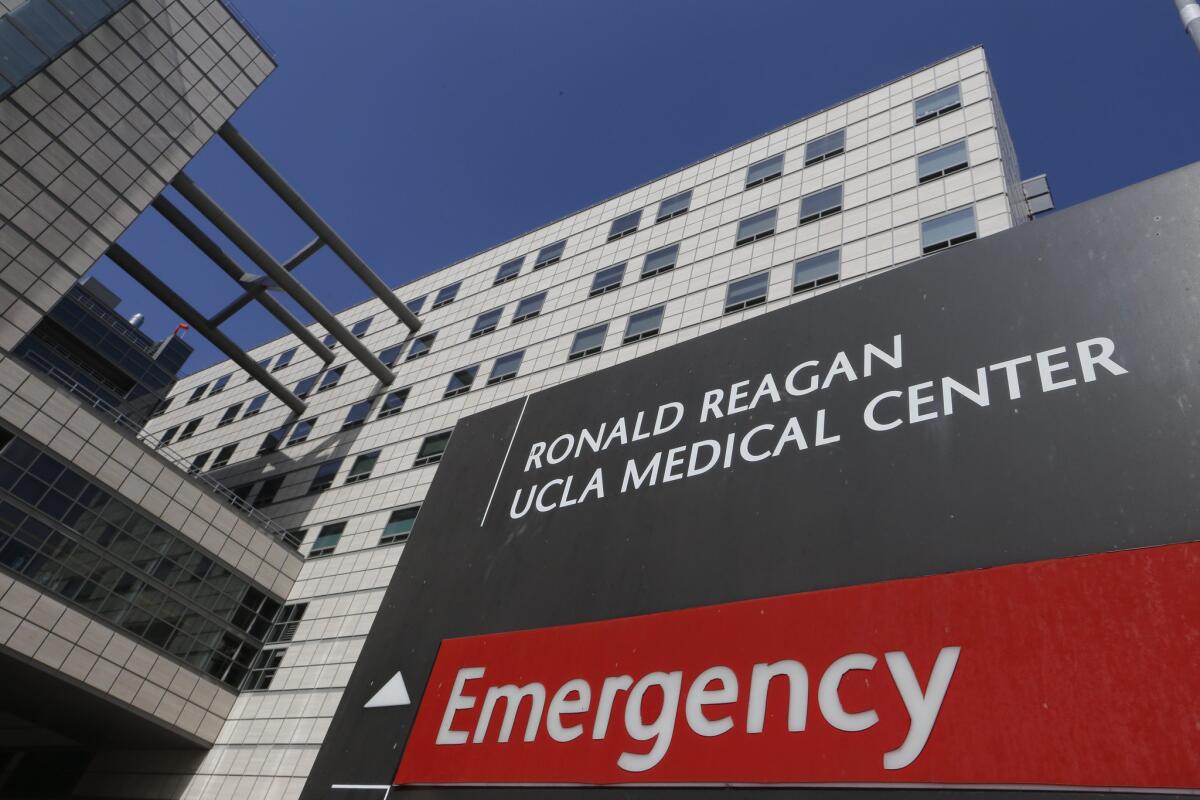
The FDA convened the advisory panel as part of its continuing response to duodenoscope-related infections at several U.S. hospitals, including
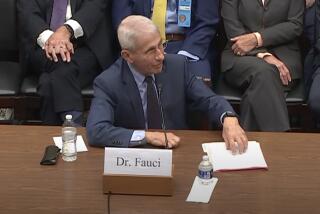
Reporting from SILVER SPRING, Md. — A federal panel concluded Friday that the medical scopes linked to a deadly string of superbug outbreaks are unsafe as designed and urged the U.S. Food and Drug Administration to do more to protect patients.
But the agency’s advisory committee stopped short of calling on the FDA to halt further use of the scopes.
Patients and doctors should continue to have access to the device, the group said, because it’s used in a potentially life-saving procedure with no better alternative.
Nonetheless, the panel’s decision marked a high-profile rebuke to Olympus Corp., the dominant maker of these duodenoscopes, and to the FDA for failing to impose sufficient measures to stop the spread of dangerous bacteria from patient to patient.
The FDA convened the advisory panel as part of its continuing response to duodenoscope-related infections at several U.S. hospitals. Federal officials have investigated nine scope-related outbreaks at hospitals that have sickened dozens of patients with antibiotic-resistant superbugs.
A top FDA official said the agency will carefully consider the panel’s recommendations as well as other information shared at the meeting from researchers, hospitals and patients.
