The Dots Are Almost Connected....Then What? : MAPPING THE HUMAN GENETIC CODE
It is New Year’s Eve 2020 and, predictably, the ER of County/USC Medical Center is swamped with victims of drunk drivers and bar brawls. Shouting to no one in particular are the partiers whose proclivity for hallucinogenic highs prompted ingestion of excessive quantities of the drug du jour, ENDORPH. A host of psychological breakdown cases, battered by holiday blues, are recuperating from a variety of creative suicide attempts. And the normal load of heart attacks, seizures, births, domestic violence, beatings and pediatric illnesses is providing Dr. Fiona James’ staff with hundreds of diversions from late-night boredom.
James runs a well-oiled ER machine, admired nationwide for its efficiency and cost-effectiveness. Everyone knows their duties and performs them well. James and her residents bear ultimate responsibility for the most crucial patient decisions, which are usually based on genetic analysis.
“Seizure on open ward! We need a doctor over here STAT!” shouts one of James’ nurses.
“What do we know about this guy,” James asks the nurse as she grabs an air injection syringe loaded with neurotranquilizers. After shooting the chemicals into the teenage boy’s arm and noting the expected instantaneous easing of his spasms, James looks expectantly at the nurse.
“Driver’s license says Robert McIsaac, age 17, from Canoga Park,” nurse Tom Shaddiford reads.
“Canoga Park? What’s he doing way over here?” James asks. “Are there any relatives here?”
Shouts in the ER waiting room fail to roust anyone connected to young McIsaac, and the ward secretary says the teen wandered in on his own, barely coherent at the time.
“But he had this,” the secretary says as she thrusts a 2-by-3-inch plastic card at James. “I already read his phone number off of it and called his parents. They’re on their way in, and they e-mailed valid approval for emergency procedures as needed.”
Excellent, James thinks.
Reaching into her pocket, the ER chief fumbles for her Gen-Com. Damn, where is it? At last she feels the familiar little slab of hard plastic, pulls it out, flips open the case and slides McIsaac’s card in a slot behind the miniature video screen. A color 3-D image fills the screen, depicting McIsaac from all angles while a scrolling line of data across the bottom lists the boy’s identification and vital statistics.
Ignoring the image, James types quickly on the tiny keyboard: SEIV.ent.EPILEP? In 10 seconds the powerful 400 megabyte mini-computer provides the following information: No seizure history. No head injury history. No trauma history.
James then types: GENSRCH. Knowing this will take a bit longer, the physician takes a glance at heart rate and temperature data on the boy. Satisfactory. She turns back to her hand-held Gen-Com and whistles at the readout.
“Bad?” Shaddiford asks.
“Uh huh. The kid’s got the Chromosome 10 partial epilepsy gene coupled with the glucose intolerance gene GP6 and . . . .” “OK, I get the picture,” Shaddiford says. “I’ll prep the kid for gene therapy. Shall I wheel him straight upstairs now or wait for the parents?”
“Wait,” James says as she reprograms her Gen-Com to run a genetic lipids utilization profile on the DNA card from an apparent heart attack victim lying beside young McIsaac.
*
In the early days of 1996, things are progressing extremely well in the global effort to sequence the entire human genetic code. The Human Genome Project, executed by the U.S. National Institutes of Health and the Department of Energy, is way ahead of schedule. So are its counterparts in Europe and Japan.
There are 3 billion bits of information, called nucleotides, that make up a human being’s genetic database. By the end of 1995, scientists had very roughly mapped the locations and identities of all of those nucleotides. Most of the nucleotides are long, repetitive sequences that seem to serve structural or regulatory purposes of some kind, maintaining the shape and maintenance of the DNA. But about 100,000 stretches of the DNA are special: they are genes that determine everything from your hair color (undyed, of course) to whether or not your child will attain suitable stature and musculature to one day play in the NBA.
Though few doctors today are using this mountain of newly discovered information in clinical practice, the frontiers of medicine all revolve around the human genome, a duplicate set of 23 chromosomes nestled inside all the cells of the body (except red blood cells) that compose each individual’s genetic imprint. In years to come, physicians will base diet and medication recommendations for heart attack victims, for example, upon knowledge of their genetic profiles concerning cholesterol uptake. Diabetics will be treated in more refined fashion, with the gamut of their genetic/hormone interactions fully evaluated. And in the long term, scientists hope to find ways to alter medical fate, directly changing faulty genes or adding genes that will help would-be patients resist the deleterious impact of their inherited programming.
When the National Research Council first gave the green light to the Human Genome Project in 1988, only 400 of those human genes had been identified and located on the 23 human chromosomes, and less than one tenth of 1% of all nucleotides had been deciphered. By mid-1995, Eric Lander and his team of MIT hotshots at the prestigious Whitehead Institute had created a very rough outline of 90% of the human genome; 35,000 human genes had been identified, 7,500 of which have been located on the DNA. Less than six months later, the Lander team announced completion of a full human map that’s good enough to roughly locate every known human gene.
Given that the effort for approval only began in 1987, this has to constitute one of the most remarkable achievements of our scientifically noteworthy century. Back in 1987, a National Research Council committee predicted that an all-out international campaign might succeed in deciphering the entire sequence of nucleotides in human chromosomes within 15 years, at a cost of about $200 million per year to U.S. taxpayers, and additional smaller monetary burdens to the European Community and Japan. If the Human Genome Project maintained its 1990 pace it would certainly achieve that goal.
But it’s not maintaining that pace--it’s going far more rapidly. Recent technological and logistic improvements in deciphering capacity may result in completion of the auspicious goal five years ahead of schedule. (See sidebar.)
So, pronounces Lee Hood, “The 21st century is going to be the century of biology. There’s no question about it.”
Excited, optimistic and supercharged with energy, Dr. Leroy Hood has been--and continues to be--a key pioneer in the human genome revolution. First at Caltech and now at the University of Washington in Seattle in a seat endowed by computer mogul Bill Gates, Hood has invented machinery that enables scientists to rapidly decipher genetic codes. Since its inception he has served as the unofficial cheerleader of the Human Genome Project.
And the crowd is roaring with scientific approval. From Tokyo to Toledo, Los Angeles to London, scientists have eagerly enjoined Hood’s quest, not only helping to sequence pieces of DNA but inventing faster, more accurate ways to accomplish the task. The pace as we approach the millennium is dizzying. The excitement is palpable among gene hunters. Dr. Francis Collins, who heads the Human Genome Project, predicts the sequencing effort will be finished by 2002, a full three years ahead of schedule. And there are reasons to believe it may even be accomplished by the year 2000.
Last spring at the Cold Spring Harbor Laboratory on Long Island, scientists compared notes and managed to present maps for eight of the 23 human chromosomes. The maps are good enough to help an L.A. freeway driver, by analogy, find an exit leading to Westwood off the Santa Monica Freeway, but not yet adequately refined to guide that driver to the Westwood Boulevard entrance of UCLA. A still rougher map was completed last fall by the Centre d’Etude du Polymorphisme Humain in Paris spanning 75% of the human genome. Its specificity is good enough to, continuing the analogy, distinguish the San Fernando Valley from Central Los Angeles, but not to pinpoint towns or roads. Eric Lander’s map, which is rougher still, could just about distinguish California from Nevada.
Rough as these maps may be, they are a far cry from where the effort stood a decade ago, when the map-makers had about enough information to recognize the existence of continents and oceans and little more.
Nearly every day another gene is discovered, mapped along the DNA, or sequenced. Most of the fervor and scientific competition is directed at genes thought to cause diseases, about 100 of which had been found, or at least hinted at, by the end of 1995. The list of disease genes that have either been discovered, or whose location on the genome has been elucidated by more than one laboratory, includes several types of cancer, Huntington’s disease, cystic fibrosis, schizophrenia, Alzheimer’s, myotonic dystrophy, some forms of epilepsy, neurofibromatosis, improper lipid utilizations that contribute to heart disease and dozens more.
In addition, the list of basic human attributes that have allegedly been traced to specific genes or mapped on chromosome sites is expanding almost daily: from homosexuality to color vision--even a putative obesity gene that makes some people store vast amounts of fat. Many genes that are experienced in adulthood as cancer-promoting turn out to be essential signals for embryonic growth--signals intended to shut down following fetal development. Thus, the search for cancer genes is opening startling windows on basic fetal and infant growth.