“The agency considers this an urgent public health matter of great importance,” said Suzanne Schwartz, an official at the FDA’s center for regulating medical devices. “We are looking at this problem from A to Z.”
Both Olympus and federal regulators have scrambled to devise new cleaning methods ever since news of an outbreak at UCLA’s Ronald Reagan Medical Center set off alarms nationwide in February.
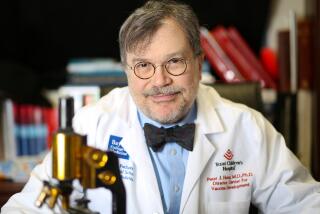
“We have heard enough data to say these devices are not safe using current conditions,” said Dr. Irving Nachamkin, a pathology professor at the University of Pennsylvania School of Medicine, and one of the panel’s 16 members.
“Everyone in this room is a potential patient,” he said, “and no one would accept anything other than a device free of pathogens.”
Noticeably absent from the discussion was Olympus and two other manufacturers of the scope. All three companies declined to participate in the two-day hearing, and several panel members chastised them for their silence on a serious health threat.
“I’m a little disappointed industry did not represent themselves,” said committee member Dr. Bryce Mays, a gastroenterologist at Fort Belvoir Community Hospital in Virginia. “I think they may have data critical to our thinking in terms of reaching a decision, and they chose not to.”
This week’s panel was made up of doctors, health experts and consumer representatives. FDA advisory committees have no authority to make regulatory decisions, but the agency often follows their recommendations.
Friday, several panelists urged the FDA not to limit its inquiry to just duodenoscopes. They noted that the transfer of pathogens has also been tied to bronchoscopes, colonoscopes and similar reusable devices.
“Let’s not pretend that it’s only happening with one set of scopes — because it’s not,” said Dr. Phyllis Della-Latta, a professor of clinical pathology at Columbia University.
But she and other committee members said they didn’t have enough data to determine the extent of the risk posed by other scopes.
The duodenoscope features a tiny camera mounted on the end of a flexible tube that is threaded down a patient’s throat and into the digestive tract. It is used in a procedure called ERCP, or endoscopic retrograde cholangiopancreatography. About 670,000 ERCP procedures were performed in the U.S. last year.
After the panel determined Friday that patients couldn’t be assured of the safety of ERCP scopes, it was asked by FDA officials if the device should be pulled from use.
Committee members rejected that idea, echoing regulators’ determination that doing so would do more harm to the public at this time.
“The risk of stopping this would be catastrophic,” said Dr. Kenneth McQuaid from the Veterans Affairs Medical Center in San Francisco.
Looking ahead, the advisory panel didn’t endorse any one method to reduce the infection risk.
There was discussion of prodding manufacturers to speed up a redesign of the scopes so they are easier to clean and don’t trap deadly bacteria in crevices at the tip. They did, however, urge companies to simplify their cleaning instructions which can run 100-plus pages.
Some ERCP physicians on the panel expressed frustration with Olympus for not sharing data on whether its revised cleaning instructions, issued in March and featuring a new brush, will actually prevent contamination.
“We need to demand that [Olympus] data. It’s hard for us to know if that is the right brush,” said Dr. Ashley Faulx, a committee member and gastroenterologist at University Hospital Case Medical Center in Cleveland. “Olympus of course will tell us to only use their brush. That is in their best interest.”
Mark Miller, a spokesman from Olympus, said the company had provided test data to the FDA showing its device could be effectively cleaned with the new brush and revised instructions. He said that data was confidential.
At the meeting, the FDA said the Olympus data had passed regulatory muster, but it offered no further details.
Miller said Olympus executives had listened to all of the two-day hearing and “as a result, Olympus has next steps to consider with our stakeholders.”
Several panel members expressed support for sterilization of duodenoscopes, an optional approach embraced by some medical providers after the outbreaks. The standard practice at many hospitals continues to be an initial cleaning by hand and then disinfection in an automated reprocessor.
But the gas sterilization available for these devices has drawbacks. The ethylene oxide is highly toxic and it can pose risks to healthcare workers and possibly patients if traces of the gas are left on the device. It’s also not widely available in some areas, and it can carry a significant cost, doctors said.
William Rutala, a professor of infectious disease at the University of North Carolina, testified Friday that current guidelines for cleaning duodenoscopes did not go far enough and hospitals must make changes right away.
“Today we are not ensuring patient safety because some percentage of scopes, between 10% to 30%, are contaminated,” he said. “Doing nothing is not an option.”
Twitter: @chadterhune, @melodypetersen
Terhune reported from Silver Spring, Md. Petersen was in Los Angeles
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.