So massive is the amount of quarternary nucleotide information that no single computer system is adequate to the task of its data storage and analysis. The Department of Energy stores most of the U.S. database at Los Alamos National Laboratory, using supercomputers originally designed for nuclear weapons and war games use. The European Community recently completed construction of the Bioinformatics Institute in Cambridge, England. Funded at a level of $8.5 million per year, the institute has enough computer power to process information on the more than 300 million human, microbe, plant and animal nucleotides already fully sequenced and the capacity to grow at a rate of 75% per year. Even at that, scientists see the institute as a mere stopgap measure. In order to completely understand how the data that is encoded in DNA ends up controlling a liver cell in one way, operating a neuron in the brain in another manner and functioning improperly in a breast cancer cell, new computer capacities will be needed--ones that can handle more than 100,000 interacting functions simultaneously in real time, Hood says.
All this computer power is needed to help humanity decode and understand its own genetic dictates. The level of complexity in DNA signaling is well beyond the simple binary system used by computers. Ironically, however, the basic DNA code is quite simple. As University of Washington molecular biologist Maynard Olson has noted, the nucleotide database in our DNA computers is only 750 megabytes in size, fills a microscopic amount of space in human eggs or sperm and, once elucidated, any individual’s personal genome sequence could be stored on a single CD-ROM.
“The Human Genome Project should get on with producing this disk, on time and under budget,” Olson declared in a recent Science magazine editorial.
Geneticist Peter Goodfellow of England’s Cambridge University believes that within five years all of the key genes responsible for complex human diseases will have been identified. Even more bullish is Harvey Lodish of the Whitehead Institute, who is convinced that science is just a few years away from having 3-D full-color computer presentations of DNA data for such things as speech, musical ability, body shape and eye color. Indeed, Lodish envisions a time when fetal DNA may be loaded into a computer and parents will be able to “see,” via computer, the child’s predicted physical appearance and talents--perhaps even hear its simulated voice of the future.
*
Though such forecasts are controversial, virtually all scientists in the field would agree with Nobel laureate Walter Gilbert’s bottom-line prediction: “The results of the Human Genome Project will produce a tremendous shift in the way we can do medicine, and attack problems of human disease. And the understanding that will come from this is likely to give us as people a much stronger feeling of how genetically influenced we are.”
Based on their collective writings and presentations at recent scientific meetings, it also seems apparent that human genome scientists would agree with Hood’s prediction that within 20 years all Americans will carry credit card-type plastic strips that contain computer readouts of their personal genomes.
“I can’t imagine that won’t be true,” Hood says. “I think that’s absolutely a given. Your entire genome and medical history will be on a credit card. You just put it in there [a computer] and a physician will instantly know what he’s dealing with. Physicians will really then have to look at humans as complex systems analysis.”
Mischievously, Hood enjoys asking physicians to describe what their jobs will be like in 25 years. “They can’t do it,” he says. “We all have pretty limited imaginations. But physicians can’t see how all this will affect them.”
Hood envisions medical practice that is fundamentally guided by genetic information. Doctors would lean heavily upon patient information obtained from each individual’s genome credit card, he says, the most important aspects of which will be probabilities. Few of the disease-relevant genes are likely to represent absolutes--to indicate that a child will definitely grow up and suffer lethal cardiovascular disease by middle age, for example. Rather, the genes will offer a complex array of statistical possibilities, all of which may be influenced by thousands of environmental, dietary, personality and other factors.
“So the vision is that very powerful computational tools, coupled with genomic information, will revolutionize medicine,” Hood says. “We’ll see emerge in the next 10 to 15 years a whole new field of biomedicine that will be manned by mathematicians. They’ll be in a position to do DNA fingerprints and compute your future health history for you. And then we will have moved into an era of preventive medicine,” wherein avoidance of certain environmental factors known to have a detrimental impact on a patients’ particular genes or direct alteration of those genes will reduce--even eliminate--the possibility of developing the otherwise likely disease.
Affymetrix, a Santa Clara-based company, has already embarked on Step 1--development of a one-centimeter-sized chip that contains all the genetic information needed to instantly identify 40 or 50 cancer genes from a single droplet of white blood cells. The chip is composed of 250,000 pieces of DNA, all of which are mirror-image mates to known disease genes. If your own genome contained one of the troublesome genes on the Affymetrix chip it would bind to its embedded mate, triggering a signal that would instantly be read. In principle the Affymetrix approach could be used to screen for tens of thousands of genes at a time. Geneticist David Burke of the University of Michigan is working on a DNA silicon chip that may be able to accomplish the same feat, but on a microscopic scale.
And in January, the Maryland-based OncorMed company announced commercial availability of a test for BRCA.1, the gene responsible for some types of breast cancer. The following month the company released a colon cancer genetic test.
Once a potentially troublesome gene is identified, the next logical step is gene therapy, a vague term that implies adding a missing or deficient gene, or removing a bad gene.
Five years ago, Drs. Michael Blaese, Steven Rosenberg and W. French Anderson began a series of pioneering gene therapy experiments at the National Institutes of Health, performed mostly on children who suffered from life-threatening genetic deficiency diseases. Their approach was to genetically engineer the children’s bone marrow cells, inserting the needed genes, and then reinfuse the altered cells back into the children’s bloodstreams. It hasn’t proven miraculous, but the procedure produced no deleterious side effects.
Since 1990, many other attempts at gene therapy have been pursued, either through laboratory genetic engineering of the patient’s DNA or via altered viruses or microscopic lipid capsules, both of which can theoretically carry needed genes into the human bloodstream. The potential benefits of gene therapy sent Wall Street to the buying floors during the early 1990s and prompted a frenzy of venture capital interests in biotechnology.
But last summer a large-scale review of progress in the field forced NIH director Dr. Harold Varmus to conclude that “there is still little or no evidence of therapeutic benefit in patients, or even in animal models.”
In August, Varmus ordered all the gene therapists at NIH back to their drawing boards, where the intellectual challenge of devising ways to supplement or alter human genes is to be rethought. And in December, a panel of experts appointed by Varmus issued a report that condemned most gene therapy efforts as “pure hype,” concluding that Wall Street and the public have been misled into believing that gene therapy was right around the corner. Not so, they said.
This after more than 567 Americans and dozens of Europeans had undergone some type of gene therapy in about a hundred different experiments. An entire gene therapy industry has developed since 1982, and 60% of all such experiments are conducted in the private sector. No one can say that gene therapy suffers for a lack of monetary and scientific support--on the contrary, the NIH has spent an average of $200 million a year on the technology since 1988 and it is estimated that the private sector’s spending has more than equaled that sum.
All those costly failures were directed at the conceptually easy task of adding a missing gene. Nobody has the foggiest idea how to change or remove a bad gene that is causing cancer or Alzheimer’s in an adult.
*
The easiest approach to gene therapy, from a biological point of view, is at the “the front end,” as some scientists put it, in a test tube-fertilized human egg before it is implanted in a woman’s uterus. Using pre-implantation diagnosis (PID), geneticists could screen pre-embryos for hundreds, even thousands, of traits ranging from diseases to eye and hair color. It would be relatively easy to either destroy those pre-embryos that carry undesired traits, or alter the genes. Whatever changes were made in the tiny one-to-eight-celled creature would be repeated in all its cells as the pre-embryo grew into a fetus.
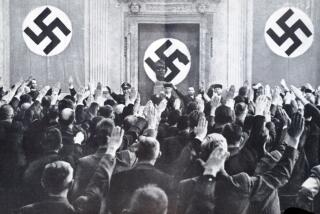
The approach, which is called germ line therapy, is so controversial that most scientists politely avoid its discussion. The Vatican and leading representatives of Islamic and Jewish religious groups have stated unequivocal objection to all forms of germ line therapy. And some prominent scientists, such as France’s Dr. Jacques Testart of the Institut Nationale de la Sante et de la Recherche Medicale in Clarmart, say that tolerating any form of PID would be tantamount to accepting widespread eugenics. For example, if current evidence for the existence of a gene for homosexuality bears fruit, how many would-be parents would order destruction or alteration of all pre-embryos that carried the trait?
Frances Collins, head of the genome project, Nobel laureate James Watson and other leaders of the genome effort have voiced concern or opposition to germ line therapy and PID. Hood, however, calls it “preventive medicine” and argues that it might well be morally acceptable within the proper legal and regulatory frameworks.
Another socially volatile approach to gene therapy involves modification of animal tissue for use in human beings. By altering pig DNA, it might be possible to engineer swine livers or hearts that could be transplanted into people without producing immune system rejection complications. People who suffer genetic hormone disorders might benefit from surgically implanted, genetically engineered animal pituitary, adrenal or ovarian tissues.
The Vatican and a host of social critics have argued that such modification and use of animal tissue is “unnatural,” even immoral. Animal rights activists, of course, oppose all such activities on principle.
Humanist Roger Straughan, of the University of Reading in England, argues, however, that given the existence of evolution and change in the animal world it is absurd to confine biomedicine to “species boundaries” and “species integrity.”
The boundaries have already been crossed, prompting creation of transgenic animals. Most such genetically engineered animals are mice or rats that had human genes of various kinds inserted into their genomes and counterpart rodent genes removed. For example, AIDS research has benefited greatly from creation of the SCID-hu mouse, an animal whose own rodent immune system has been genetically replaced with the human system. And cells from transgenic animals have been experimentally injected into people. To date, however, no one has received an organ transplant from a genetically modified animal.
While the bloom is temporarily off the gene therapy rose, even the technology’s harshest cynics believe the intellectual stumbling blocks that currently mire the field will be overcome within 20 to 30 years. Most encouraging, they say, is industry’s firm commitment.
“We stand at a crossroad, at which we can decide how much we want to control our future as a species,” Chiron CEO Dr. Edward Penhoet wrote in a recent statement from the Bay Area biotechnology firm. “As an optimist about human nature, I say we should take control of our destiny.”
*
No matter how great the corporate and NIH commitments to gene therapy, optimists say we are two decades away from viable modes of gene replacement or alteration, and the less sanguine put the timetable at 50 years.
That means a terrible gap will soon exist. It is already opening as disease-associated genes are rapidly discovered, and will be fully agape within five to seven years, when the human genome will be entirely sequenced. Suddenly humanity will know more about itself than ever before but will be temporarily helpless to alter its fate. Individually we will all have the opportunity--perhaps even mandate--to be tested for a range of genetic traits and disorders but our physicians will have little, short of exercise and dietary recommendations, to offer.
We will witness our fates, impotent to alter their courses.
“Mostly what each of us for a generation or two of Americans will be finding out will be bad news,” says Dr. George Annas. “Do you really want to know your genome?”
As chair of the Health and Law Department of Boston University, Annas has served on a variety of Human Genome Project ethics and advisory committees. Even before the sequencing project was formally underway, Annas was one of the ethicists most influential in convincing James Watson, then head of the human genome drive, to direct about $3 million a year of the effort’s monies toward study of its legal, social and ethical impacts. ELSI, or Ethical, Legal and Social Implications of Human Genome Research, was born along with the rest of the project and has since spawned an enormous amount of hand-wringing and debate. It is an unprecedented entity in the annals of Science: It funds, in the main, humanists and attorneys to analyze the potential impact of a scientific revolution before it occurs.
By far the biggest immediate concern is how humanity will deal with the coming tsunami of genetic information during the decades-long gap period in which therapeutic options will be limited or nonexistent. The more ELSI participants consider the matter the larger the list of concerns grows. And every day more scientists and physicians add their voices to the chorus of worry.
“I’m basically in favor of the genome project, but I think it needs strict legal constrictions,” Annas says. “I buy the argument that we may learn something that will help people, find cures for diseases and so on. And that’s the only upside. There’s enough serious scientific background here to say there are some possibilities.”
But in the absence of cures and correctives, Annas predicts, “Mostly we’re going to look at these genes and see how we’re different from one another, rather than say we’re all in one family.”
Your genes give you Alzheimer’s, but--thank God--mine don’t. I have genes for aggression. Your genes make you passive. Those people (fill in the ethnic blank) all have genes that make them (fill in the stereotyped trait). In a world already stratified and rife with ethnic and gender tensions, Annas fears that genetic information will simply add to the name-calling noise.
New York University sociologist Dorothy Nelkin, who has also been a major player in ELSI, asks the same basic question: “Why do we want to know this kind of information? The DNA mystique--why are we so willing to accept this?”
From Nelkin’s perspective few, if any, of the most fundamental questions about human behavior will ever be answerable based on genes alone. Yet interest in predictive behavior--particularly for antisocial and violent traits--is strong. Though psychiatrists today generally say that key behaviors result from a mix of genetic and environmental factors, few adhere to the neo-Freudian view that the nature of the family environment is absolutely paramount in determining a child’s behavior as an adult. In the early 20th century, if a father and son both exhibited violent tempers and heavy bouts of alcoholism, observers would shrug and say, “Like father, like son.” It was the street-smart way of indicating that the son was brought up to behave like his rotten father. As the 21st century approaches, however, psychiatrists are far more likely to assume that the father and son exhibit the same antisocial behavior because they share an identical constellation of pertinent behavioral genes.
The search is on, with considerable apparent success, for genes that dictate teenage malaise, seasonal depressions, schizophrenia, borderline personality disorder, aggressiveness, passivity, bipolar disorder, depression, mania, alcoholism and addictive personality disorder, altruism, dominance and a host of other factors that ultimately determine not only how each of us behaves on an individual level, but how we interact and coexist as a society.
“We’ll never be able to predict personality or behavior. The risks and factors involved are just too complex,” Nelkin argues. But she suspects that genes linked to key behaviors will be targets for individual testing.
“It’s associated with the larger societal issue of blaming the individual,” Nelkin insists. “Rather than blaming the collective response or government or the state. If you’re sick, it’s your fault. So you now see Gallo wine sponsoring research on the genetics of alcoholism, for example.”
Individually genetic information holds plenty of pitfalls, critics say, but they underscore that the issue goes well beyond the individual. If you carry the BRCA.1 gene thought to be associated with breast cancer or the Xq28 gene that seems to be linked to homosexuality, in all likelihood the genes are also present in one or more of your siblings, parents, children and cousins. Your genome data isn’t just yours.
For doctors and counselors this creates an enormous confusion, and possible conflicts with the Hippocratic Oath.
“Who is the patient?” Nelkin asks. “Who should be informed? If they find a deleterious gene in their patients, do they [doctors] have a duty to inform family members? Just who, in fact, is the patient?”
The doctor is in a no-win situation, Annas says. Consider the example of a 25-year-old woman who carries a combination of genes that give her 90% odds of developing malignant breast cancer before she reaches menopause. In all likelihood, she would have asked to be tested because several of her female relatives had succumbed to the disease. It would seem prudent for the physician to contact the woman’s sisters and mother immediately, suggesting that they also undergo testing. But by doing so the doctor violates the patient’s rights to confidentiality and privacy.
*
Few issues are as thorny for ELSI participants as privacy and personal control over one’s genetic information.
“Who has the right to decode your genome?” Annas asks. “What can they do with it?”
Putting aside genome data, hospitals and health insurance companies already possess an enormous amount of medical information on everyone reading this article. Increasingly your medical information is finding its way onto the all-too-leak-prone Internet in the form of interstate transferal of clinical and experimental files. Addressing hearings of the Congressional Subcommittee on Government Information in 1991, James Watson concluded, “the idea that there will be a huge databank of genetic information on millions of people is repulsive.”
Annas believes that the confluence of genetics and psychiatry has led to a point wherein, “the stage is set for an explosion of DNA databanks for criminal law purposes.”
He calls an individual’s genome a “future diary,” and insists it is deserving of as much legal and moral protection as the private entries a troubled teen makes in a notebook.
Noted molecular biologist Maxine Singer, president of the Carnegie Institute in Washington, D.C., warns that “we’re dealing with something that affects every life on the planet. We are all affected by DNA molecules.” Thus we all stand to lose a great deal if our private DNA becomes the subject of public discussion.
Last year, ELSI came up with the Genetic Privacy Act, which Annas and other advocates hope will gain support in Congress. The act prohibits analysis of DNA samples without the written approval of the individual from whom the DNA was extracted. It also states who shall have a right to see or collect that data, gives an individual the right to order destruction of all samples of that person’s genetic database or DNA samples and grants individuals permission to deny use of their genes for research purposes.
Congress is currently debating a bill, called the Medical Records Confidentiality Act, that seeks to limit the numbers of individuals who can have access to medical information. Testimony before the Senate Labor and Human Resources Committee last November revealed thousands of abuses of individual privacy, violations of doctor/patient confidentiality and medical databases. The act seeks to limit and control the numbers of databases that can obtain and store personal medical records. Annas and other critics charge that the act will result in even larger, more efficient medical databases run by private companies.
Among the largest existing databases are those used by huge health maintenance organizations (HMOs) and companies that sell their information to insurance companies. Some genetic information is already in those commercial databases, and individuals who carry traits for ailments such as sickle cell anemia and Huntington’s disease have suffered insurance, job and health-care discrimination as an outcome of electronic distribution of their test results.
In a special 1993 report, an ELSI task force on health insurance concluded: “One of the ironies in the current health care coverage crisis is that developing more accurate biomedical information could make things worse rather than better . . . the likelihood of needing health care and the ability to obtain coverage for that care has the unfortunate result that those most in need may have the greatest difficulty finding affordable health care coverage. New advances in human genetics are transforming medicine by making available increasing amounts of such information about risk.”
The ELSI report concluded that strong federal legal instruments were crucial to preventing “the unwelcome possibility of genetic discrimination.” Twelve states, including California, have enacted laws that aim at limiting insurance company access to genetic information, according to Karen Rothenberg, director of the Law and Health Program of the University of Maryland School of Law in Baltimore. But the state laws vary dramatically and none can touch the borderless world of cyberspace, wherein every entry instantaneously crosses state lines to become nationally--even internationally--accessible.
*
As 1995 came to a close, two genetic privacy acts were introduced in Congress. One, sponsored by Oregon Republican Sen. Mark Hatfield, would eliminate all but forensic use of genetic information without written consent. Democratic Rep. Louise Slaughter of New York has introduced another bill on the House side that would specifically prohibit insurance companies from having access to or using personal genetic information. Given Congress’ crowded schedule, neither bill is expected to reach the floor for debate until this fall or early next year unless championed by Speaker Newt Gingrich. To date, Gingrich has made no public comments on genetic privacy issues.
Dr. Thomas Murray of Case Western Reserve Medical School in Cleveland chaired the ELSI investigation on health insurance. He says that individuals, often at the encouragement of their physicians or genetic counselors, are already submitting to gene tests under false names in order to protect themselves from insurance discrimination. Providers who deal with breast cancer, Huntington’s and other disorders for which gene tests are now available are encouraging their patients to pay for testing in cash in order to avoid a paper trail that might turn up in a computer database.
“Lest anybody think this is my imagination, I should say that people are literally knocking on my door almost every day with such stories,” Murray said in a speech last year to the American Association for the Advancement of Science. In the absence of universal health-care coverage, he predicted, the insurance industry notion of “actuarial fairness” will virtually compel use of genetic information.
“Insurers don’t want to write insurance on a house that’s already burning,” Murray explained. “Actuarial fairness says that people ought to pay into the system according to what they expect to receive. To not do so would be unfair to those whose houses aren’t on fire.”
In the medical context it is fraudulent to gain low-cost private health insurance by lying about a preexisting condition, such as heart disease or cancer. Today, says health insurance industry spokesman Harvie Raymond, no company is requiring genetic tests of its applicants or clients.
“But some are requesting information on those tests that have been performed,” Raymond, of the Health Insurance Association of America, said. “They are universally concerned about being able to have results of genetic tests available, just as would be the case with any other medical information . . . The insurance industry would say that if that kind of information is taken off the table . . . a fair and equitable assessment of risk will not be able to be made, and fair pricing cannot be made.”
More than half of all insured Americans are covered through their employers, so individual health risks are not raised directly by insurance providers. But increasingly employers are screening potential employees for health tendencies that might make their care costly in the future. Annas and Nelkin think that, without legal prohibition, genetic screening could one day be employment-based.
Raymond says that in the absence of a national health-care system there is no easy way to satisfy the needs of both societal justice and actuarial fairness.
“We don’t really, as a nation, have a solution,” he says.
The thorny issues of discrimination and the structure of American health care are the only issues that give Human Genome Project cheerleader Lee Hood pause. As humanity teeters on the brink of a dramatic biomedical revolution, he says, the entire effort hinges on the mundane realities of how people get health care, who pays for it and who subsidizes innovative medicine.
“Who’s going to pay for the next step, taking all this genetic information and translating it into gene therapy or some other kind of medical benefit?” Hood asks. “It’s a never-never land right now. We have great teaching hospitals shaking their heads and saying, ‘Where are we supposed to go?’ ”
Revolutions are never easy. By the time Americans ring in the 21st century, most, if not all, of our essential DNA will have been sequenced. And if we haven’t taken action before, we will then be collectively and individually compelled to confront the question of just what we want to do with our newfound knowledge.